
Chapter 20: The Cardiovascular System: Blood Vessels and Circulation
Structure and Function of Blood Vessels
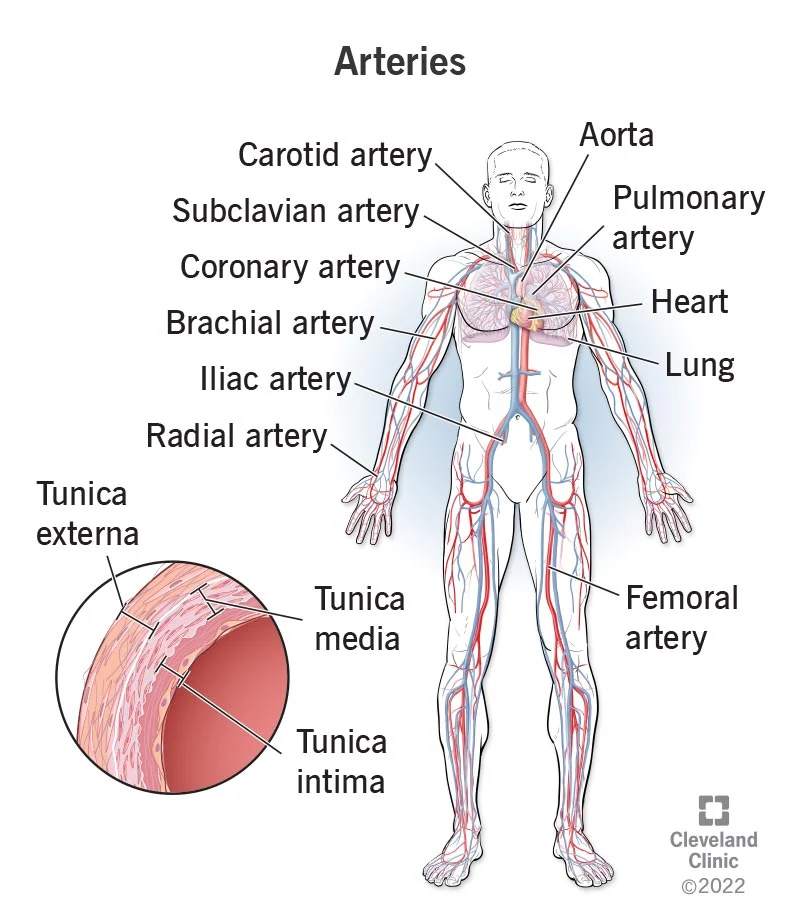
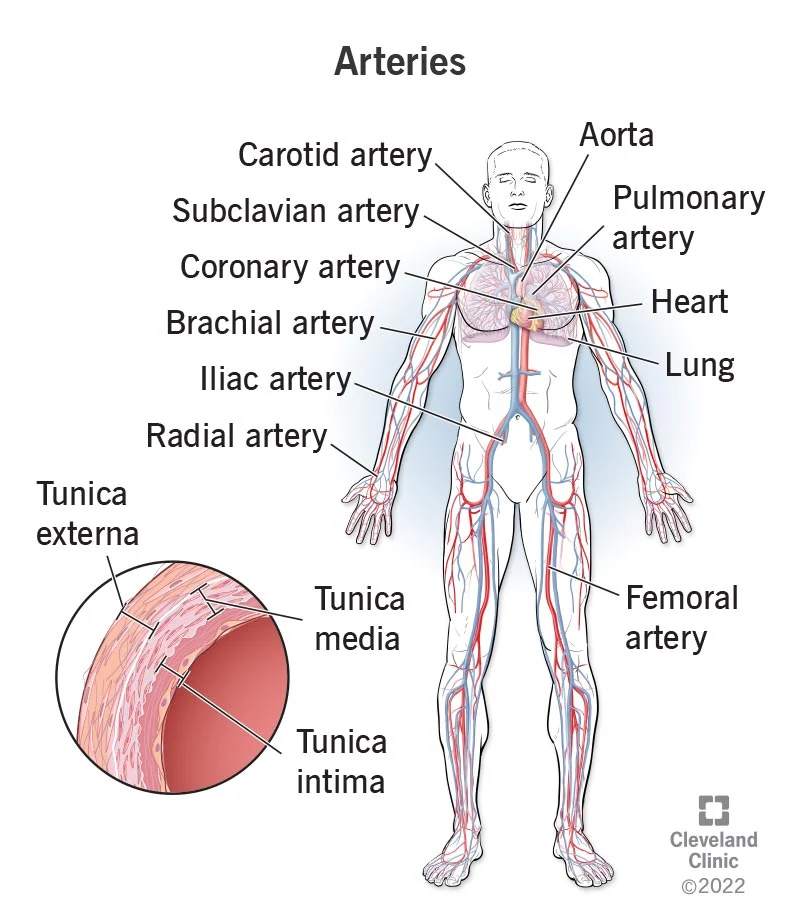
Blood is carried through the body via blood vessels.
An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels.
Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries, where nutrients and wastes are exchanged, and then combine with other vessels that exit capillaries to form venules, small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart.
Comparison of Tunics in Arteries and Veins
Arteries | Veins | |
|---|---|---|
General appearance | Thick walls with small lumensGenerally appear rounded | Thin walls with large lumensGenerally appear flattened |
Tunica intima | Endothelium usually appears wavy due to constriction ofsmooth muscleInternal elastic membrane present in larger vessels | Endothelium appears smoothInternal elastic membraneabsent |
Tunica media | Normally the thickest layer in arteriesSmooth muscle cells and elastic fibers predominate (theproportions of these vary with distance from the heart)External elastic membrane present in larger vessels | Normally thinner than thetunica externaSmooth muscle cells andcollagenous fiberspredominateNervi vasorum and vasavasorum presentExternal elastic membraneabsent |
Tunica externa | Normally thinner than the tunica media in all but the largestarteriesCollagenous and elastic fibersNervi vasorum and vasa vasorum present | Normally the thickest layer inveinsCollagenous and smoothfibers predominateSome smooth muscle fibersNervi vasorum and vasavasorum present |
Tunica Intima
The tunica intima (also called the tunica interna) is composed of epithelial and connective tissue layers.
In larger arteries, there is also a thick, distinct layer of elastic fibers known as the internal elastic membrane (also called the internal elastic lamina) at the boundary with the tunica media.
Tunica Media
The tunica media is the substantial middle layer of the vessel wall.
The tunica media consists of layers of smooth muscle supported by connective tissue that is primarily made up of elastic fibers, most of which are arranged in circular sheets.
Both vasoconstriction and vasodilation are regulated in part by small vascular nerves, known as nervi vasorum, or “nerves of the vessel,” that run within the walls of blood vessels.
Separating the tunica media from the outer tunica externa in larger arteries is the external elastic membrane (also called the external elastic lamina), which also appears wavy in slides.
Tunica Externa: The outer tunic, the tunica externa (also called the tunica adventitia), is a substantial sheath of connective tissue composed primarily of collagenous fibers.
Arteries
An artery is a blood vessel that conducts blood away from the heart.
However, those close to the heart have the thickest walls, containing a high percentage of elastic fibers in all three of their tunics. This type of artery is known as an elastic artery.
Arterioles: An arteriole is a very small artery that leads to a capillary.
Capillaries
A capillary is a microscopic channel that supplies blood to the tissues themselves, a process called perfusion.
Flow through capillaries is often described as microcirculation.
Continuous Capillaries: The most common type of capillary, the continuous capillary, is found in almost all vascularized tissues.
Fenestrated Capillaries: A fenestrated capillary is one that has pores (or fenestrations) in addition to tight junctions in the endothelial lining.
Sinusoid Capillaries
A sinusoid capillary (or sinusoid) is the least common type of capillary.
Sinusoid capillaries are flattened, and they have extensive intercellular gaps and incomplete basement membranes, in addition to intercellular clefts and fenestrations.
Metarterioles and Capillary Beds
A metarteriole is a type of vessel that has structural characteristics of both an arteriole and a capillary.
Each metarteriole arises from a terminal arteriole and branches to supply blood to a capillary bed that may consist of 10–100 capillaries.
The precapillary sphincters, circular smooth muscle cells that surround the capillary at its origin with the metarteriole, tightly regulate the flow of blood from a metarteriole to the capillaries it supplies.
An arteriovenous anastomosis may bypass the capillary bed and lead directly to the venous system.
Venules: A venule is an extremely small vein, generally 8–100 micrometers in diameter.
Veins: A vein is a blood vessel that conducts blood toward the heart.
Veins as Blood Reservoirs
Their ability to hold this much blood is due to their high capacitance, that is, their capacity to distend (expand) readily to store a high volume of blood, even at a low pressure.
The large lumens and relatively thin walls of veins make them far more distensible than arteries; thus, they are said to be capacitance vessels.
Blood Flow, Blood Pressure, and Resistance
Blood flow refers to the movement of blood through a vessel, tissue, or organ, and is usually expressed in terms of volume of blood per unit of time.
One form of hydrostatic pressure is blood pressure, the force exerted by blood upon the walls of the blood vessels or the chambers of the heart.
Systolic and Diastolic Pressures
The systolic pressure is the higher value (typically around 120 mm Hg) and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction, or systole.
The diastolic pressure is the lower value (usually about 80 mm Hg) and represents the arterial pressure of blood during ventricular relaxation, or diastole.
Mean Arterial Pressure: Mean arterial pressure (MAP) represents the “average” pressure of blood in the arteries, that is, the average force driving blood into vessels that serve the tissues.
Pulse
After blood is ejected from the heart, elastic fibers in the arteries help maintain a high-pressure gradient as they expand to accommodate the blood, then recoil.
This expansion and recoiling effect, known as the pulse, can be palpated manually or measured electronically.
Measurement of Blood Pressure
Blood pressure is one of the critical parameters measured on virtually every patient in every healthcare setting.
Turbulent blood flow through the vessels can be heard as a soft ticking while measuring blood pressure; these sounds are known as Korotkoff sounds.
The technique of measuring blood pressure requires the use of a sphygmomanometer (a blood pressure cuff attached to a measuring device) and a stethoscope.
Five variables influence blood flow and blood pressure:
Cardiac output
Compliance
Volume of the blood
Viscosity of the blood
Blood vessel length and diameter
Compliance: Compliance is the ability of any compartment to expand to accommodate increased content.
Skeletal Muscle Pump: In many body regions, the pressure within the veins can be increased by the contraction of the surrounding skeletal muscle.
Respiratory Pump: The respiratory pump aids blood flow through the veins of the thorax and abdomen.
Bulk Flow
This movement, often referred to as bulk flow, involves two pressure-driven mechanisms:
Volumes of fluid move from an area of higher pressure in a capillary bed to an area of lower pressure in the tissues via filtration.
Hydrostatic Pressure
Blood hydrostatic pressure is the force exerted by the blood confined within blood vessels or heart chambers.
Even more specifically, the pressure exerted by blood against the wall of a capillary is called capillary hydrostatic pressure (CHP), and is the same as capillary blood pressure.
Osmotic Pressure
The pressure created by the concentration of colloidal proteins in the blood is called the blood colloidal osmotic pressure (BCOP).
The net filtration pressure (NFP) represents the interaction of the hydrostatic and osmotic pressures, driving fluid out of the capillary.
Baroreceptor Reflexes
Baroreceptors are specialized stretch receptors located within thin areas of blood vessels and heart chambers that respond to the degree of stretch caused by the presence of blood.
Chemoreceptor Reflexes
Chemoreceptors monitoring the blood are located in close proximity to the baroreceptors in the aortic and carotid sinuses.
They signal the cardiovascular center as well as the respiratory centers in the medulla oblongata.
Endocrine Regulation
Endocrine control over the cardiovascular system involves the catecholamines, epinephrine and norepinephrine, as well as several hormones that interact with the kidneys in the regulation of blood volume.
Antidiuretic Hormone
Antidiuretic hormone (ADH), also known as vasopressin, is secreted by the cells in the hypothalamus and transported via the hypothalamic-hypophyseal tracts to the posterior pituitary where it is stored until released upon nervous stimulation.
Erythropoietin
Erythropoietin (EPO) is released by the kidneys when blood flow and/or oxygen levels decrease.
EPO stimulates the production of erythrocytes within the bone marrow.
Atrial Natriuretic Hormone
Secreted by cells in the atria of the heart, atrial natriuretic hormone (ANH) (also known as atrial natriuretic peptide) is secreted when blood volume is high enough to cause extreme stretching of the cardiac cells.
The Myogenic Response: The myogenic response is a reaction to the stretching of the smooth muscle in the walls of arterioles as changes in blood flow occur through the vessel.
Hypertension and Hypotension
Chronically elevated blood pressure is known clinically as hypertension.
It is defined as chronic and persistent blood pressure measurements of 140/90 mm Hg or above.
Hemorrhage: Hemorrhage is a loss of blood that cannot be controlled by hemostatic mechanisms.
Circulatory Shock
The loss of too much blood may lead to circulatory shock, a life-threatening condition in which the circulatory system is unable to maintain blood flow to adequately supply sufficient oxygen and other nutrients to the tissues to maintain cellular metabolism.
Hypovolemic shock in adults is typically caused by hemorrhage, although in children it may be caused by fluid losses related to severe vomiting or diarrhea.
Cardiogenic shock results from the inability of the heart to maintain cardiac output.
Vascular shock occurs when arterioles lose their normal muscular tone and dilate dramatically.
A common cause is sepsis (or septicemia), also called “blood poisoning,” which is a widespread bacterial infection that results in an organismal-level inflammatory response known as septic shock.
Anaphylactic shock is a severe allergic response that causes the widespread release of histamines, triggering vasodilation throughout the body.
Obstructive shock, as the name would suggest, occurs when a significant portion of the vascular system is blocked.
Pulmonary Circulation
From the right atrium, blood moves into the right ventricle, which pumps it to the lungs for gas exchange. This system of vessels is referred to as the pulmonary circuit.
The single vessel exiting the right ventricle is the pulmonary trunk.
As the pulmonary trunk reaches the superior surface of the heart, it curves posteriorly and rapidly bifurcates (divides) into two branches, a left and a right pulmonary artery.
Once gas exchange is completed, oxygenated blood flows from the pulmonary capillaries into a series of pulmonary venules that eventually lead to a series of larger pulmonary veins.
The Aorta
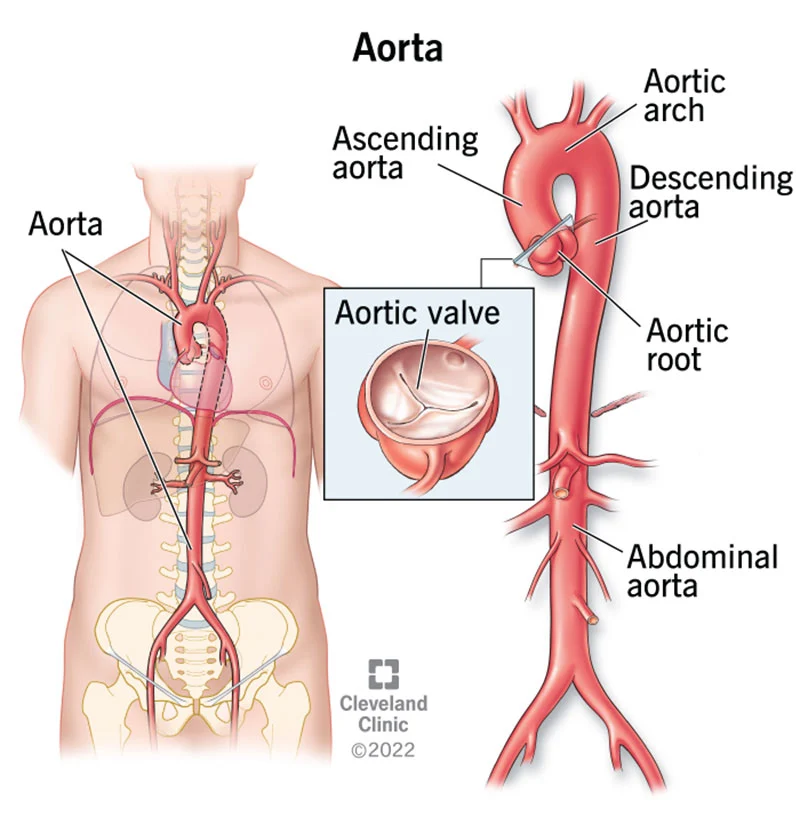
The aorta is the largest artery in the body.
After exiting the heart, the ascending aorta moves in a superior direction for approximately 5 cm and ends at the sternal angle.
Forming a graceful arc to the left, called the aortic arch.
Beyond this point, the descending aorta continues close to the bodies of the vertebrae and passes through an opening in the diaphragm known as the aortic hiatus.
Superior to the diaphragm, the aorta is called the thoracic aorta, and inferior to the diaphragm, it is called the abdominal aorta.
Aortic Arch Branches
Each subclavian artery supplies blood to the arms, chest, shoulders, back, and central nervous system.
The internal thoracic artery, or mammary artery, supplies blood to the thymus, the pericardium of the heart, and the anterior chest wall.
The vertebral artery passes through the vertebral foramen in the cervical vertebrae and then through the foramen magnum into the cranial cavity to supply blood to the brain and spinal cord.
The subclavian artery also gives rise to the thyrocervical artery that provides blood to the thyroid, the cervical region of the neck, and the upper back and shoulder.
The common carotid artery divides into internal and external carotid arteries.
The external carotid artery supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx.
The internal carotid artery initially forms an expansion known as the carotid sinus, containing the carotid baroreceptors and chemoreceptors.
Loss of blood flow for longer periods, typically between 3 and 4 minutes, will likely produce irreversible brain damage or a stroke, also called a cerebrovascular accident (CVA).
The anterior cerebral artery that supplies blood to the frontal lobe of the cerebrum.
The middle cerebral artery, supplies blood to the temporal and parietal lobes, which are the most common sites of CVAs.
The ophthalmic artery, the third major branch, provides blood to the eyes.
The right and left anterior cerebral arteries join together to form an anastomosis called the anterior communicating artery.
The posterior portion of the arterial circle is formed by a left and a right posterior communicating artery that branches from the posterior cerebral artery, which arises from the basilar artery.
The basilar artery is an anastomosis that begins at the junction of the two vertebral arteries and sends branches to the cerebellum and brain stem.
Thoracic Aorta and Major Branches
Those branches that supply blood primarily to visceral organs are known as the visceral branches and include the bronchial arteries, pericardial arteries, esophageal arteries, and the mediastinal arteries, each named after the tissues it supplies.
Each bronchial artery (typically two on the left and one on the right) supplies systemic blood to the lungs and visceral pleura, in addition to the blood pumped to the lungs for oxygenation via the pulmonary circuit.
Each pericardial artery supplies blood to the pericardium, the esophageal artery provides blood to the esophagus, and the mediastinal artery provides blood to the mediastinum.
Each intercostal artery provides blood to the muscles of the thoracic cavity and vertebral column.
The superior phrenic artery provides blood to the superior surface of the diaphragm.
Abdominal Aorta and Major Branches
A single celiac trunk (artery) emerges and divides into the left gastric artery to supply blood to the stomach and esophagus, the splenic artery to supply blood to the spleen, and the common hepatic artery, which in turn gives rise to the hepatic artery proper to supply blood to the liver, the right gastric artery to supply blood to the stomach, the cystic artery to supply blood to the gall bladder, and several branches, one to supply blood to the duodenum and another to supply blood to the pancreas.
The superior mesenteric artery arises approximately 2.5 cm after the celiac trunk and branches into several major vessels that supply blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine.
The inferior mesenteric artery supplies blood to the distal segment of the large intestine, including the rectum.
Each inferior phrenic artery is a counterpart of a superior phrenic artery and supplies blood to the inferior surface of the diaphragm.
The adrenal artery supplies blood to the adrenal (suprarenal) glands and arises near the superior mesenteric artery.
Each renal artery branches approximately 2.5 cm inferior to the superior mesenteric arteries and supplies a kidney.
Gonadal artery supplies blood to the gonads, or reproductive organs, and is also described as either an ovarian artery or a testicular artery (internal spermatic), depending upon the sex of the individual.
An ovarian artery supplies blood to an ovary, uterine (Fallopian) tube, and the uterus, and is located within the suspensory ligament of the uterus.
Arteries Serving the Upper Limbs
As the subclavian artery exits the thorax into the axillary region, it is renamed the axillary artery.
The brachial artery supplies blood to much of the brachial region and divides at the elbow into several smaller branches, including the deep brachial arteries, which provide blood to the posterior surface of the arm, and the ulnar collateral arteries, which supply blood to the region of the elbow.
The radial artery and ulnar artery parallel their namesake bones, giving off smaller branches until they reach the wrist, or carpal region.
Arteries Serving the Lower Limbs
As it passes through the body wall, it is renamed the femoral artery.
It gives off several smaller branches as well as the lateral deep femoral artery that in turn gives rise to a lateral circumflex artery.
The femoral artery also gives rise to the genicular artery, which provides blood to the region of the knee
The popliteal artery branches into the anterior and posterior tibial arteries..
The anterior tibial artery is located between the tibia and fibula, and supplies blood to the muscles and integument of the anterior tibial region.
Upon reaching the tarsal region, it becomes the dorsalis pedis artery, which branches repeatedly and provides blood to the tarsal and dorsal regions of the foot.
The posterior tibial artery provides blood to the muscles and integument on the posterior surface of the tibial region.
There is an anastomosis with the dorsalis pedis artery, and the medial and lateral plantar arteries form two arches called the dorsal arch (also called the arcuate arch) and the plantar arch, which provide blood to the remainder of the foot and toes.
The Superior Vena Cava
The superior vena cava drains most of the body superior to the diaphragm.
On both the left and right sides, the subclavian vein forms when the axillary vein passes through the body wall from the axillary region.
Each vertebral vein also flows into the brachiocephalic vein close to this fusion.
Each internal thoracic vein, also known as an internal mammary vein, drains the anterior surface of the chest wall and flows into the brachiocephalic vein.
Veins of the Head and Neck
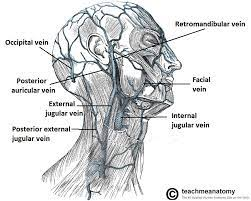
Blood from the brain and the superficial facial vein flow into each internal jugular vein.
Blood from the more superficial portions of the head, scalp, and cranial regions, including the temporal vein and maxillary vein, flow into each external jugular vein.
Veins Draining the Upper Limbs
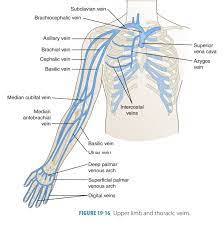
The digital veins in the fingers come together in the hand to form the palmar venous arches.
The radial vein and the ulnar vein parallel the bones of the forearm and join together at the antebrachium to form the brachial vein, a deep vein that flows into the axillary vein in the brachium.
The median antebrachial vein parallels the ulnar vein, is more medial in location, and joins the basilic vein in the forearm.
As the basilic vein reaches the antecubital region, it gives off a branch called the median cubital vein that crosses at an angle to join the cephalic vein.
The cephalic vein begins in the antebrachium and drains blood from the superficial surface of the arm into the axillary vein.
The subscapular vein drains blood from the subscapular region and joins the cephalic vein to form the axillary vein.
The Inferior Vena Cava
Lying just beneath the parietal peritoneum in the abdominal cavity, the inferior vena cava parallels the abdominal aorta, where it can receive blood from abdominal veins.
Blood supply from the kidneys flows into each renal vein, normally the largest veins entering the inferior vena cava.
Veins Draining the Lower Limbs
The superior surface of the foot drains into the digital veins, and the inferior surface drains into the plantar veins, which flow into a complex series of anastomoses in the feet and ankles, including the dorsal venous arch and the plantar venous arch.
The anterior tibial vein drains the area near the tibialis anterior muscle and combines with the posterior tibial vein and the fibular vein to form the popliteal vein.
The posterior tibial vein drains the posterior surface of the tibia and joins the popliteal vein.
The fibular vein drains the muscles and integument in proximity to the fibula and also joins the popliteal vein.
The small saphenous vein located on the lateral surface of the leg drains blood from the superficial regions of the lower leg and foot, and flows into to the popliteal vein.
Development of Blood Vessels and Fetal Circulation
During those first few weeks, blood vessels begin to form from the embryonic mesoderm. The precursor cells are known as hemangioblasts.
Vascular tubes also develop on the blood islands, and they eventually connect to one another as well as to the developing, tubular heart.
This angiogenesis the creation of new blood vessels from existing ones continues as needed throughout life as we grow and develop.
Emerging from the placenta is the umbilical vein, which carries oxygen-rich blood from the mother to the fetal inferior vena cava via the ductus venosus to the heart that pumps it into fetal circulation.
The foramen ovale is an opening in the interatrial septum that allows blood to flow from the right atrium to the left atrium.
The ductus arteriosus is a short, muscular vessel that connects the pulmonary trunk to the aorta.
The ductus venosus is a temporary blood vessel that branches from the umbilical vein, allowing much of the freshly oxygenated blood from the placenta the organ of gas exchange between the mother and fetus to bypass the fetal liver and go directly to the fetal heart.
Chapter 20: The Cardiovascular System: Blood Vessels and Circulation
Structure and Function of Blood Vessels
Blood is carried through the body via blood vessels.
An artery is a blood vessel that carries blood away from the heart, where it branches into ever-smaller vessels.
Eventually, the smallest arteries, vessels called arterioles, further branch into tiny capillaries, where nutrients and wastes are exchanged, and then combine with other vessels that exit capillaries to form venules, small blood vessels that carry blood to a vein, a larger blood vessel that returns blood to the heart.
Comparison of Tunics in Arteries and Veins
Arteries | Veins | |
|---|---|---|
General appearance | Thick walls with small lumensGenerally appear rounded | Thin walls with large lumensGenerally appear flattened |
Tunica intima | Endothelium usually appears wavy due to constriction ofsmooth muscleInternal elastic membrane present in larger vessels | Endothelium appears smoothInternal elastic membraneabsent |
Tunica media | Normally the thickest layer in arteriesSmooth muscle cells and elastic fibers predominate (theproportions of these vary with distance from the heart)External elastic membrane present in larger vessels | Normally thinner than thetunica externaSmooth muscle cells andcollagenous fiberspredominateNervi vasorum and vasavasorum presentExternal elastic membraneabsent |
Tunica externa | Normally thinner than the tunica media in all but the largestarteriesCollagenous and elastic fibersNervi vasorum and vasa vasorum present | Normally the thickest layer inveinsCollagenous and smoothfibers predominateSome smooth muscle fibersNervi vasorum and vasavasorum present |
Tunica Intima
The tunica intima (also called the tunica interna) is composed of epithelial and connective tissue layers.
In larger arteries, there is also a thick, distinct layer of elastic fibers known as the internal elastic membrane (also called the internal elastic lamina) at the boundary with the tunica media.
Tunica Media
The tunica media is the substantial middle layer of the vessel wall.
The tunica media consists of layers of smooth muscle supported by connective tissue that is primarily made up of elastic fibers, most of which are arranged in circular sheets.
Both vasoconstriction and vasodilation are regulated in part by small vascular nerves, known as nervi vasorum, or “nerves of the vessel,” that run within the walls of blood vessels.
Separating the tunica media from the outer tunica externa in larger arteries is the external elastic membrane (also called the external elastic lamina), which also appears wavy in slides.
Tunica Externa: The outer tunic, the tunica externa (also called the tunica adventitia), is a substantial sheath of connective tissue composed primarily of collagenous fibers.
Arteries
An artery is a blood vessel that conducts blood away from the heart.
However, those close to the heart have the thickest walls, containing a high percentage of elastic fibers in all three of their tunics. This type of artery is known as an elastic artery.
Arterioles: An arteriole is a very small artery that leads to a capillary.
Capillaries
A capillary is a microscopic channel that supplies blood to the tissues themselves, a process called perfusion.
Flow through capillaries is often described as microcirculation.
Continuous Capillaries: The most common type of capillary, the continuous capillary, is found in almost all vascularized tissues.
Fenestrated Capillaries: A fenestrated capillary is one that has pores (or fenestrations) in addition to tight junctions in the endothelial lining.
Sinusoid Capillaries
A sinusoid capillary (or sinusoid) is the least common type of capillary.
Sinusoid capillaries are flattened, and they have extensive intercellular gaps and incomplete basement membranes, in addition to intercellular clefts and fenestrations.
Metarterioles and Capillary Beds
A metarteriole is a type of vessel that has structural characteristics of both an arteriole and a capillary.
Each metarteriole arises from a terminal arteriole and branches to supply blood to a capillary bed that may consist of 10–100 capillaries.
The precapillary sphincters, circular smooth muscle cells that surround the capillary at its origin with the metarteriole, tightly regulate the flow of blood from a metarteriole to the capillaries it supplies.
An arteriovenous anastomosis may bypass the capillary bed and lead directly to the venous system.
Venules: A venule is an extremely small vein, generally 8–100 micrometers in diameter.
Veins: A vein is a blood vessel that conducts blood toward the heart.
Veins as Blood Reservoirs
Their ability to hold this much blood is due to their high capacitance, that is, their capacity to distend (expand) readily to store a high volume of blood, even at a low pressure.
The large lumens and relatively thin walls of veins make them far more distensible than arteries; thus, they are said to be capacitance vessels.
Blood Flow, Blood Pressure, and Resistance
Blood flow refers to the movement of blood through a vessel, tissue, or organ, and is usually expressed in terms of volume of blood per unit of time.
One form of hydrostatic pressure is blood pressure, the force exerted by blood upon the walls of the blood vessels or the chambers of the heart.
Systolic and Diastolic Pressures
The systolic pressure is the higher value (typically around 120 mm Hg) and reflects the arterial pressure resulting from the ejection of blood during ventricular contraction, or systole.
The diastolic pressure is the lower value (usually about 80 mm Hg) and represents the arterial pressure of blood during ventricular relaxation, or diastole.
Mean Arterial Pressure: Mean arterial pressure (MAP) represents the “average” pressure of blood in the arteries, that is, the average force driving blood into vessels that serve the tissues.
Pulse
After blood is ejected from the heart, elastic fibers in the arteries help maintain a high-pressure gradient as they expand to accommodate the blood, then recoil.
This expansion and recoiling effect, known as the pulse, can be palpated manually or measured electronically.
Measurement of Blood Pressure
Blood pressure is one of the critical parameters measured on virtually every patient in every healthcare setting.
Turbulent blood flow through the vessels can be heard as a soft ticking while measuring blood pressure; these sounds are known as Korotkoff sounds.
The technique of measuring blood pressure requires the use of a sphygmomanometer (a blood pressure cuff attached to a measuring device) and a stethoscope.
Five variables influence blood flow and blood pressure:
Cardiac output
Compliance
Volume of the blood
Viscosity of the blood
Blood vessel length and diameter
Compliance: Compliance is the ability of any compartment to expand to accommodate increased content.
Skeletal Muscle Pump: In many body regions, the pressure within the veins can be increased by the contraction of the surrounding skeletal muscle.
Respiratory Pump: The respiratory pump aids blood flow through the veins of the thorax and abdomen.
Bulk Flow
This movement, often referred to as bulk flow, involves two pressure-driven mechanisms:
Volumes of fluid move from an area of higher pressure in a capillary bed to an area of lower pressure in the tissues via filtration.
Hydrostatic Pressure
Blood hydrostatic pressure is the force exerted by the blood confined within blood vessels or heart chambers.
Even more specifically, the pressure exerted by blood against the wall of a capillary is called capillary hydrostatic pressure (CHP), and is the same as capillary blood pressure.
Osmotic Pressure
The pressure created by the concentration of colloidal proteins in the blood is called the blood colloidal osmotic pressure (BCOP).
The net filtration pressure (NFP) represents the interaction of the hydrostatic and osmotic pressures, driving fluid out of the capillary.
Baroreceptor Reflexes
Baroreceptors are specialized stretch receptors located within thin areas of blood vessels and heart chambers that respond to the degree of stretch caused by the presence of blood.
Chemoreceptor Reflexes
Chemoreceptors monitoring the blood are located in close proximity to the baroreceptors in the aortic and carotid sinuses.
They signal the cardiovascular center as well as the respiratory centers in the medulla oblongata.
Endocrine Regulation
Endocrine control over the cardiovascular system involves the catecholamines, epinephrine and norepinephrine, as well as several hormones that interact with the kidneys in the regulation of blood volume.
Antidiuretic Hormone
Antidiuretic hormone (ADH), also known as vasopressin, is secreted by the cells in the hypothalamus and transported via the hypothalamic-hypophyseal tracts to the posterior pituitary where it is stored until released upon nervous stimulation.
Erythropoietin
Erythropoietin (EPO) is released by the kidneys when blood flow and/or oxygen levels decrease.
EPO stimulates the production of erythrocytes within the bone marrow.
Atrial Natriuretic Hormone
Secreted by cells in the atria of the heart, atrial natriuretic hormone (ANH) (also known as atrial natriuretic peptide) is secreted when blood volume is high enough to cause extreme stretching of the cardiac cells.
The Myogenic Response: The myogenic response is a reaction to the stretching of the smooth muscle in the walls of arterioles as changes in blood flow occur through the vessel.
Hypertension and Hypotension
Chronically elevated blood pressure is known clinically as hypertension.
It is defined as chronic and persistent blood pressure measurements of 140/90 mm Hg or above.
Hemorrhage: Hemorrhage is a loss of blood that cannot be controlled by hemostatic mechanisms.
Circulatory Shock
The loss of too much blood may lead to circulatory shock, a life-threatening condition in which the circulatory system is unable to maintain blood flow to adequately supply sufficient oxygen and other nutrients to the tissues to maintain cellular metabolism.
Hypovolemic shock in adults is typically caused by hemorrhage, although in children it may be caused by fluid losses related to severe vomiting or diarrhea.
Cardiogenic shock results from the inability of the heart to maintain cardiac output.
Vascular shock occurs when arterioles lose their normal muscular tone and dilate dramatically.
A common cause is sepsis (or septicemia), also called “blood poisoning,” which is a widespread bacterial infection that results in an organismal-level inflammatory response known as septic shock.
Anaphylactic shock is a severe allergic response that causes the widespread release of histamines, triggering vasodilation throughout the body.
Obstructive shock, as the name would suggest, occurs when a significant portion of the vascular system is blocked.
Pulmonary Circulation
From the right atrium, blood moves into the right ventricle, which pumps it to the lungs for gas exchange. This system of vessels is referred to as the pulmonary circuit.
The single vessel exiting the right ventricle is the pulmonary trunk.
As the pulmonary trunk reaches the superior surface of the heart, it curves posteriorly and rapidly bifurcates (divides) into two branches, a left and a right pulmonary artery.
Once gas exchange is completed, oxygenated blood flows from the pulmonary capillaries into a series of pulmonary venules that eventually lead to a series of larger pulmonary veins.
The Aorta
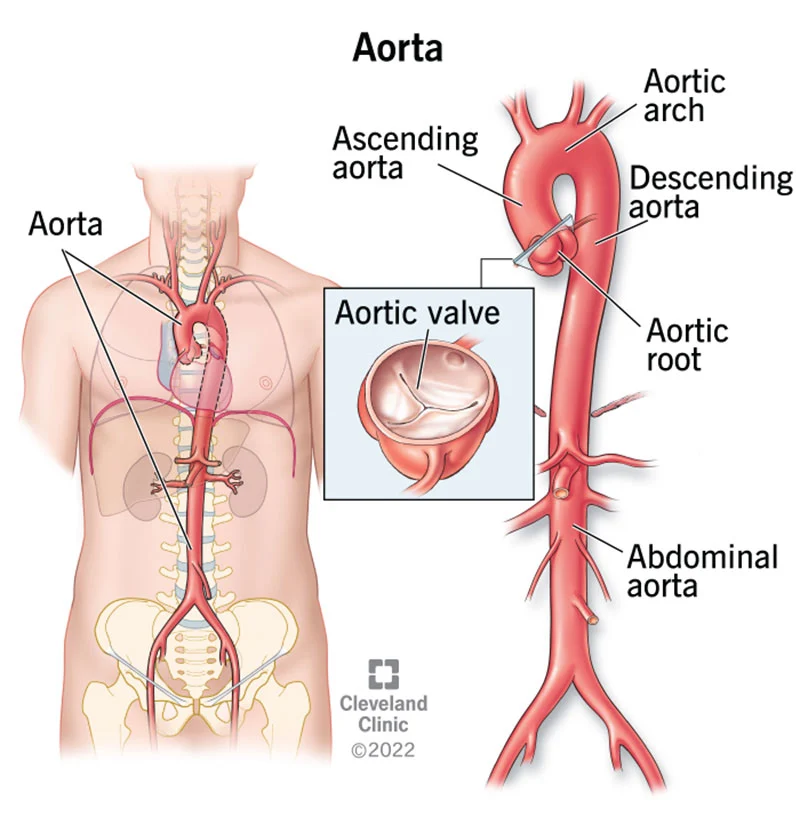
The aorta is the largest artery in the body.
After exiting the heart, the ascending aorta moves in a superior direction for approximately 5 cm and ends at the sternal angle.
Forming a graceful arc to the left, called the aortic arch.
Beyond this point, the descending aorta continues close to the bodies of the vertebrae and passes through an opening in the diaphragm known as the aortic hiatus.
Superior to the diaphragm, the aorta is called the thoracic aorta, and inferior to the diaphragm, it is called the abdominal aorta.
Aortic Arch Branches
Each subclavian artery supplies blood to the arms, chest, shoulders, back, and central nervous system.
The internal thoracic artery, or mammary artery, supplies blood to the thymus, the pericardium of the heart, and the anterior chest wall.
The vertebral artery passes through the vertebral foramen in the cervical vertebrae and then through the foramen magnum into the cranial cavity to supply blood to the brain and spinal cord.
The subclavian artery also gives rise to the thyrocervical artery that provides blood to the thyroid, the cervical region of the neck, and the upper back and shoulder.
The common carotid artery divides into internal and external carotid arteries.
The external carotid artery supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx.
The internal carotid artery initially forms an expansion known as the carotid sinus, containing the carotid baroreceptors and chemoreceptors.
Loss of blood flow for longer periods, typically between 3 and 4 minutes, will likely produce irreversible brain damage or a stroke, also called a cerebrovascular accident (CVA).
The anterior cerebral artery that supplies blood to the frontal lobe of the cerebrum.
The middle cerebral artery, supplies blood to the temporal and parietal lobes, which are the most common sites of CVAs.
The ophthalmic artery, the third major branch, provides blood to the eyes.
The right and left anterior cerebral arteries join together to form an anastomosis called the anterior communicating artery.
The posterior portion of the arterial circle is formed by a left and a right posterior communicating artery that branches from the posterior cerebral artery, which arises from the basilar artery.
The basilar artery is an anastomosis that begins at the junction of the two vertebral arteries and sends branches to the cerebellum and brain stem.
Thoracic Aorta and Major Branches
Those branches that supply blood primarily to visceral organs are known as the visceral branches and include the bronchial arteries, pericardial arteries, esophageal arteries, and the mediastinal arteries, each named after the tissues it supplies.
Each bronchial artery (typically two on the left and one on the right) supplies systemic blood to the lungs and visceral pleura, in addition to the blood pumped to the lungs for oxygenation via the pulmonary circuit.
Each pericardial artery supplies blood to the pericardium, the esophageal artery provides blood to the esophagus, and the mediastinal artery provides blood to the mediastinum.
Each intercostal artery provides blood to the muscles of the thoracic cavity and vertebral column.
The superior phrenic artery provides blood to the superior surface of the diaphragm.
Abdominal Aorta and Major Branches
A single celiac trunk (artery) emerges and divides into the left gastric artery to supply blood to the stomach and esophagus, the splenic artery to supply blood to the spleen, and the common hepatic artery, which in turn gives rise to the hepatic artery proper to supply blood to the liver, the right gastric artery to supply blood to the stomach, the cystic artery to supply blood to the gall bladder, and several branches, one to supply blood to the duodenum and another to supply blood to the pancreas.
The superior mesenteric artery arises approximately 2.5 cm after the celiac trunk and branches into several major vessels that supply blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine.
The inferior mesenteric artery supplies blood to the distal segment of the large intestine, including the rectum.
Each inferior phrenic artery is a counterpart of a superior phrenic artery and supplies blood to the inferior surface of the diaphragm.
The adrenal artery supplies blood to the adrenal (suprarenal) glands and arises near the superior mesenteric artery.
Each renal artery branches approximately 2.5 cm inferior to the superior mesenteric arteries and supplies a kidney.
Gonadal artery supplies blood to the gonads, or reproductive organs, and is also described as either an ovarian artery or a testicular artery (internal spermatic), depending upon the sex of the individual.
An ovarian artery supplies blood to an ovary, uterine (Fallopian) tube, and the uterus, and is located within the suspensory ligament of the uterus.
Arteries Serving the Upper Limbs
As the subclavian artery exits the thorax into the axillary region, it is renamed the axillary artery.
The brachial artery supplies blood to much of the brachial region and divides at the elbow into several smaller branches, including the deep brachial arteries, which provide blood to the posterior surface of the arm, and the ulnar collateral arteries, which supply blood to the region of the elbow.
The radial artery and ulnar artery parallel their namesake bones, giving off smaller branches until they reach the wrist, or carpal region.
Arteries Serving the Lower Limbs
As it passes through the body wall, it is renamed the femoral artery.
It gives off several smaller branches as well as the lateral deep femoral artery that in turn gives rise to a lateral circumflex artery.
The femoral artery also gives rise to the genicular artery, which provides blood to the region of the knee
The popliteal artery branches into the anterior and posterior tibial arteries..
The anterior tibial artery is located between the tibia and fibula, and supplies blood to the muscles and integument of the anterior tibial region.
Upon reaching the tarsal region, it becomes the dorsalis pedis artery, which branches repeatedly and provides blood to the tarsal and dorsal regions of the foot.
The posterior tibial artery provides blood to the muscles and integument on the posterior surface of the tibial region.
There is an anastomosis with the dorsalis pedis artery, and the medial and lateral plantar arteries form two arches called the dorsal arch (also called the arcuate arch) and the plantar arch, which provide blood to the remainder of the foot and toes.
The Superior Vena Cava
The superior vena cava drains most of the body superior to the diaphragm.
On both the left and right sides, the subclavian vein forms when the axillary vein passes through the body wall from the axillary region.
Each vertebral vein also flows into the brachiocephalic vein close to this fusion.
Each internal thoracic vein, also known as an internal mammary vein, drains the anterior surface of the chest wall and flows into the brachiocephalic vein.
Veins of the Head and Neck
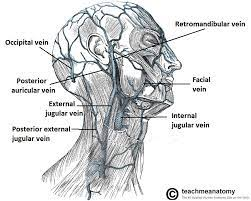
Blood from the brain and the superficial facial vein flow into each internal jugular vein.
Blood from the more superficial portions of the head, scalp, and cranial regions, including the temporal vein and maxillary vein, flow into each external jugular vein.
Veins Draining the Upper Limbs
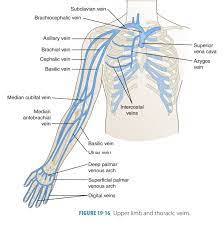
The digital veins in the fingers come together in the hand to form the palmar venous arches.
The radial vein and the ulnar vein parallel the bones of the forearm and join together at the antebrachium to form the brachial vein, a deep vein that flows into the axillary vein in the brachium.
The median antebrachial vein parallels the ulnar vein, is more medial in location, and joins the basilic vein in the forearm.
As the basilic vein reaches the antecubital region, it gives off a branch called the median cubital vein that crosses at an angle to join the cephalic vein.
The cephalic vein begins in the antebrachium and drains blood from the superficial surface of the arm into the axillary vein.
The subscapular vein drains blood from the subscapular region and joins the cephalic vein to form the axillary vein.
The Inferior Vena Cava
Lying just beneath the parietal peritoneum in the abdominal cavity, the inferior vena cava parallels the abdominal aorta, where it can receive blood from abdominal veins.
Blood supply from the kidneys flows into each renal vein, normally the largest veins entering the inferior vena cava.
Veins Draining the Lower Limbs
The superior surface of the foot drains into the digital veins, and the inferior surface drains into the plantar veins, which flow into a complex series of anastomoses in the feet and ankles, including the dorsal venous arch and the plantar venous arch.
The anterior tibial vein drains the area near the tibialis anterior muscle and combines with the posterior tibial vein and the fibular vein to form the popliteal vein.
The posterior tibial vein drains the posterior surface of the tibia and joins the popliteal vein.
The fibular vein drains the muscles and integument in proximity to the fibula and also joins the popliteal vein.
The small saphenous vein located on the lateral surface of the leg drains blood from the superficial regions of the lower leg and foot, and flows into to the popliteal vein.
Development of Blood Vessels and Fetal Circulation
During those first few weeks, blood vessels begin to form from the embryonic mesoderm. The precursor cells are known as hemangioblasts.
Vascular tubes also develop on the blood islands, and they eventually connect to one another as well as to the developing, tubular heart.
This angiogenesis the creation of new blood vessels from existing ones continues as needed throughout life as we grow and develop.
Emerging from the placenta is the umbilical vein, which carries oxygen-rich blood from the mother to the fetal inferior vena cava via the ductus venosus to the heart that pumps it into fetal circulation.
The foramen ovale is an opening in the interatrial septum that allows blood to flow from the right atrium to the left atrium.
The ductus arteriosus is a short, muscular vessel that connects the pulmonary trunk to the aorta.
The ductus venosus is a temporary blood vessel that branches from the umbilical vein, allowing much of the freshly oxygenated blood from the placenta the organ of gas exchange between the mother and fetus to bypass the fetal liver and go directly to the fetal heart.
 Knowt
Knowt
