
Neuroanatomy & Psychiatric Disorders - prereading
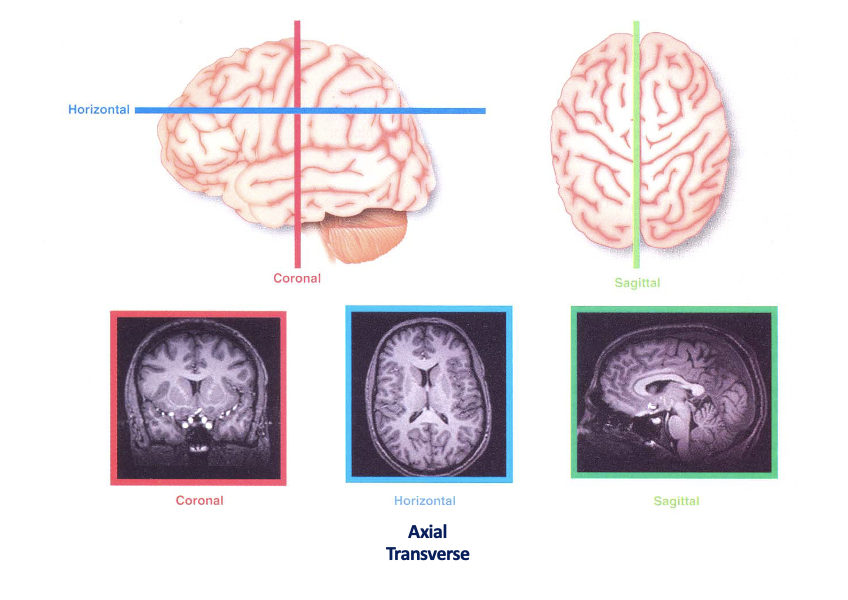
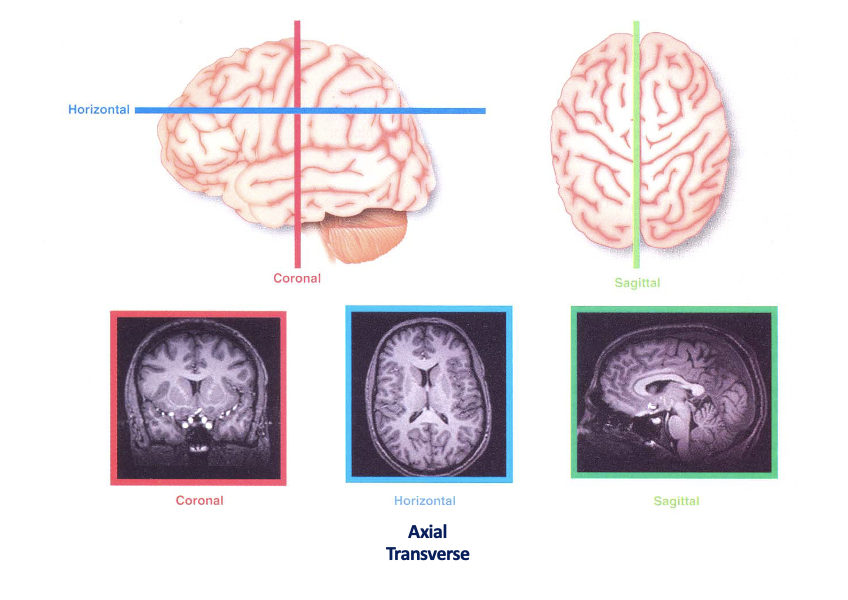
Planes of the brain
White matter": Mainly axons due to myelination (lipid/ fatty sheath)
Grey matter: neuronal cell bodies
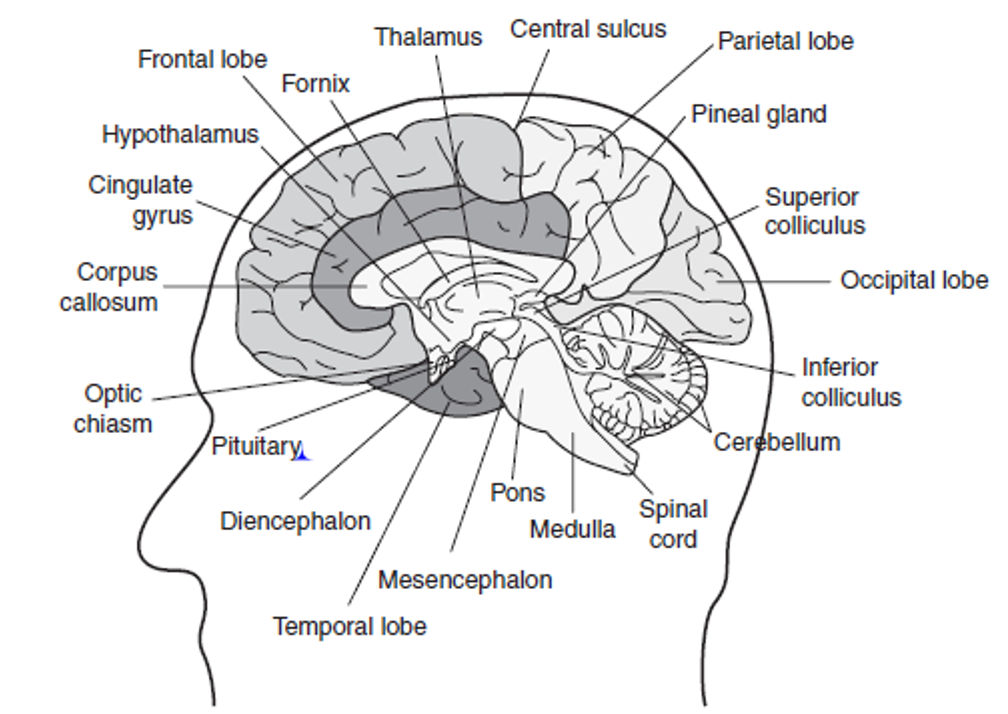
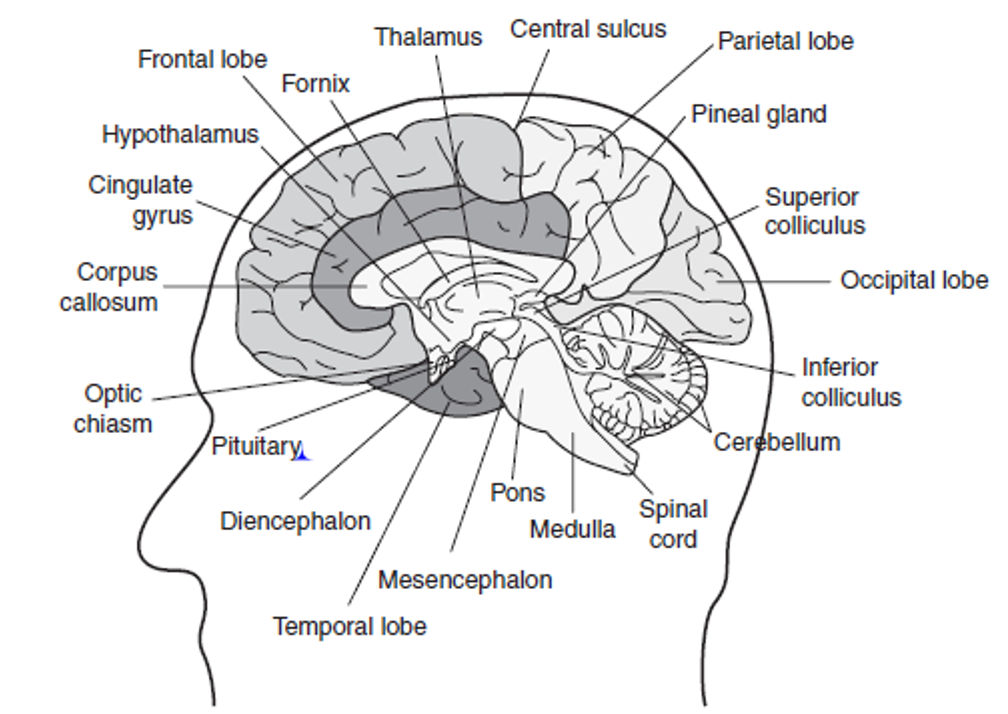
Main regions of the brian
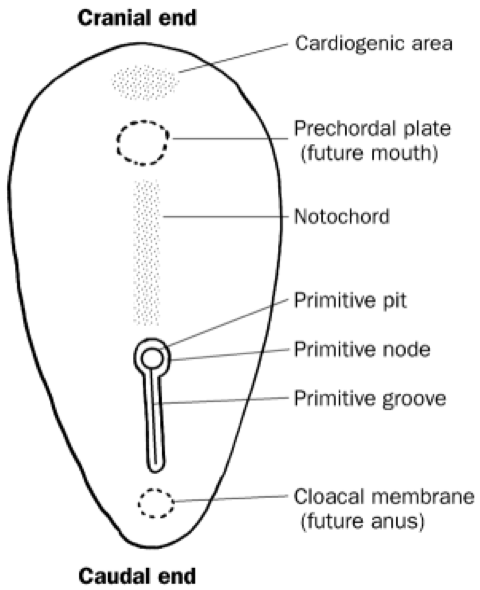
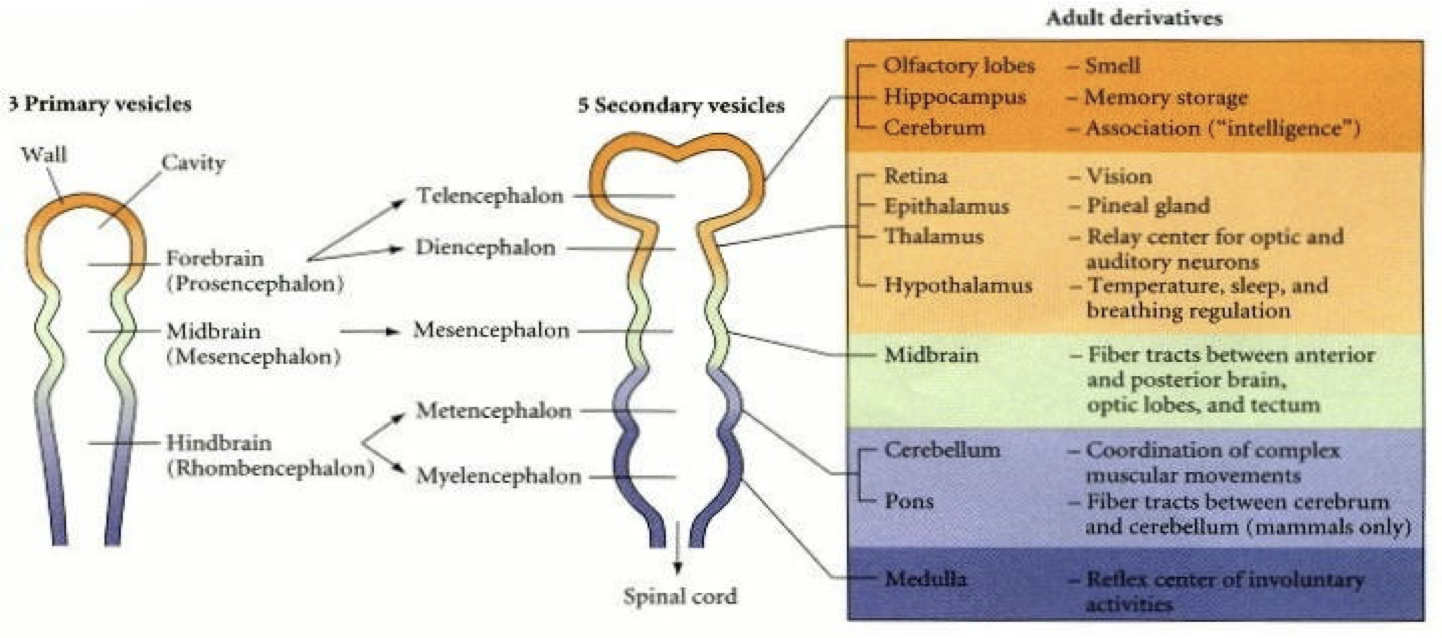
Embryology
Refer back to case 7 embryology on the formation of the spinal cord
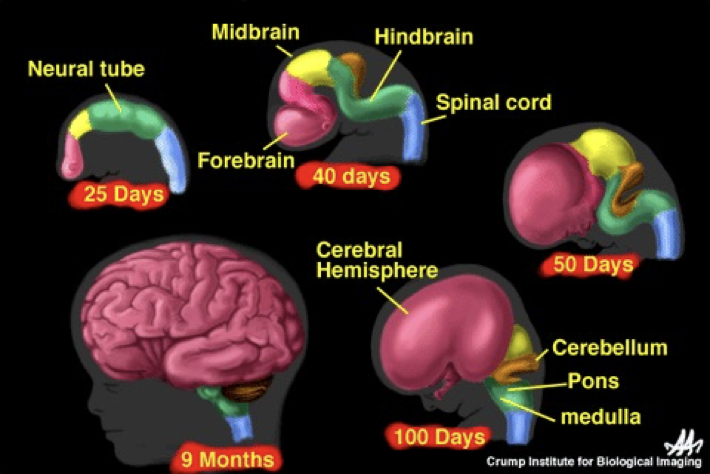
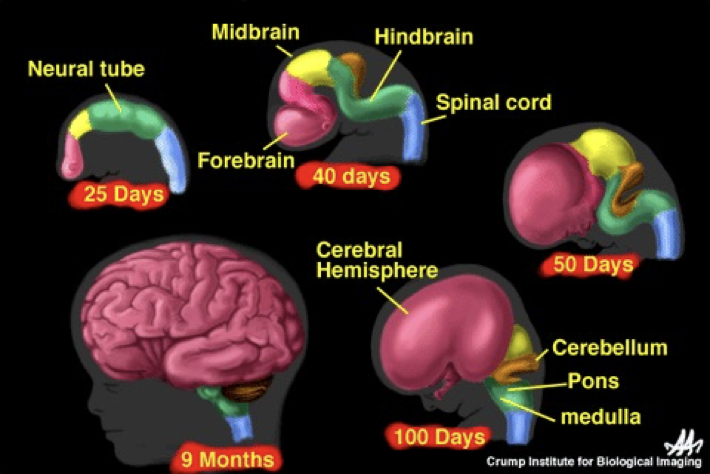
The neural tube then splits into the main parts of the brain
Rhombencephalon
Brain stem
Cranial nerves + normal nerves run from the medulla
The cerebellum + pons are important in co-ordinating movements + responding to external stimuli
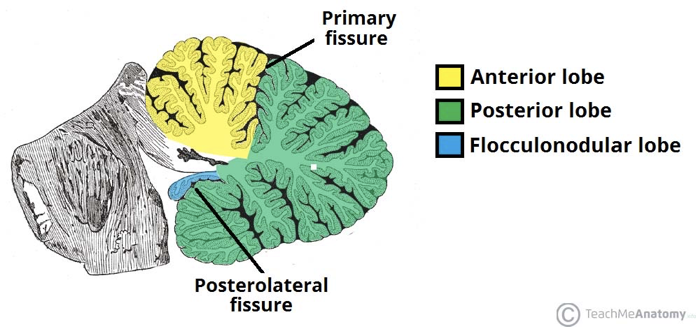
Cerebellum - divided i nto 3 lobes:
Flocculonodular lobe
Vestibulocerebellum/ archicerebellum
Regulates balance + co-ordination (oldest)
Posterior lobe
Anterior lobe
Contains Purkinjie + granule cells
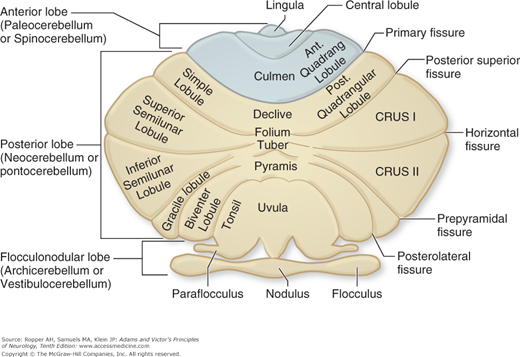
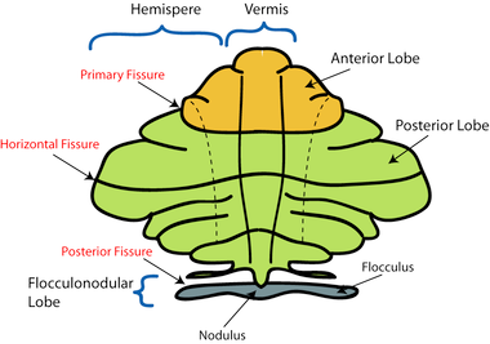
Areas closest to the vermis- spinocerebellum/ paleocerebellum
Spinocerebellum: regulates body temperature + limb movement
Laterally- neocerebellum
Neocerebellum:
regulates planning,
sensory movement for action
Cerebellar Disorders
Damage of the neocerebellum causes ataxic gait e.g. stroke or alcohol-related
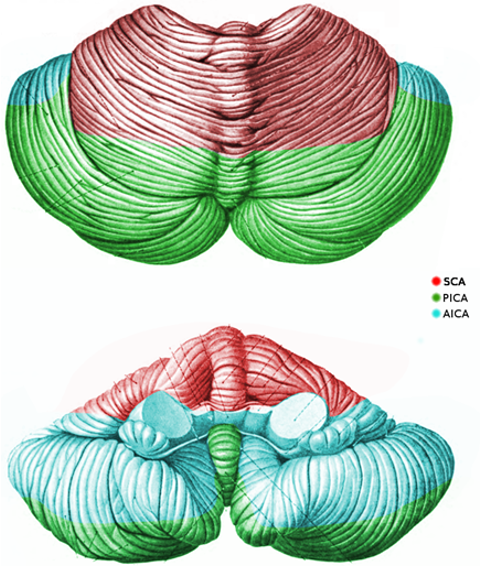
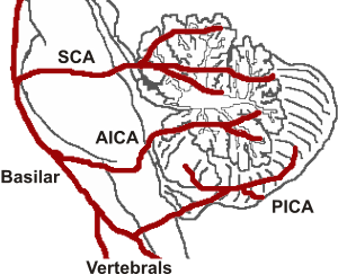
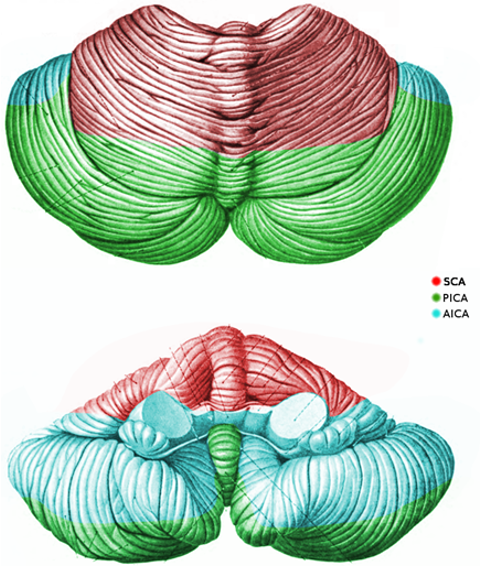
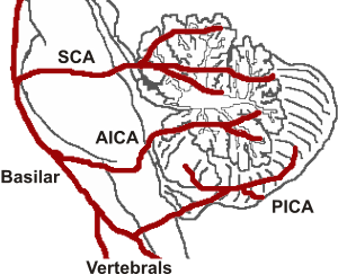
Cerebellum has a complex arterial supply
Therefore, it is important in cases of stroke or vertebral/ basilar artery dissection (present with cerebellar signs
Pontine disorders
locked-in syndrome
Central pontine myelinolysis
Progressive Supranuclear Palsy (Steele-Richardson-Olszewski):
Supranuclear ophthalmoplegia
Neck dystonia
Parkinsonism
Pseudobulbar palsy
Behavioural impairment
Imbalance
Frequently falls
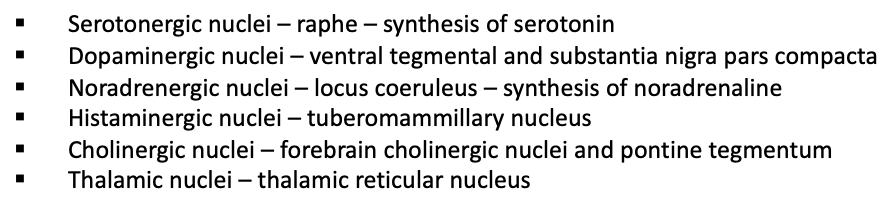
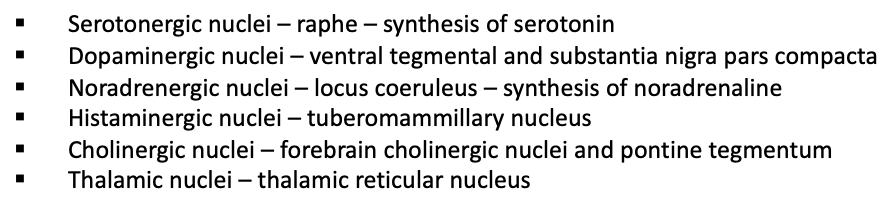
Reticular formation
Allows for communication of the brain to the rest of the body
A hub for the synthesis of neurotransmitters and wake/sleep state
Ascending/ descending through the brainstem
Includes ascending reticular activating system- role in arousal
Mesencephalon
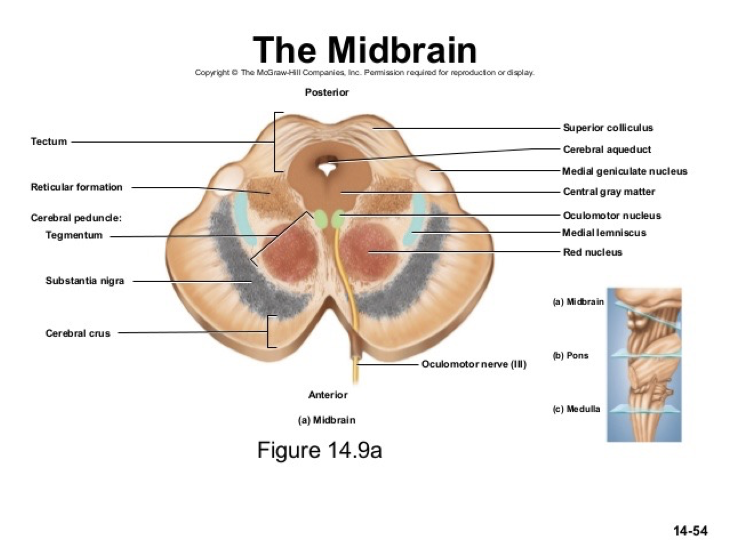
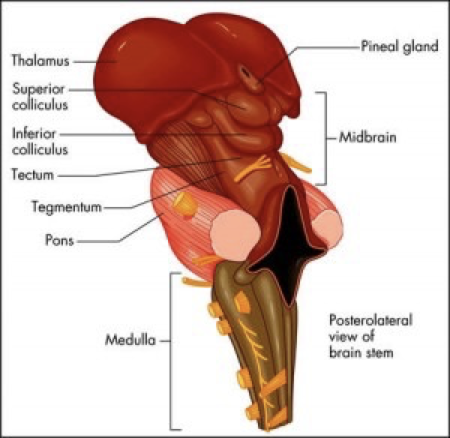
Midbrain
Acts as a connector between different parts of the brain
links everything together
Don’t worry too much about the next info
Parts of the midbrain
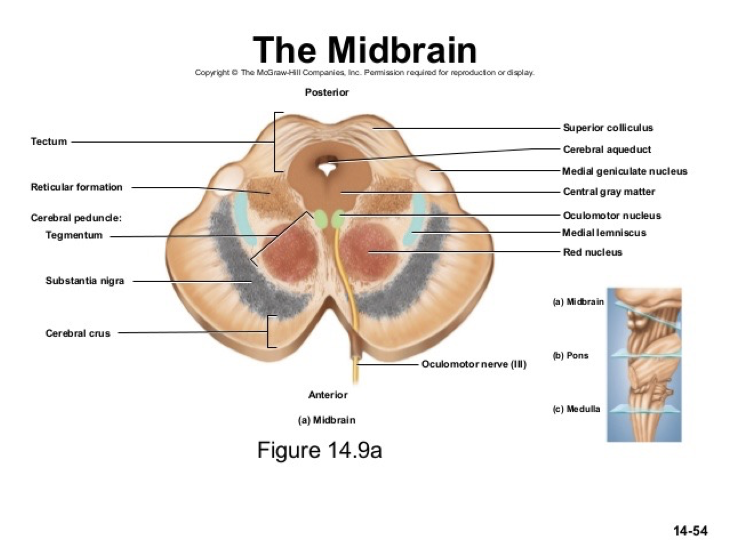
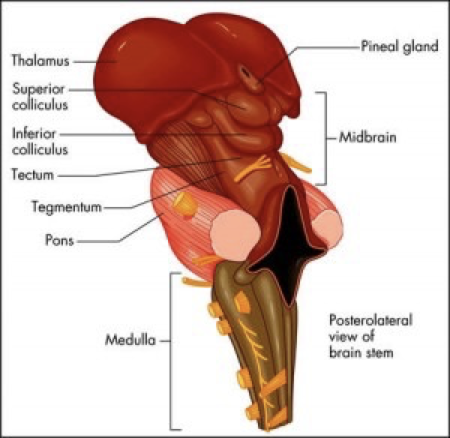
Tectum (dorsal part) splits into:
Superior colliculus- visual processing + eye movement control
Inferior colliculus- auditory processing
![]()
Disorders of the mesencephalon
Parkinson’s - reduction in dopaminergic neurones in substantia nigra
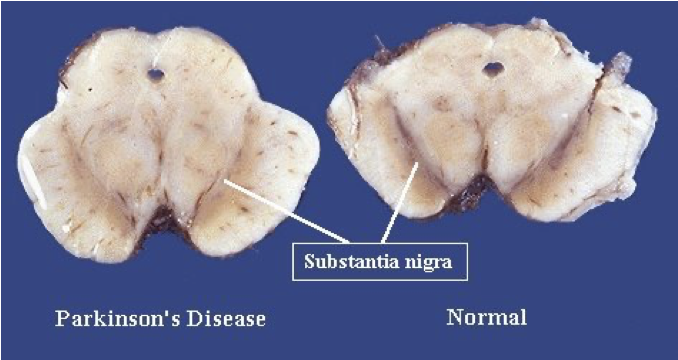
Schizophrenia- increased dopamine in substantia nigra
Multi-system atrophy- degeneration of striatum and substantia nigra
Ventral tegmental area- primary sites of addictive drugs (heroin, cocaine, alcohol, nicotine)
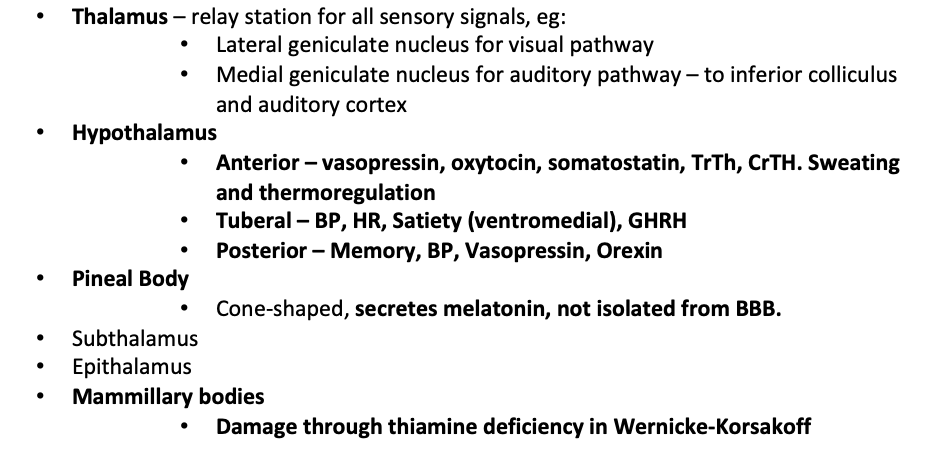
Diencephalon
Contains:
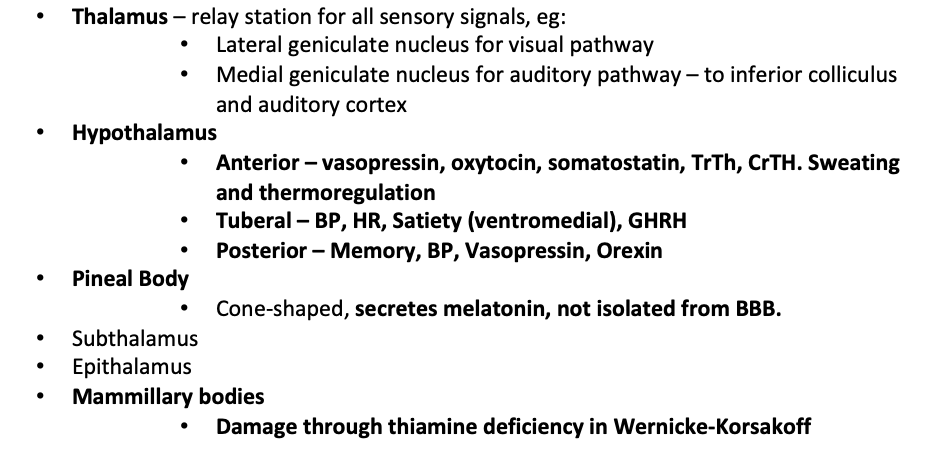
Thalamus
Hypothalamus
Pineal Body
Subthalamus
Epithalamus
Mammillary bodies
Limbic system:
Connects cortical control to memory / sensory/ secretory areas
Involved in motivation, visceral processes + rewards
Systems of emotions
Connects a group of structures surrounding the brainstem (cingulate gyrus, hippocampus, hypothalamus + anterior thalamic nuclei)
Connecting these structures enables cortical control of emotion + plays a role in storing memory
Telencephalon
higher functions such as smell, memory + Intelligence
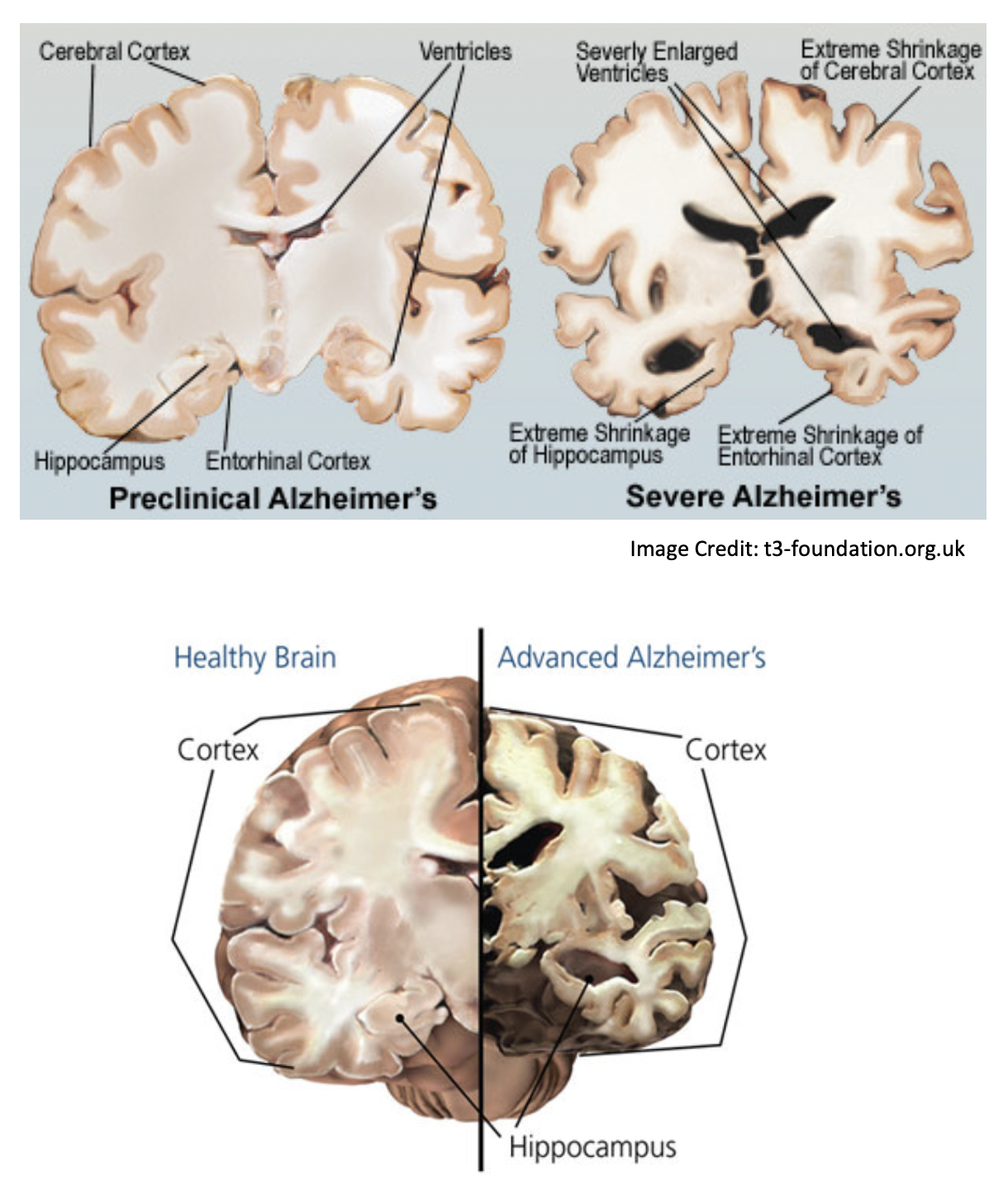
Hippocampus
Medial temporal lobe
Short-term memory to long term memory
Spatial memory
Includes dentate gyrus + granule cells - formation of new episodic memories, site of neurogenesis, affected in depression
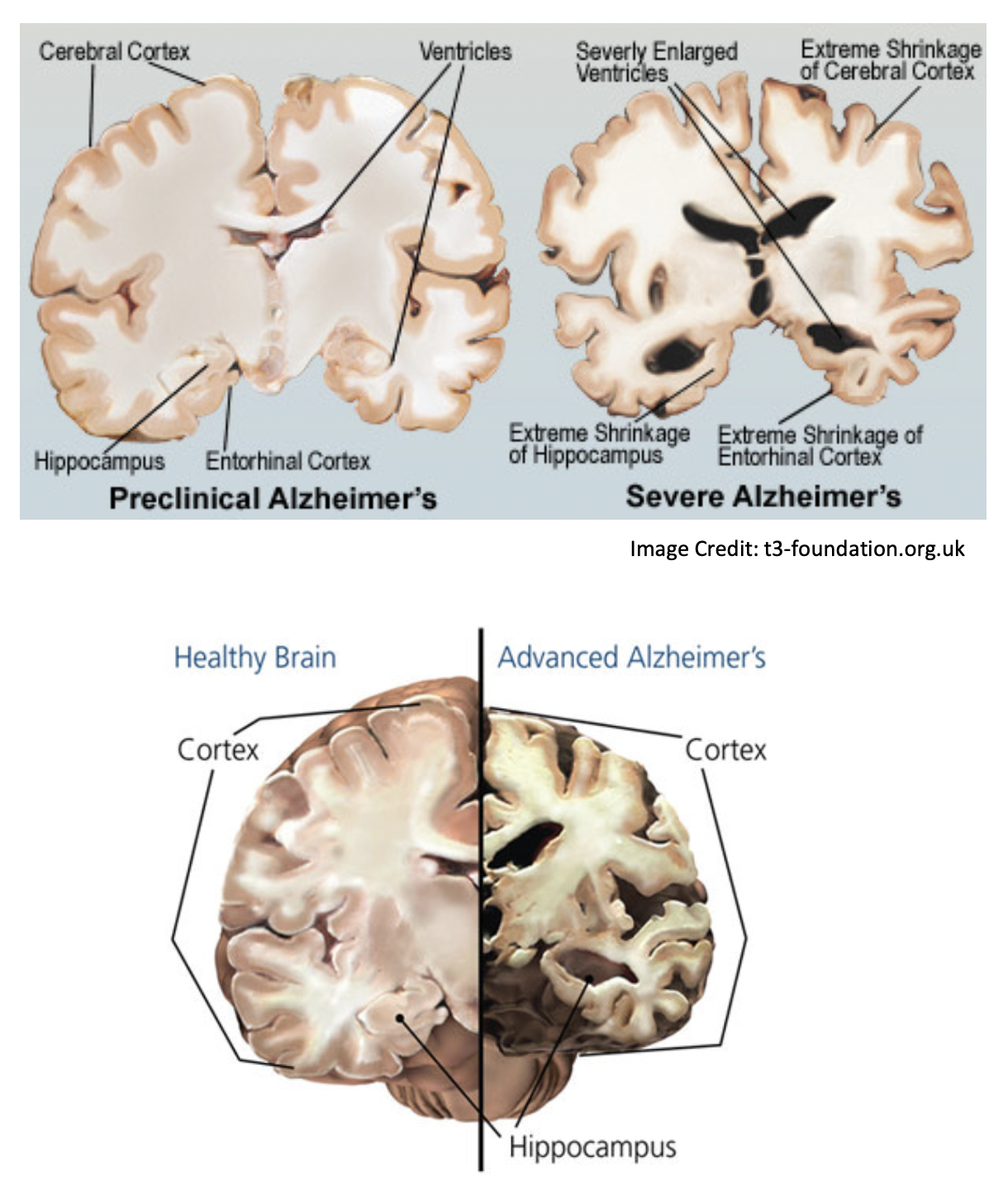
Alzheimer’s + dementia → hippocampal atrophy → memory symptoms
Cortex
Memory
attention
Cognition
awareness
thought
language
consciousness
4 lobes, gyrus (fold) + sulcus
Frontal lobe
Superior frontal gyrus = self-awareness/ laughter
Middle frontal gyrus
Inferior frontal gyrus = language processing, Broca’s area
Medial frontal gyrus = executive mechanism
Paraolfactory area= limbic
Orbitofrontal cortex= stimulus-reward, stimulus/outcome, addiction
Ventromedial prefrontal cortex- decision making, emotion regulation, addiction
frontotemporal dementia/ Pick’s disease = genetic + accumulation of tau + frontal symptoms
Prefrontal cortex
Planning + executing actions
One of the last to develop
lesions:
Dramatic changes in personality
Loss of spontaneity/ problems with initiating speech/ movements
inability to make + carry out sequences of actions/plans
Parietal lobe
Integrates sensory information
Dominant hemisphere lesions:
Dysphasia, aphasia
Dyscalculia- difficulty learning, doing calculations
Dyslexia
Apraxia- ability to execute or carry out skilled movements and gestures, despite having the desire and the physical ability to perform them.
Agnosia- inability to recognize and identify objects or persons.
Gerstmann syndrome- Dyscalculia, Dysphasia, finger agnosia, LR disorientation
Non- dominant hemisphere lesions:
Spatial disorientation
Constructional apraxia
Dressing apraxia
anosognosia- unaware of their own health problems
Temporal lobe
Transeverse temporal gyri - Heschl’s gyri
Superior temporal gyrus= auditory context with TTG. Pricess perception of sound + apply comprehension.
Posterior STG = wernicke’s area
Middle temporal gyrus
Fusiform gyrus = FACIAL RECOGNITION, synaesthesia, dyslexia, prosopagnosia
Inferior temporal gyrus= visual object recognition
Occipital lobe
Lingual gyrus
role in vision + dreaming
Visuo-limbic integration
encoding complex images
word processing
Cuneus - basic visual processing
Calcarine sulcus/fissure
primary visual cortex
takes signals from geniculate nucleus via thalamus
Tracts- only for reference
Arcuate fasciculus- links Broca’s + Wernicks area
Uncinate fasciculus
Links temporal inferior frontal gyrus + frontal lobe
Hippocampus + amygdala with orbitofrontal cortex
implicated in several psych conditions
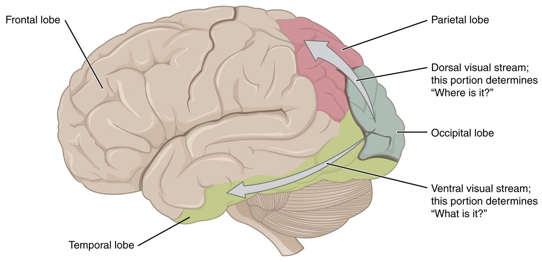
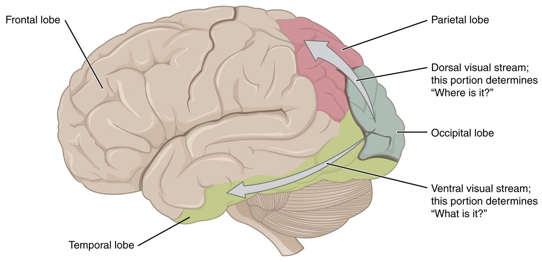
2 visual streams hypothesis:
dorsal - where?
ventral- what?
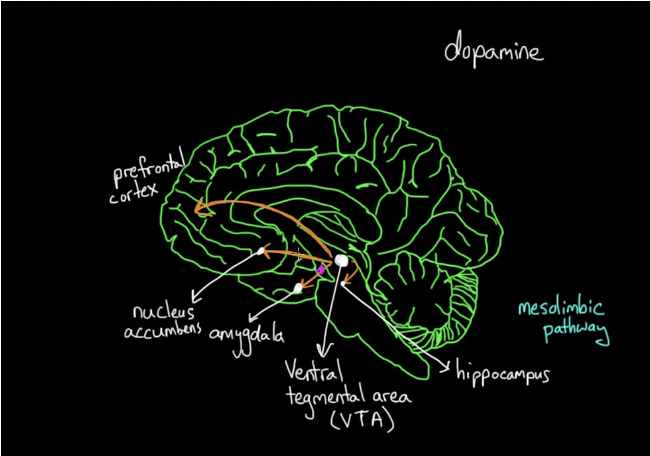
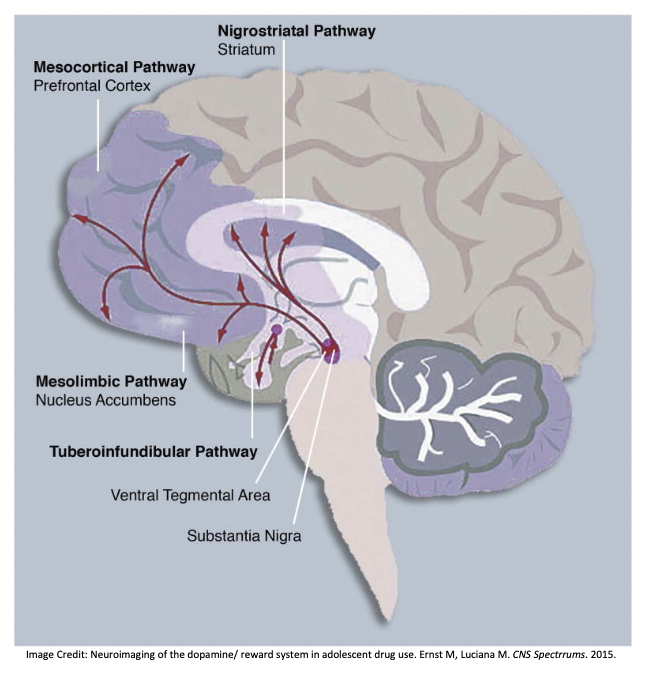
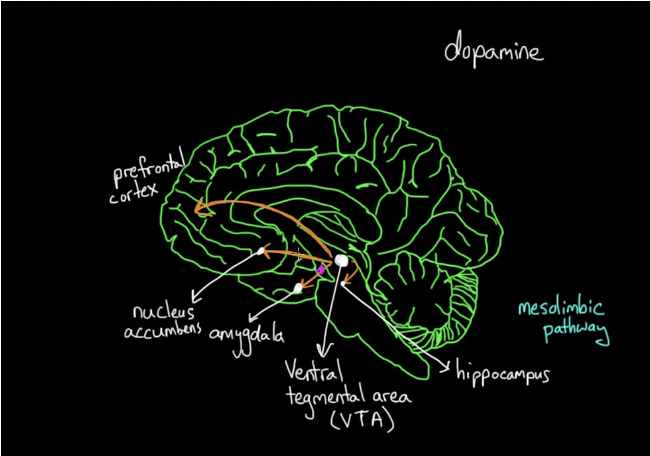
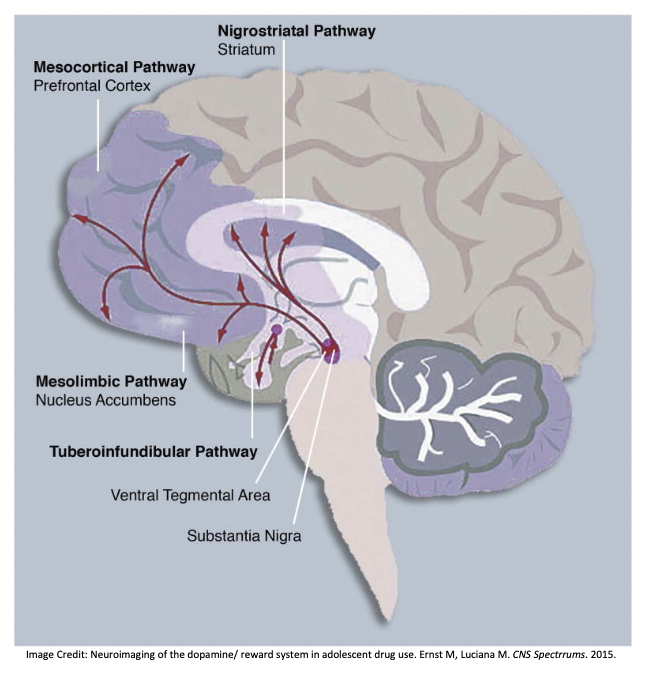
Central dopamine hypothesis
Meso-cortical pathway
Meso-limbic pathway
Nigrostriatal pathway
Affected in schizophrenia + other psych disorders
Medications for scz work on this pathway
Side effects of these meds are linked to these pathways (e.g. cog-wheel rigidity like that seen in parkinson’s/ galactorrhea due to pituitary stimulation)
Alzheimer’s Dementia
Microscopic accumulations of peptide amyloid-β – plaques → cause loss of synapses, then neurons.
Progressive degeneration
Early changes in the hippocampus (first to be damaged)
Generalised shrinking and enlarged ventricles follow
In severe depression, the dentate gyrus don’t light up in the scans which means they don’t form many memories.
Drug misuse
The reward system is based on dopamine.
It activates all dopamine pathways, particularly the mesolimbic pathway.
Dopamine is produced in the Vental Tegmental Area (VTA).
The mesolimbic pathway links this to the Nucleus Accumbens (motivation/ reward).
If we do something good, or use an addictive drug, this pathway is stimulated.
The mesocortical pathway is also activated.
This links to the Prefrontal Cortex (PFC).
This changes how you prioritise and plan.
Disorders
Case 1- depression after frontal tumour
56 year old female
Progressive apathy
Social withdrawal
Poor self-care for part 3 years
Admitted to a psychiatric facility for depression
unresponsive to antidepressants so CT was conducted
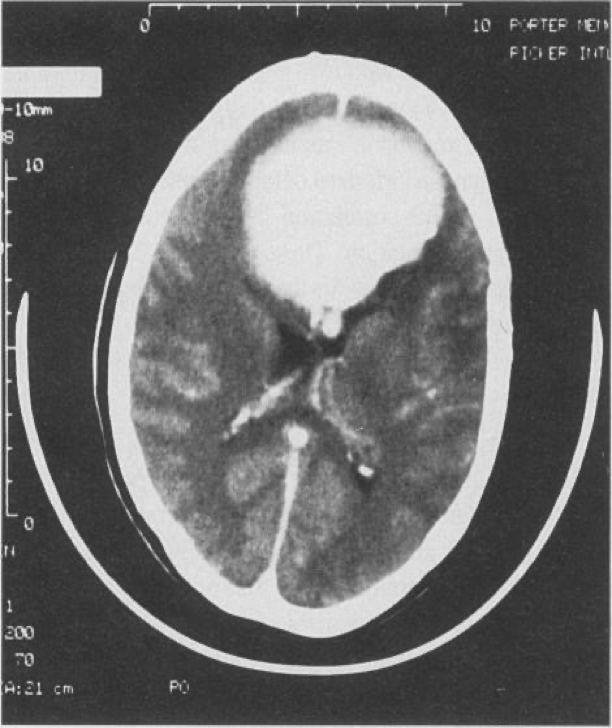
8cm medial bifrontal mass
Total excision benign transitional-type meningioma → rapid improvement
4 months after the operation was cheerful + motivated
Case 2- Psychosis after temporal tumour
18-year-old female
Referred form school to a psychosis clinic (high risk)
2 years of withdrawal from social activities + resent from work groups or talking in public
1 year later became concerned about unknown people stating + laughing at her for no reason
Feeling the world around her has changed
She is concerned that people are intimidating her + that there are special messages in TV for her
She is neurologically normal + an average IQ
Initial diagnosis: prodromal syndrome of schizophrenia but symptoms became more rapidly severe
Routine MRI conducted
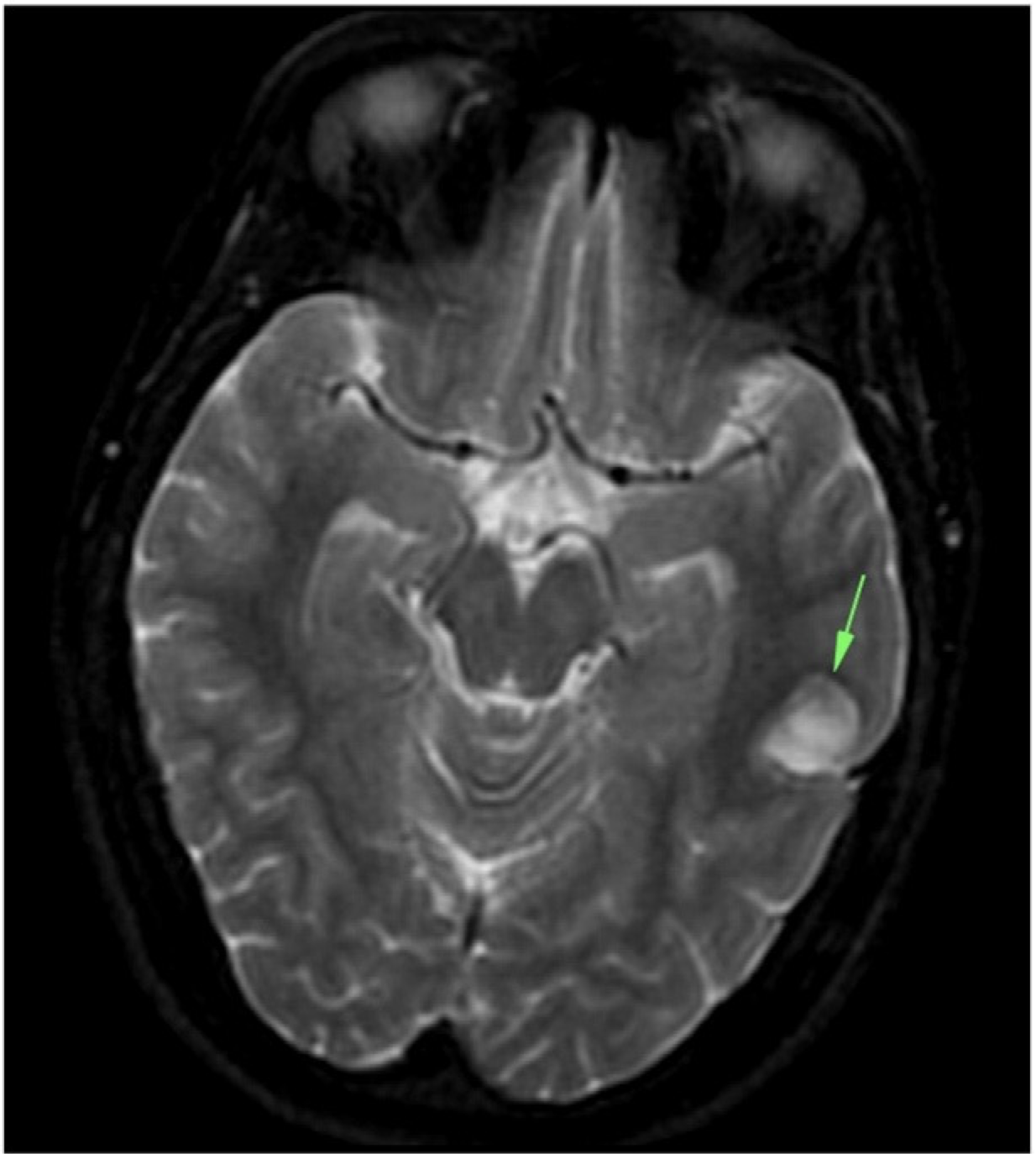
Tumour in the left temporal lobe - dysembryoplastic neuroepithelial tumour (DNET)- usually benign glial neural neoplasm
Surgically remove
Psychotic symptoms improved with the help of other treatments- risperidone + CBT
However, remained socially withdrawn
Case 3- bipolar effective disorder due to Wilsons disease
Middle aged female
Detained + admitted under section 2 of the Mental Health Act (MHA) 2007- decline in her mental state
Initially aggressive behaviour + required restrain by the Emergency Department security + police
Quietly spoken
voicing paranoid persecutory delusions
euthymic with labile affect
alternating between anger
tearfulness
displaying disinhibited affection
Doesn’t know why she was presented
CT

Hypodensity in the putamen, worse on the left
No mass, infarct or infectious process to explain the lesions
Consistent with the MRI from a couple of months ago which demonstrates hyperintensity of both putamina
Associated with Wilson’s disease
final diagnosis: psychosis secondary to neurological Wilson’s Disease
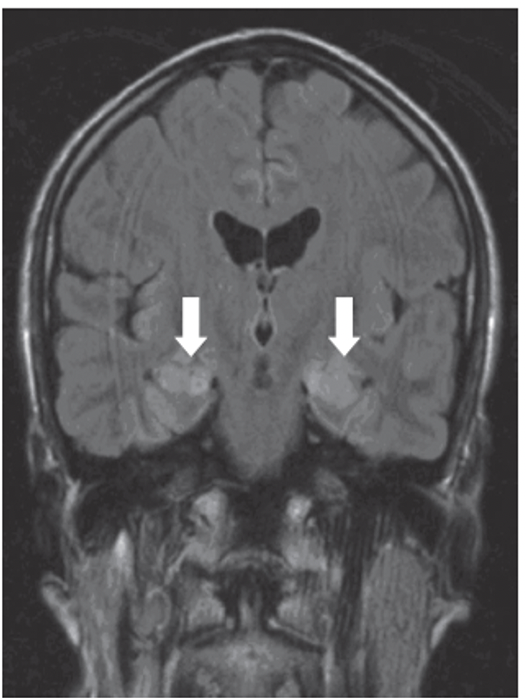
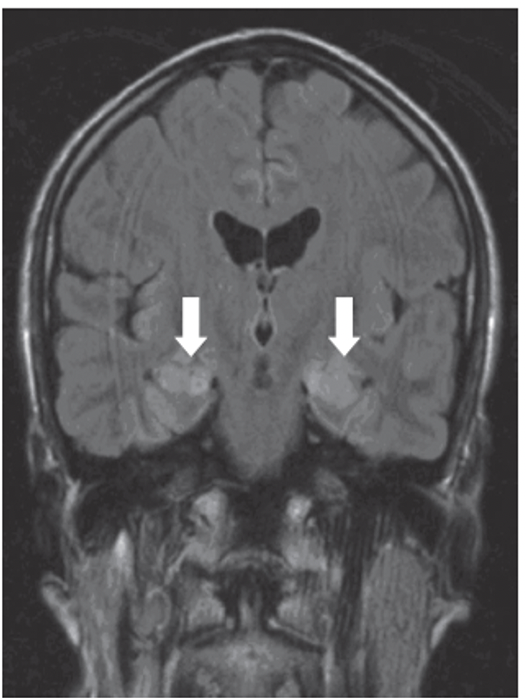
Case 4- Psychiatric syndromes associated with neurological disease
63-year-old male
paranoia
impaired anterograde memory + fatigue
FLAIR scan shows bilateral hyperintensities in the hippocampus (arrows) → shows inflammatory process
Blood tests revealed anti-voltage gated potassium channel antibodies
Neuroanatomy & Psychiatric Disorders - prereading
Planes of the brain
White matter": Mainly axons due to myelination (lipid/ fatty sheath)
Grey matter: neuronal cell bodies
Main regions of the brian
Embryology
Refer back to case 7 embryology on the formation of the spinal cord
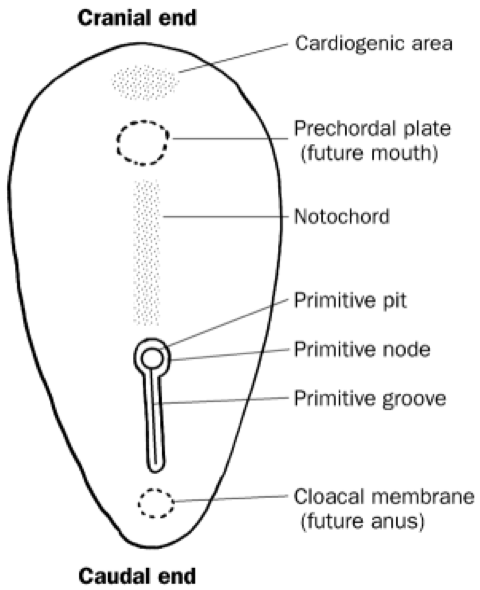
The neural tube then splits into the main parts of the brain
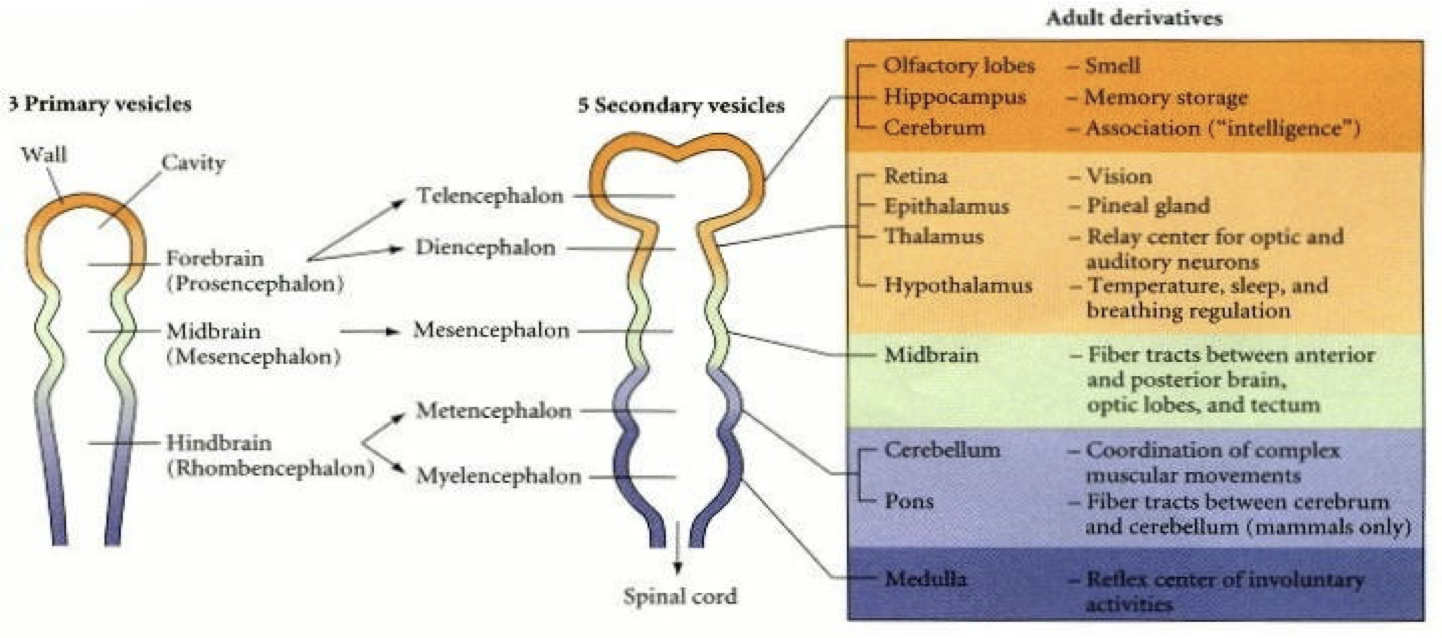
Rhombencephalon
Brain stem
Cranial nerves + normal nerves run from the medulla
The cerebellum + pons are important in co-ordinating movements + responding to external stimuli
Cerebellum - divided i nto 3 lobes:
Flocculonodular lobe
Vestibulocerebellum/ archicerebellum
Regulates balance + co-ordination (oldest)
Posterior lobe
Anterior lobe
Contains Purkinjie + granule cells
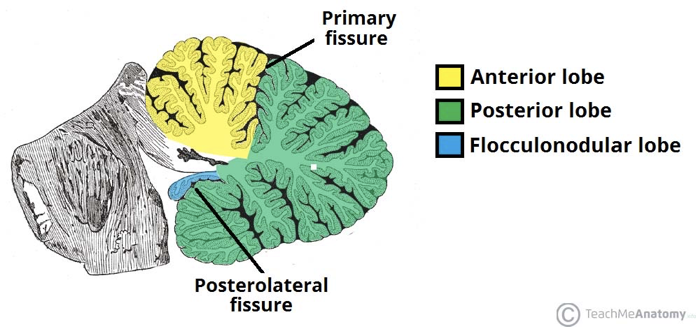
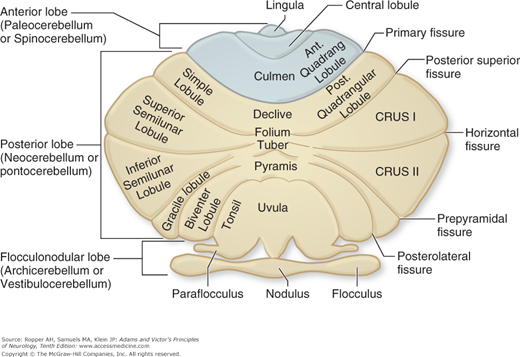
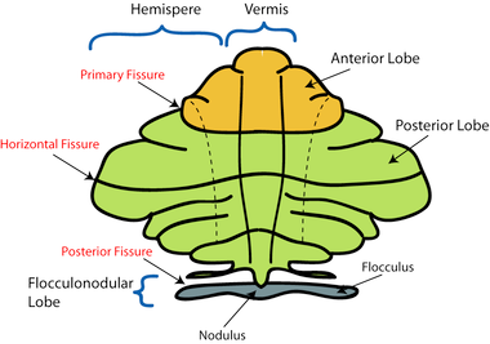
Areas closest to the vermis- spinocerebellum/ paleocerebellum
Spinocerebellum: regulates body temperature + limb movement
Laterally- neocerebellum
Neocerebellum:
regulates planning,
sensory movement for action
Cerebellar Disorders
Damage of the neocerebellum causes ataxic gait e.g. stroke or alcohol-related
Cerebellum has a complex arterial supply
Therefore, it is important in cases of stroke or vertebral/ basilar artery dissection (present with cerebellar signs
Pontine disorders
locked-in syndrome
Central pontine myelinolysis
Progressive Supranuclear Palsy (Steele-Richardson-Olszewski):
Supranuclear ophthalmoplegia
Neck dystonia
Parkinsonism
Pseudobulbar palsy
Behavioural impairment
Imbalance
Frequently falls
Reticular formation
Allows for communication of the brain to the rest of the body
A hub for the synthesis of neurotransmitters and wake/sleep state
Ascending/ descending through the brainstem
Includes ascending reticular activating system- role in arousal
Mesencephalon
Midbrain
Acts as a connector between different parts of the brain
links everything together
Don’t worry too much about the next info
Parts of the midbrain
Tectum (dorsal part) splits into:
Superior colliculus- visual processing + eye movement control
Inferior colliculus- auditory processing
![]()
Disorders of the mesencephalon
Parkinson’s - reduction in dopaminergic neurones in substantia nigra
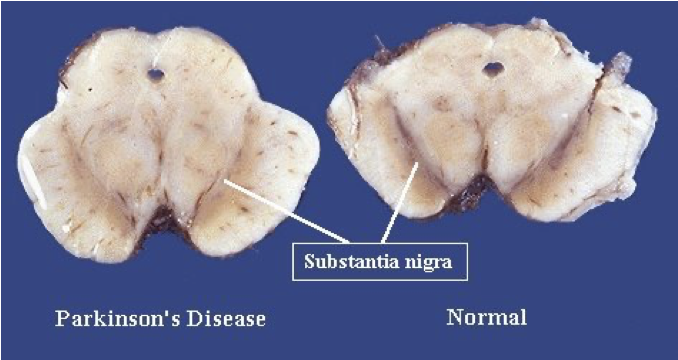
Schizophrenia- increased dopamine in substantia nigra
Multi-system atrophy- degeneration of striatum and substantia nigra
Ventral tegmental area- primary sites of addictive drugs (heroin, cocaine, alcohol, nicotine)
Diencephalon
Contains:
Thalamus
Hypothalamus
Pineal Body
Subthalamus
Epithalamus
Mammillary bodies
Limbic system:
Connects cortical control to memory / sensory/ secretory areas
Involved in motivation, visceral processes + rewards
Systems of emotions
Connects a group of structures surrounding the brainstem (cingulate gyrus, hippocampus, hypothalamus + anterior thalamic nuclei)
Connecting these structures enables cortical control of emotion + plays a role in storing memory
Telencephalon
higher functions such as smell, memory + Intelligence
Hippocampus
Medial temporal lobe
Short-term memory to long term memory
Spatial memory
Includes dentate gyrus + granule cells - formation of new episodic memories, site of neurogenesis, affected in depression
Alzheimer’s + dementia → hippocampal atrophy → memory symptoms
Cortex
Memory
attention
Cognition
awareness
thought
language
consciousness
4 lobes, gyrus (fold) + sulcus
Frontal lobe
Superior frontal gyrus = self-awareness/ laughter
Middle frontal gyrus
Inferior frontal gyrus = language processing, Broca’s area
Medial frontal gyrus = executive mechanism
Paraolfactory area= limbic
Orbitofrontal cortex= stimulus-reward, stimulus/outcome, addiction
Ventromedial prefrontal cortex- decision making, emotion regulation, addiction
frontotemporal dementia/ Pick’s disease = genetic + accumulation of tau + frontal symptoms
Prefrontal cortex
Planning + executing actions
One of the last to develop
lesions:
Dramatic changes in personality
Loss of spontaneity/ problems with initiating speech/ movements
inability to make + carry out sequences of actions/plans
Parietal lobe
Integrates sensory information
Dominant hemisphere lesions:
Dysphasia, aphasia
Dyscalculia- difficulty learning, doing calculations
Dyslexia
Apraxia- ability to execute or carry out skilled movements and gestures, despite having the desire and the physical ability to perform them.
Agnosia- inability to recognize and identify objects or persons.
Gerstmann syndrome- Dyscalculia, Dysphasia, finger agnosia, LR disorientation
Non- dominant hemisphere lesions:
Spatial disorientation
Constructional apraxia
Dressing apraxia
anosognosia- unaware of their own health problems
Temporal lobe
Transeverse temporal gyri - Heschl’s gyri
Superior temporal gyrus= auditory context with TTG. Pricess perception of sound + apply comprehension.
Posterior STG = wernicke’s area
Middle temporal gyrus
Fusiform gyrus = FACIAL RECOGNITION, synaesthesia, dyslexia, prosopagnosia
Inferior temporal gyrus= visual object recognition
Occipital lobe
Lingual gyrus
role in vision + dreaming
Visuo-limbic integration
encoding complex images
word processing
Cuneus - basic visual processing
Calcarine sulcus/fissure
primary visual cortex
takes signals from geniculate nucleus via thalamus
Tracts- only for reference
Arcuate fasciculus- links Broca’s + Wernicks area
Uncinate fasciculus
Links temporal inferior frontal gyrus + frontal lobe
Hippocampus + amygdala with orbitofrontal cortex
implicated in several psych conditions
2 visual streams hypothesis:
dorsal - where?
ventral- what?
Central dopamine hypothesis
Meso-cortical pathway
Meso-limbic pathway
Nigrostriatal pathway
Affected in schizophrenia + other psych disorders
Medications for scz work on this pathway
Side effects of these meds are linked to these pathways (e.g. cog-wheel rigidity like that seen in parkinson’s/ galactorrhea due to pituitary stimulation)
Alzheimer’s Dementia
Microscopic accumulations of peptide amyloid-β – plaques → cause loss of synapses, then neurons.
Progressive degeneration
Early changes in the hippocampus (first to be damaged)
Generalised shrinking and enlarged ventricles follow
In severe depression, the dentate gyrus don’t light up in the scans which means they don’t form many memories.
Drug misuse
The reward system is based on dopamine.
It activates all dopamine pathways, particularly the mesolimbic pathway.
Dopamine is produced in the Vental Tegmental Area (VTA).
The mesolimbic pathway links this to the Nucleus Accumbens (motivation/ reward).
If we do something good, or use an addictive drug, this pathway is stimulated.
The mesocortical pathway is also activated.
This links to the Prefrontal Cortex (PFC).
This changes how you prioritise and plan.
Disorders
Case 1- depression after frontal tumour
56 year old female
Progressive apathy
Social withdrawal
Poor self-care for part 3 years
Admitted to a psychiatric facility for depression
unresponsive to antidepressants so CT was conducted
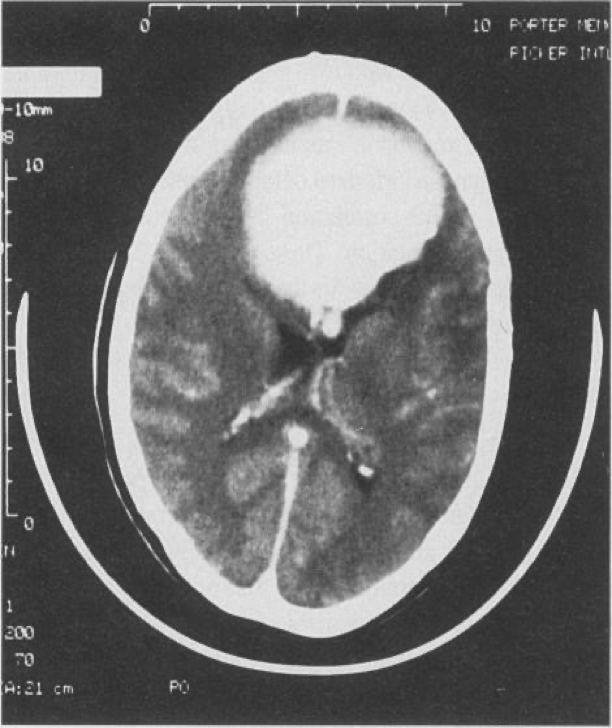
8cm medial bifrontal mass
Total excision benign transitional-type meningioma → rapid improvement
4 months after the operation was cheerful + motivated
Case 2- Psychosis after temporal tumour
18-year-old female
Referred form school to a psychosis clinic (high risk)
2 years of withdrawal from social activities + resent from work groups or talking in public
1 year later became concerned about unknown people stating + laughing at her for no reason
Feeling the world around her has changed
She is concerned that people are intimidating her + that there are special messages in TV for her
She is neurologically normal + an average IQ
Initial diagnosis: prodromal syndrome of schizophrenia but symptoms became more rapidly severe
Routine MRI conducted
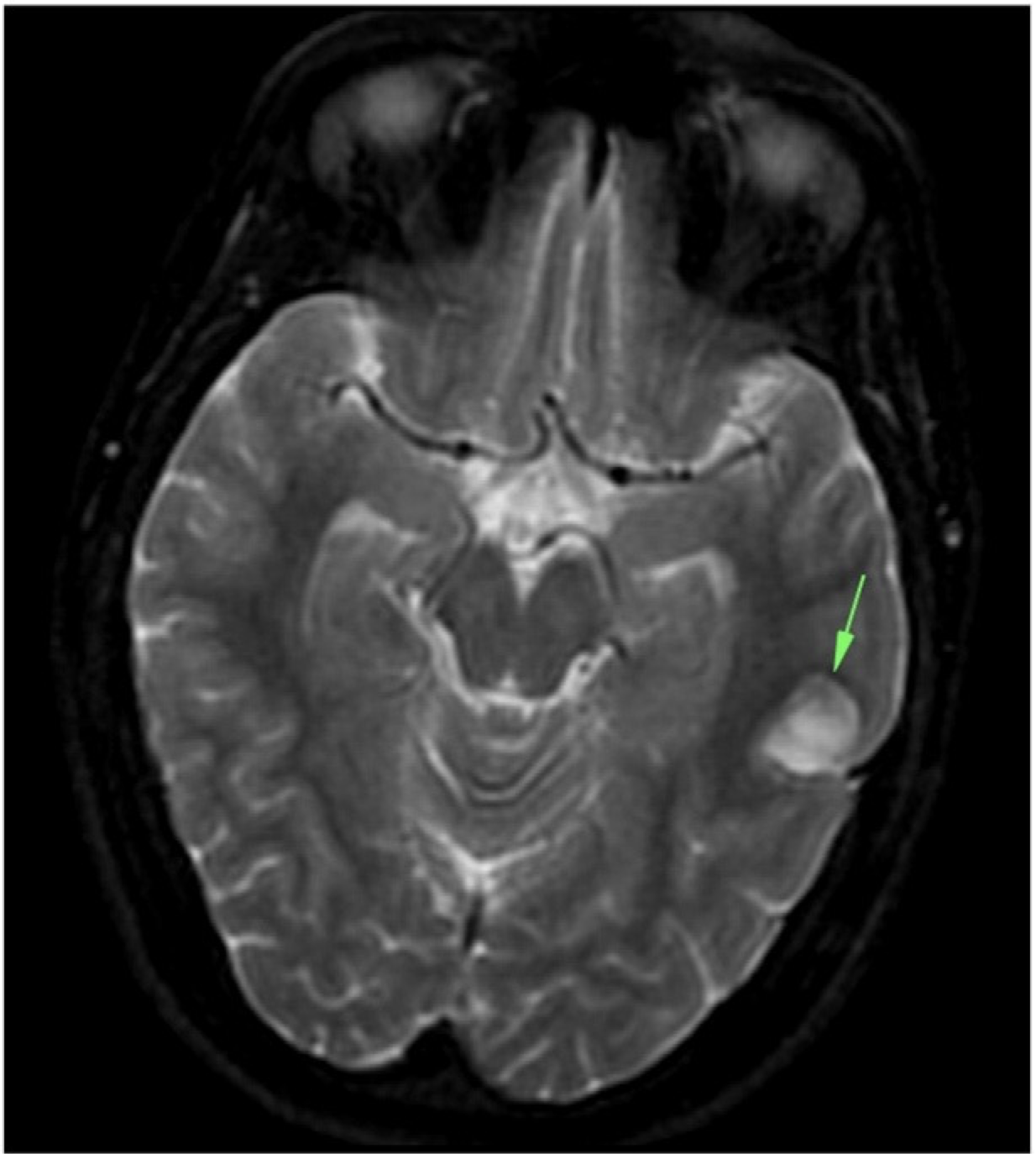
Tumour in the left temporal lobe - dysembryoplastic neuroepithelial tumour (DNET)- usually benign glial neural neoplasm
Surgically remove
Psychotic symptoms improved with the help of other treatments- risperidone + CBT
However, remained socially withdrawn
Case 3- bipolar effective disorder due to Wilsons disease
Middle aged female
Detained + admitted under section 2 of the Mental Health Act (MHA) 2007- decline in her mental state
Initially aggressive behaviour + required restrain by the Emergency Department security + police
Quietly spoken
voicing paranoid persecutory delusions
euthymic with labile affect
alternating between anger
tearfulness
displaying disinhibited affection
Doesn’t know why she was presented
CT

Hypodensity in the putamen, worse on the left
No mass, infarct or infectious process to explain the lesions
Consistent with the MRI from a couple of months ago which demonstrates hyperintensity of both putamina
Associated with Wilson’s disease
final diagnosis: psychosis secondary to neurological Wilson’s Disease
Case 4- Psychiatric syndromes associated with neurological disease
63-year-old male
paranoia
impaired anterograde memory + fatigue
FLAIR scan shows bilateral hyperintensities in the hippocampus (arrows) → shows inflammatory process
Blood tests revealed anti-voltage gated potassium channel antibodies
 Knowt
Knowt