Other Subject
endocrine system
science
anatomy
Development and Aging of the Endocrine System
Reproductive Hormones
hormones
Structures of the Endocrine System
Types of Hormones
pituitary gland
hypothalamus
Thyroid Hormones
Hormones of the Pancreas
pancreas
Amine Hormones
Peptide and Protein Hormones
Steroid Hormones
Pathways of Hormone Action
Pathways Involving Intracellular Hormone Receptors
Factors Affecting Target Cell Response
Hypothalamus
Pituitary Gland
Oxytocin
Antidiuretic Hormone (ADH)
Anterior Pituitary
University/Undergrad

Chapter 17: The Endocrine System
Neural and Endocrine Signaling
The nervous system uses two types of intercellular communicatioN electrical and chemical signaling either by the direct action of an electrical potential, or in the latter case, through the action of chemical neurotransmitters such as serotonin or norepinephrine.
The endocrine system uses just one method of communication: chemical signaling.
These signals are sent by the endocrine organs, which secrete chemicals the hormone into the extracellular fluid.
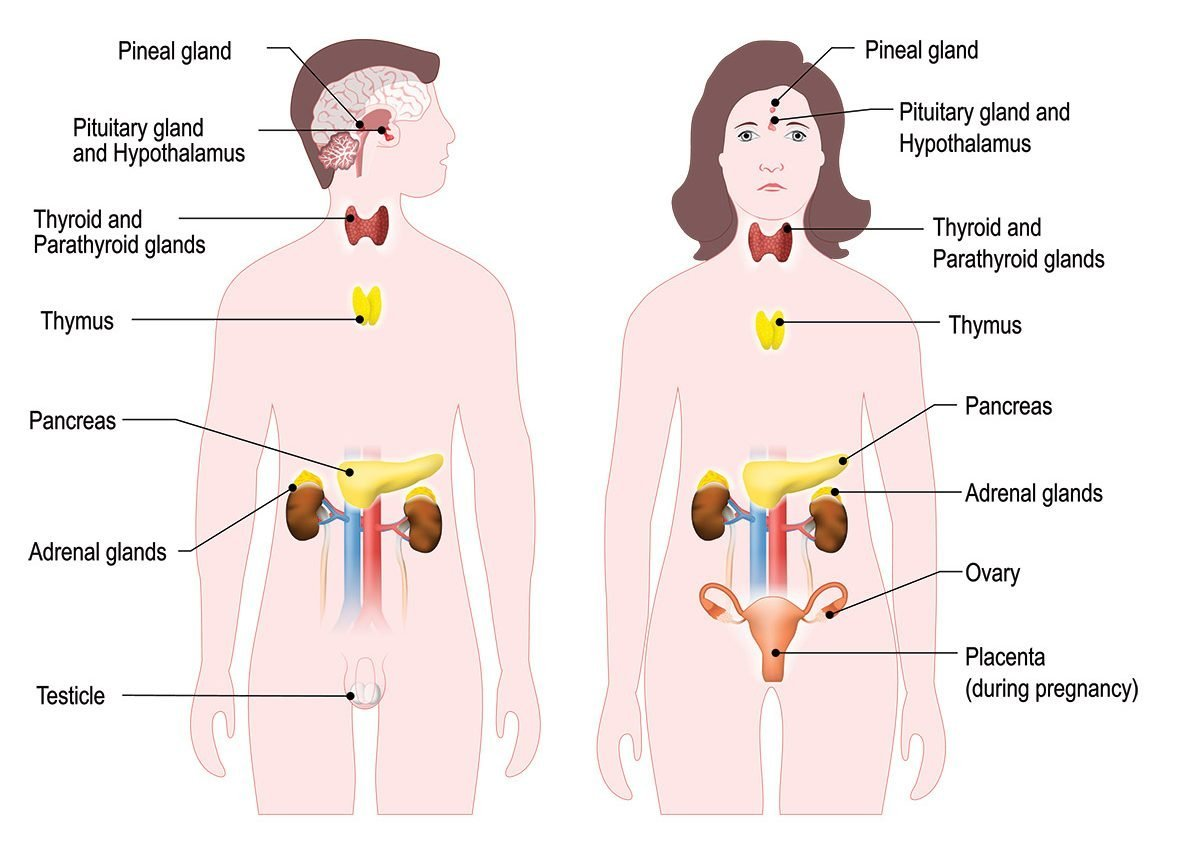
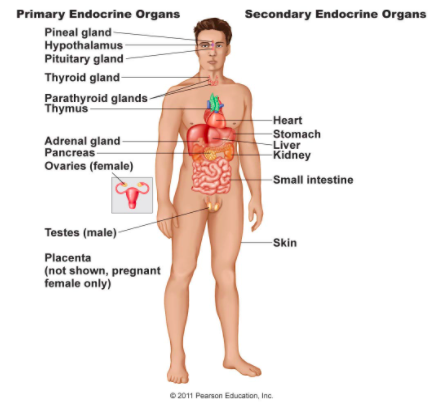
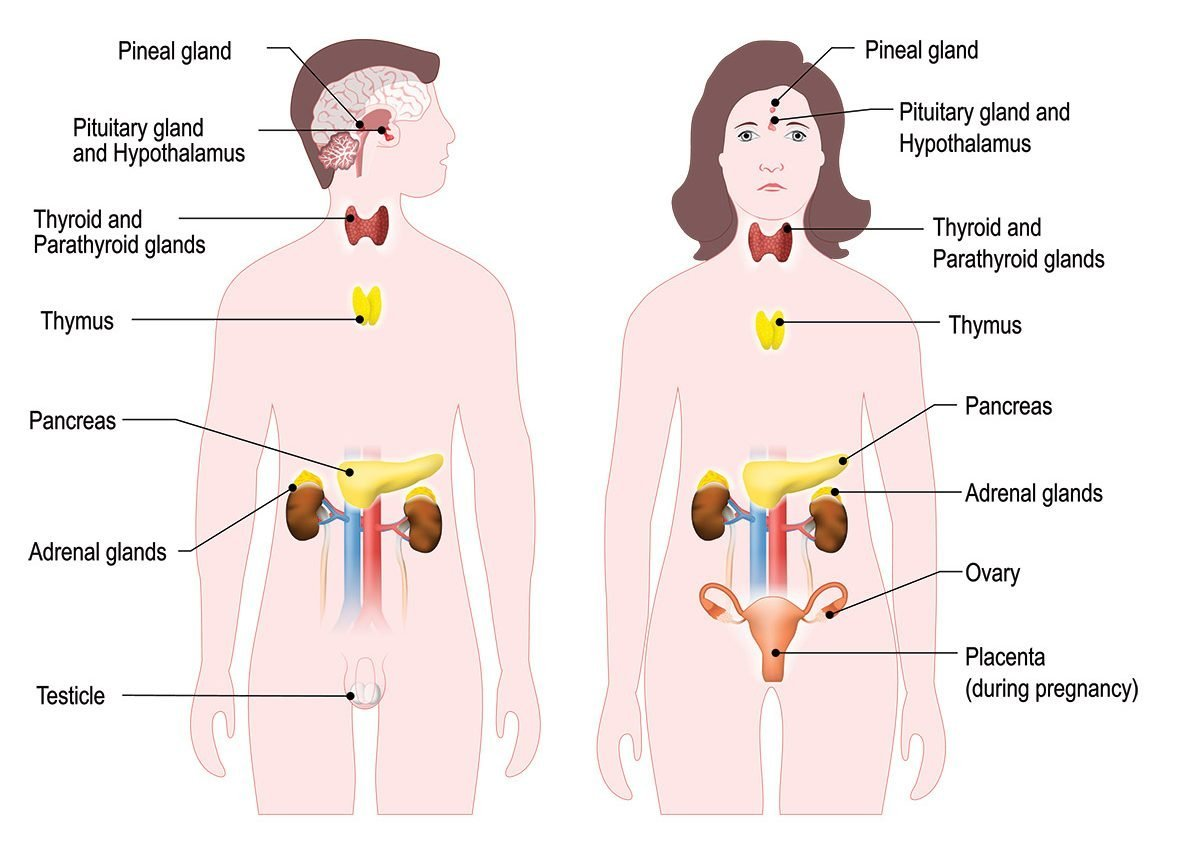
Structures of the Endocrine System
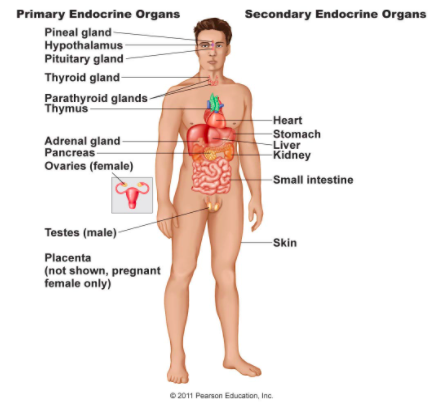
The endocrine system consists of cells, tissues, and organs that secrete hormones as a primary or secondary function.
The endocrine gland is the major player in this system.
The ductless endocrine glands are not to be confused with the body’s exocrine system, whose glands release their secretions through ducts.
An autocrine (auto-= “self”) is a chemical that elicits a response in the same cell that secreted it.
Local intercellular communication is the province of the paracrine, also called a paracrine factor, which is a chemical that induces a response in neighboring cells.
Types of Hormones
Amine Hormones
Hormones derived from the modification of amino acids are referred to as amine hormones.
Amine hormones are synthesized from the amino acids tryptophan or tyrosine.
Peptide and Protein Hormones: Peptide hormones consist of short chains of amino acids, whereas protein hormones are longer polypeptides.
Steroid Hormones
The primary hormones derived from lipids are steroids.
Steroid hormones are derived from the lipid cholesterol.
Pathways of Hormone Action
The message a hormone sends is received by a hormone receptor, a protein located either inside the cell or within the cell membrane.
Hormone receptors recognize molecules with specific shapes and side groups, and respond only to those hormones that are recognized.
Pathways Involving Intracellular Hormone Receptors
Intracellular hormone receptors are located inside the cell.
Hormones that bind to this type of receptor must be able to cross the cell membrane.
Steroid hormones are derived from cholesterol and therefore can readily diffuse through the lipid bilayer of the cell membrane to reach the intracellular receptor.
Pathways Involving Cell Membrane Hormone Receptors
Initiate a signaling cascade that is carried out by a molecule called a second messenger.
The second messenger used by most hormones is cyclic adenosine monophosphate (cAMP).
Factors Affecting Target Cell Response
When the level of a hormone is chronically reduced, target cells engage in upregulation to increase their number of receptors.
The three most common types of interaction are as follows:
The permissive effect, in which the presence of one hormone enables another hormone to act.
For example, thyroid hormones have complex permissive relationships with certain reproductive hormones.
A dietary deficiency of iodine, a component of thyroid hormones, can therefore affect reproductive system development and functioning.
The synergistic effect, in which two hormones with similar effects produce an amplified response.
In some cases, two hormones are required for an adequate response.
For example, two different reproductive hormones—FSH from the pituitary gland and estrogens from the ovaries—are required for the maturation of female ova (egg cells).
The antagonistic effect, in which two hormones have opposing effects.
A familiar example is the effect of two pancreatic hormones, insulin and glucagon.
Insulin increases the liver’s storage of glucose as glycogen, decreasing blood glucose, whereas glucagon stimulates the breakdown of glycogen stores, increasing blood glucose.
The Pituitary Gland and Hypothalamus
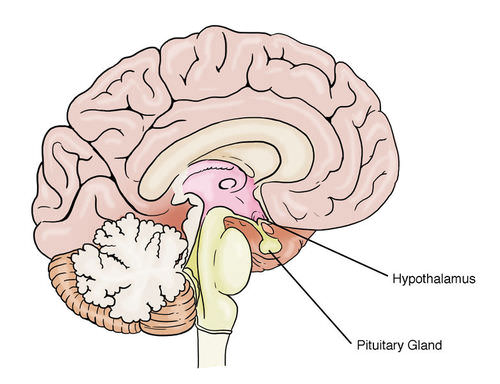
The hypothalamus–pituitary complex can be thought of as the “command center” of the endocrine system.
The hypothalamus is a structure of the diencephalon of the brain located anterior and inferior to the thalamus
In addition, the hypothalamus is anatomically and functionally related to the pituitary gland (or hypophysis), a bean-sized organ suspended from it by a stem called the infundibulum (or pituitary stalk).
Oxytocin: When fetal development is complete, the peptide-derived hormone oxytocin (tocia- = “childbirth”) stimulates uterine contractions and dilation of the cervix.
Antidiuretic Hormone (ADH)
Blood osmolarity is constantly monitored by osmoreceptors—specialized cells within the hypothalamus that are particularly sensitive to the concentration of sodium ions and other solutes.
In response to high blood osmolarity, which can occur during dehydration or following a very salty meal, the osmoreceptors signal the posterior pituitary to release antidiuretic hormone (ADH).
Anterior Pituitary
The anterior pituitary originates from the digestive tract in the embryo and migrates toward the brain during fetal development.
There are three regions: the pars distalis is the most anterior, the pars intermedia is adjacent to the posterior pituitary, and the pars tuberalis is a slender “tube” that wraps the infundibulum.
Within the infundibulum is a bridge of capillaries that connects the hypothalamus to the anterior pituitary.
This network, called the hypophyseal portal system, allows hypothalamic hormones to be transported to the anterior pituitary without first entering the systemic circulation.
Hormones produced by the anterior pituitary (in response to releasing hormones) enter a secondary capillary plexus, and from there drain into the circulation.
Growth Hormone
The endocrine system regulates the growth of the human body, protein synthesis, and cellular replication.
A major hormone involved in this process is growth hormone (GH), also called somatotropin—a protein hormone produced and secreted by the anterior pituitary gland.
GH indirectly mediates growth and protein synthesis by triggering the liver and other tissues to produce a group of proteins called insulin-like growth factors (IGFs).
Abnormally low levels of GH in children can cause growth impairment—a disorder called pituitary dwarfism (also known as growth hormone deficiency).
Thyroid-Stimulating Hormone
The activity of the thyroid gland is regulated by thyroid-stimulating hormone (TSH), also called thyrotropin.
Adrenocorticotropic Hormone
The adrenocorticotropic hormone (ACTH), also called corticotropin, stimulates the adrenal cortex (the more superficial “bark” of the adrenal glands) to secrete corticosteroid hormones such as cortisol.
Follicle-Stimulating Hormone and Luteinizing Hormone
GnRH stimulates the anterior pituitary to secrete gonadotropins hormones that regulate the function of the gonads.
The gonadotropins include two glycoprotein hormones: follicle-stimulating hormone (FSH) stimulates the production and maturation of sex cells, or gametes, including ova in women and sperm in men.
Luteinizing hormone (LH) triggers ovulation in women, as well as the production of estrogens and progesterone by the ovaries.
Prolactin: Prolactin (PRL) promotes lactation (milk production) in women.
The Thyroid Gland
A butterfly-shaped organ, the thyroid gland is located anterior to the trachea, just inferior to the larynx.
The follicles are made up of a central cavity filled with a sticky fluid called colloid.
Synthesis and Release of Thyroid Hormones
1. Binding of TSH to its receptors in the follicle cells of the thyroid gland causes the cells to actively transport iodide ions (I–) across their cell membrane, from the bloodstream into the cytosol.
As a result, the concentration of iodide ions “trapped” in the follicular cells is many times higher than the concentration in the bloodstream.
2. Iodide ions then move to the lumen of the follicle cells that border the colloid.
There, the ions undergo oxidation (their negatively charged electrons are removed).
The oxidation of two iodide ions (2 I–) results in iodine (I2), which passes through the follicle cell membrane into the colloid.
3. In the colloid, peroxidase enzymes link the iodine to the tyrosine amino acids in thyroglobulin to produce two intermediaries: a tyrosine attached to one iodine and a tyrosine attached to two iodines.
When one of each of these intermediaries is linked by covalent bonds, the resulting compound is triiodothyronine (T3), a thyroid hormone with three iodines.
Much more commonly, two copies of the second intermediary bond, forming tetraiodothyronine, also known as thyroxine (T4), a thyroid hormone with four iodines.
Thyroid Hormones
Associated hormones | Chemical class | Effect |
|---|---|---|
Thyroxine (T4), triiodothyronine (T3) | Amine | Stimulate basal metabolic rate |
Calcitonin | Peptide | Reduces blood Ca2+ levels |
The Parathyroid Glands
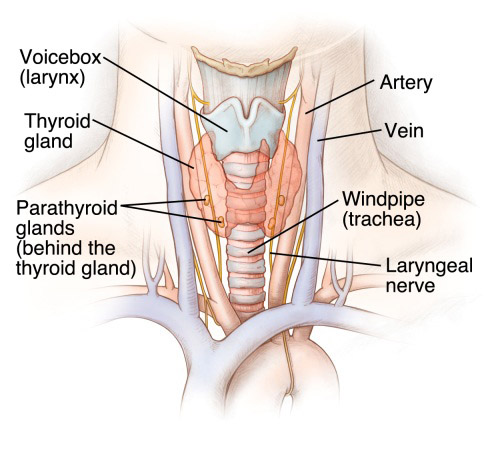
The parathyroid glands are tiny, round structures usually found embedded in the posterior surface of the thyroid gland.
These epithelial cells produce and secrete the parathyroid hormone (PTH), the major hormone involved in the regulation of blood calcium levels.
Abnormally high activity of the parathyroid gland can cause hyperparathyroidism, a disorder caused by an overproduction of PTH that results in excessive calcium reabsorption from bone.
Abnormally low blood calcium levels may be caused by parathyroid hormone deficiency, called hypoparathyroidism, which may develop following injury or surgery involving the thyroid gland.
The Adrenal Glands
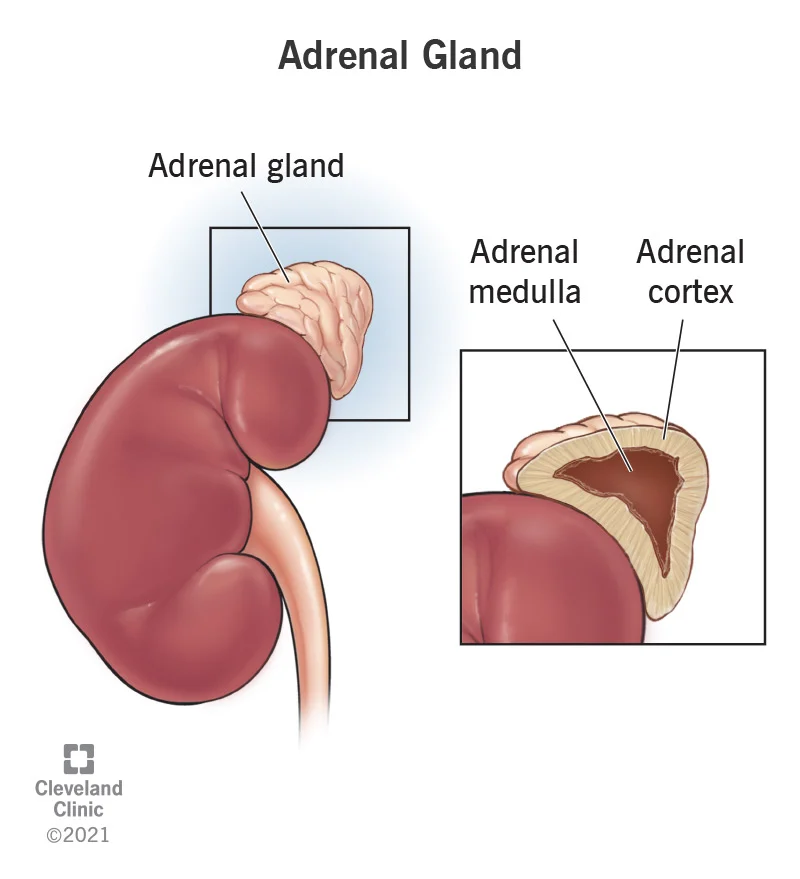
The adrenal glands are wedges of glandular and neuroendocrine tissue adhering to the top of the kidneys by a fibrous capsule.
The adrenal gland consists of an outer cortex of glandular tissue and an inner medulla of nervous tissue. The cortex itself is divided into three zones: the zona glomerulosa, the zona fasciculata, and the zona reticularis.
Each region secretes its own set of hormones.
The adrenal cortex, as a component of the hypothalamic-pituitary-adrenal (HPA) axis, secretes steroid hormones important for the regulation of the long-term stress response, blood pressure and blood volume, nutrient uptake and storage, fluid and electrolyte balance, and inflammation.
The adrenal medulla is neuroendocrine tissue composed of postganglionic sympathetic nervous system (SNS) neurons.
The body responds in different ways to short-term stress and long-term stress following a pattern known as the general adaptation syndrome (GAS).
Stage one of GAS is called the alarm reaction.
If the stress is not soon relieved, the body adapts to the stress in the second stage called the stage of resistance.
During the stage of exhaustion, individuals may begin to suffer depression, the suppression of their immune response, severe fatigue, or even a fatal heart attack.
Adrenal Cortex
The adrenal cortex consists of multiple layers of lipid-storing cells that occur in three structurally distinct regions.
Each of these regions produces different hormones.
Hormones of the Zona Glomerulosa
The most superficial region of the adrenal cortex is the zona glomerulosa, which produces a group of hormones collectively referred to as mineralocorticoids because of their effect on body minerals, especially sodium and potassium.
Aldosterone is the major mineralocorticoid.
Hormones of the Adrenal Glands
Adrenal gland | Associated hormones | Chemical class | Effect |
|---|---|---|---|
Adrenal cortex | Aldosterone | Steroid | Increases blood Na+levels |
Adrenal cortex | Cortisol, corticosterone, cortisone | Steroid | Increase blood glucose levels |
Adrenal medulla | Epinephrine, norepinephrine | Amine | Stimulate fight-or-flight response |
The Pineal Gland
Inferior but somewhat posterior to the thalamus is the pineal gland, a tiny endocrine gland whose functions are not entirely clear.
The pinealocyte cells that make up the pineal gland are known to produce and secrete the amine hormone melatonin, which is derived from serotonin.
Gonadal and Placental Hormones
The primary hormone produced by the male testes is testosterone, a steroid hormone important in the development of the male reproductive system, the maturation of sperm cells, and the development of male secondary sex characteristics such as a deepened voice, body hair, and increased muscle mass.
In addition, the testes produce the peptide hormone inhibin, which inhibits the secretion of FSH from the anterior pituitary gland.
FSH stimulates spermatogenesis.
The primary hormones produced by the ovaries are estrogens, which include estradiol, estriol, and estrone.
Another significant ovarian hormone is progesterone, which contributes to regulation of the menstrual cycle and is important in preparing the body for pregnancy as well as maintaining pregnancy.
Reproductive Hormones
Gonad | Associated hormones | Chemical class | Effect |
|---|---|---|---|
Testes | Testosterone | Steroid | Stimulates development of male secondary sexcharacteristics and sperm production |
Testes | Inhibin | Protein | Inhibits FSH release from pituitary |
Ovaries | Estrogens and progesterone | Steroid | Stimulate development of female secondary sexcharacteristics and prepare the body for childbirth |
Placenta | Human chorionic gonadotropin | Protein | Promotes progesterone synthesis during pregnancy and |
The Endocrine Pancreas
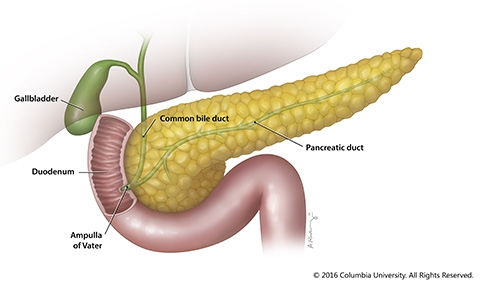
The pancreas is a long, slender organ, most of which is located posterior to the bottom half of the stomach.
Its pancreatic islets clusters of cells formerly known as the islets of Langerhans secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide (PP).
Cells and Secretions of the Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet.
Glucagon plays an important role in blood glucose regulation; low blood glucose levels stimulate its release.
The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet.
Elevated blood glucose levels stimulate the release of insulin.
The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin.
The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone.
Glucagon - Receptors in the pancreas can sense the decline in blood glucose levels, such as during periods of fasting or during prolonged labor or exercise.
Insulin
The primary function of insulin is to facilitate the uptake of glucose into body cells.
Precisely how insulin facilitates glucose uptake is not entirely clear.
Hormones of the Pancreas
Associated hormones | Chemical class | Effect |
|---|---|---|
Insulin (beta cells) | Protein | Reduces blood glucose levels |
Glucagon (alpha cells) | Protein | Increases blood glucose levels |
Somatostatin (delta cells) | Protein | Inhibits insulin and glucagon release |
Pancreatic polypeptide (PP cells) | Protein | Role in appetite |
Organs with Secondary Endocrine Functions
Heart
When the body experiences an increase in blood volume or pressure, the cells of the heart’s atrial wall stretch.
In response, specialized cells in the wall of the atria produce and secrete the peptide hormone atrial natriuretic peptide (ANP).
Gastrointestinal Tract
The endocrine cells of the GI tract are located in the mucosa of the stomach and small intestine.
Some of these hormones are secreted in response to eating a meal and aid in digestion.
Kidneys
The kidneys participate in several complex endocrine pathways and produce certain hormones. A decline in blood flow to the kidneys stimulates them to release the enzyme renin, triggering the renin-angiotensin-aldosterone (RAAS) system, and stimulating the reabsorption of sodium and water.
The reabsorption increases blood flow and blood pressure.
The kidneys produce the hormone erythropoietin (EPO) in response to low oxygen levels.
EPO stimulates the production of red blood cells (erythrocytes) in the bone marrow, thereby increasing oxygen delivery to tissues.
Skeleton: Although bone has long been recognized as a target for hormones, only recently have researchers recognized that the skeleton itself produces at least two hormones.
Adipose Tissue
Adipose tissue produces and secretes several hormones involved in lipid metabolism and storage.
One important example is leptin, a protein manufactured by adipose cells that circulates in amounts directly proportional to levels of body fat.
Skin
The skin functions as an endocrine organ in the production of the inactive form of vitamin D3, cholecalciferol.
When cholesterol present in the epidermis is exposed to ultraviolet radiation, it is converted to cholecalciferol, which then enters the blood.
Thymus
The thymus is an organ of the immune system that is larger and more active during infancy and early childhood, and begins to atrophy as we age.
Its endocrine function is the production of a group of hormones called thymosins that contribute to the development and differentiation of T lymphocytes, which are immune cells.
Liver
The liver is responsible for secreting at least four important hormones or hormone precursors: insulin-like growth factor (somatomedin), angiotensinogen, thrombopoetin, and hepcidin.
Development and Aging of the Endocrine System
The endocrine system arises from all three embryonic germ layers.
The pituitary gland arises from two distinct areas of the ectoderm: the anterior pituitary gland arises from the oral ectoderm, whereas the posterior pituitary gland arises from the neural ectoderm at the base of the hypothalamus.
As the body ages, changes occur that affect the endocrine system, sometimes altering the production, secretion, and catabolism of hormones.
Chapter 17: The Endocrine System
Neural and Endocrine Signaling
The nervous system uses two types of intercellular communicatioN electrical and chemical signaling either by the direct action of an electrical potential, or in the latter case, through the action of chemical neurotransmitters such as serotonin or norepinephrine.
The endocrine system uses just one method of communication: chemical signaling.
These signals are sent by the endocrine organs, which secrete chemicals the hormone into the extracellular fluid.
Structures of the Endocrine System
The endocrine system consists of cells, tissues, and organs that secrete hormones as a primary or secondary function.
The endocrine gland is the major player in this system.
The ductless endocrine glands are not to be confused with the body’s exocrine system, whose glands release their secretions through ducts.
An autocrine (auto-= “self”) is a chemical that elicits a response in the same cell that secreted it.
Local intercellular communication is the province of the paracrine, also called a paracrine factor, which is a chemical that induces a response in neighboring cells.
Types of Hormones
Amine Hormones
Hormones derived from the modification of amino acids are referred to as amine hormones.
Amine hormones are synthesized from the amino acids tryptophan or tyrosine.
Peptide and Protein Hormones: Peptide hormones consist of short chains of amino acids, whereas protein hormones are longer polypeptides.
Steroid Hormones
The primary hormones derived from lipids are steroids.
Steroid hormones are derived from the lipid cholesterol.
Pathways of Hormone Action
The message a hormone sends is received by a hormone receptor, a protein located either inside the cell or within the cell membrane.
Hormone receptors recognize molecules with specific shapes and side groups, and respond only to those hormones that are recognized.
Pathways Involving Intracellular Hormone Receptors
Intracellular hormone receptors are located inside the cell.
Hormones that bind to this type of receptor must be able to cross the cell membrane.
Steroid hormones are derived from cholesterol and therefore can readily diffuse through the lipid bilayer of the cell membrane to reach the intracellular receptor.
Pathways Involving Cell Membrane Hormone Receptors
Initiate a signaling cascade that is carried out by a molecule called a second messenger.
The second messenger used by most hormones is cyclic adenosine monophosphate (cAMP).
Factors Affecting Target Cell Response
When the level of a hormone is chronically reduced, target cells engage in upregulation to increase their number of receptors.
The three most common types of interaction are as follows:
The permissive effect, in which the presence of one hormone enables another hormone to act.
For example, thyroid hormones have complex permissive relationships with certain reproductive hormones.
A dietary deficiency of iodine, a component of thyroid hormones, can therefore affect reproductive system development and functioning.
The synergistic effect, in which two hormones with similar effects produce an amplified response.
In some cases, two hormones are required for an adequate response.
For example, two different reproductive hormones—FSH from the pituitary gland and estrogens from the ovaries—are required for the maturation of female ova (egg cells).
The antagonistic effect, in which two hormones have opposing effects.
A familiar example is the effect of two pancreatic hormones, insulin and glucagon.
Insulin increases the liver’s storage of glucose as glycogen, decreasing blood glucose, whereas glucagon stimulates the breakdown of glycogen stores, increasing blood glucose.
The Pituitary Gland and Hypothalamus
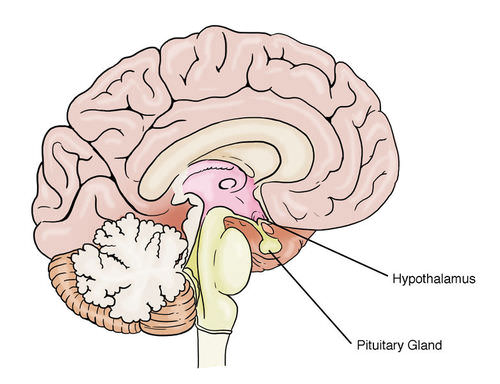
The hypothalamus–pituitary complex can be thought of as the “command center” of the endocrine system.
The hypothalamus is a structure of the diencephalon of the brain located anterior and inferior to the thalamus
In addition, the hypothalamus is anatomically and functionally related to the pituitary gland (or hypophysis), a bean-sized organ suspended from it by a stem called the infundibulum (or pituitary stalk).
Oxytocin: When fetal development is complete, the peptide-derived hormone oxytocin (tocia- = “childbirth”) stimulates uterine contractions and dilation of the cervix.
Antidiuretic Hormone (ADH)
Blood osmolarity is constantly monitored by osmoreceptors—specialized cells within the hypothalamus that are particularly sensitive to the concentration of sodium ions and other solutes.
In response to high blood osmolarity, which can occur during dehydration or following a very salty meal, the osmoreceptors signal the posterior pituitary to release antidiuretic hormone (ADH).
Anterior Pituitary
The anterior pituitary originates from the digestive tract in the embryo and migrates toward the brain during fetal development.
There are three regions: the pars distalis is the most anterior, the pars intermedia is adjacent to the posterior pituitary, and the pars tuberalis is a slender “tube” that wraps the infundibulum.
Within the infundibulum is a bridge of capillaries that connects the hypothalamus to the anterior pituitary.
This network, called the hypophyseal portal system, allows hypothalamic hormones to be transported to the anterior pituitary without first entering the systemic circulation.
Hormones produced by the anterior pituitary (in response to releasing hormones) enter a secondary capillary plexus, and from there drain into the circulation.
Growth Hormone
The endocrine system regulates the growth of the human body, protein synthesis, and cellular replication.
A major hormone involved in this process is growth hormone (GH), also called somatotropin—a protein hormone produced and secreted by the anterior pituitary gland.
GH indirectly mediates growth and protein synthesis by triggering the liver and other tissues to produce a group of proteins called insulin-like growth factors (IGFs).
Abnormally low levels of GH in children can cause growth impairment—a disorder called pituitary dwarfism (also known as growth hormone deficiency).
Thyroid-Stimulating Hormone
The activity of the thyroid gland is regulated by thyroid-stimulating hormone (TSH), also called thyrotropin.
Adrenocorticotropic Hormone
The adrenocorticotropic hormone (ACTH), also called corticotropin, stimulates the adrenal cortex (the more superficial “bark” of the adrenal glands) to secrete corticosteroid hormones such as cortisol.
Follicle-Stimulating Hormone and Luteinizing Hormone
GnRH stimulates the anterior pituitary to secrete gonadotropins hormones that regulate the function of the gonads.
The gonadotropins include two glycoprotein hormones: follicle-stimulating hormone (FSH) stimulates the production and maturation of sex cells, or gametes, including ova in women and sperm in men.
Luteinizing hormone (LH) triggers ovulation in women, as well as the production of estrogens and progesterone by the ovaries.
Prolactin: Prolactin (PRL) promotes lactation (milk production) in women.
The Thyroid Gland
A butterfly-shaped organ, the thyroid gland is located anterior to the trachea, just inferior to the larynx.
The follicles are made up of a central cavity filled with a sticky fluid called colloid.
Synthesis and Release of Thyroid Hormones
1. Binding of TSH to its receptors in the follicle cells of the thyroid gland causes the cells to actively transport iodide ions (I–) across their cell membrane, from the bloodstream into the cytosol.
As a result, the concentration of iodide ions “trapped” in the follicular cells is many times higher than the concentration in the bloodstream.
2. Iodide ions then move to the lumen of the follicle cells that border the colloid.
There, the ions undergo oxidation (their negatively charged electrons are removed).
The oxidation of two iodide ions (2 I–) results in iodine (I2), which passes through the follicle cell membrane into the colloid.
3. In the colloid, peroxidase enzymes link the iodine to the tyrosine amino acids in thyroglobulin to produce two intermediaries: a tyrosine attached to one iodine and a tyrosine attached to two iodines.
When one of each of these intermediaries is linked by covalent bonds, the resulting compound is triiodothyronine (T3), a thyroid hormone with three iodines.
Much more commonly, two copies of the second intermediary bond, forming tetraiodothyronine, also known as thyroxine (T4), a thyroid hormone with four iodines.
Thyroid Hormones
Associated hormones | Chemical class | Effect |
|---|---|---|
Thyroxine (T4), triiodothyronine (T3) | Amine | Stimulate basal metabolic rate |
Calcitonin | Peptide | Reduces blood Ca2+ levels |
The Parathyroid Glands
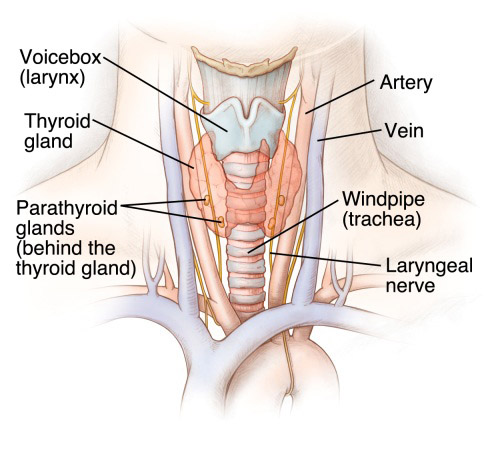
The parathyroid glands are tiny, round structures usually found embedded in the posterior surface of the thyroid gland.
These epithelial cells produce and secrete the parathyroid hormone (PTH), the major hormone involved in the regulation of blood calcium levels.
Abnormally high activity of the parathyroid gland can cause hyperparathyroidism, a disorder caused by an overproduction of PTH that results in excessive calcium reabsorption from bone.
Abnormally low blood calcium levels may be caused by parathyroid hormone deficiency, called hypoparathyroidism, which may develop following injury or surgery involving the thyroid gland.
The Adrenal Glands
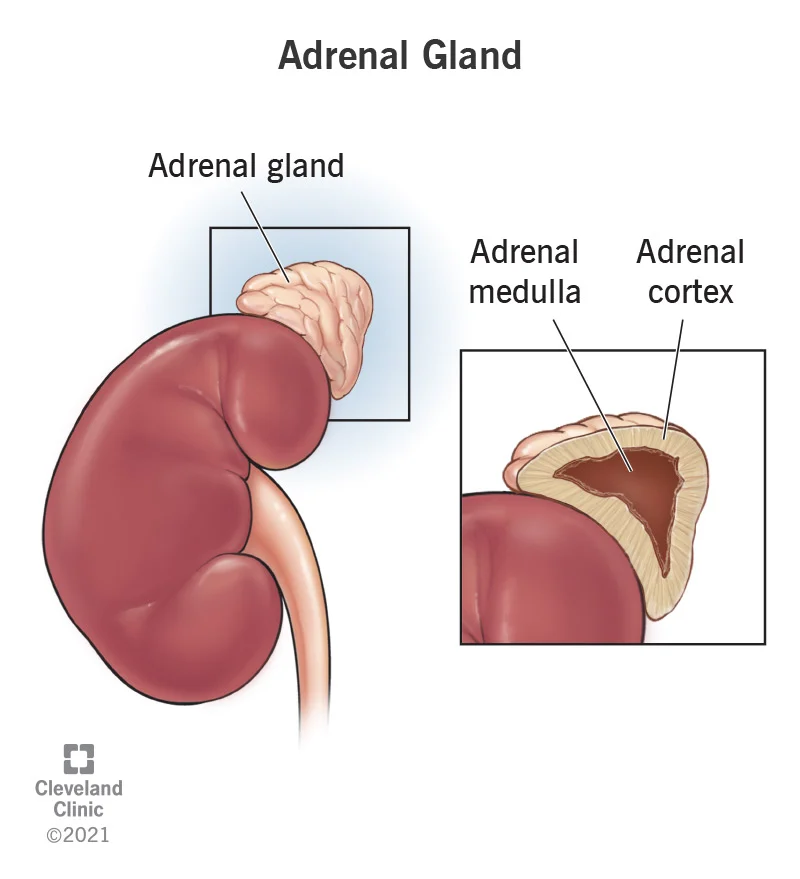
The adrenal glands are wedges of glandular and neuroendocrine tissue adhering to the top of the kidneys by a fibrous capsule.
The adrenal gland consists of an outer cortex of glandular tissue and an inner medulla of nervous tissue. The cortex itself is divided into three zones: the zona glomerulosa, the zona fasciculata, and the zona reticularis.
Each region secretes its own set of hormones.
The adrenal cortex, as a component of the hypothalamic-pituitary-adrenal (HPA) axis, secretes steroid hormones important for the regulation of the long-term stress response, blood pressure and blood volume, nutrient uptake and storage, fluid and electrolyte balance, and inflammation.
The adrenal medulla is neuroendocrine tissue composed of postganglionic sympathetic nervous system (SNS) neurons.
The body responds in different ways to short-term stress and long-term stress following a pattern known as the general adaptation syndrome (GAS).
Stage one of GAS is called the alarm reaction.
If the stress is not soon relieved, the body adapts to the stress in the second stage called the stage of resistance.
During the stage of exhaustion, individuals may begin to suffer depression, the suppression of their immune response, severe fatigue, or even a fatal heart attack.
Adrenal Cortex
The adrenal cortex consists of multiple layers of lipid-storing cells that occur in three structurally distinct regions.
Each of these regions produces different hormones.
Hormones of the Zona Glomerulosa
The most superficial region of the adrenal cortex is the zona glomerulosa, which produces a group of hormones collectively referred to as mineralocorticoids because of their effect on body minerals, especially sodium and potassium.
Aldosterone is the major mineralocorticoid.
Hormones of the Adrenal Glands
Adrenal gland | Associated hormones | Chemical class | Effect |
|---|---|---|---|
Adrenal cortex | Aldosterone | Steroid | Increases blood Na+levels |
Adrenal cortex | Cortisol, corticosterone, cortisone | Steroid | Increase blood glucose levels |
Adrenal medulla | Epinephrine, norepinephrine | Amine | Stimulate fight-or-flight response |
The Pineal Gland
Inferior but somewhat posterior to the thalamus is the pineal gland, a tiny endocrine gland whose functions are not entirely clear.
The pinealocyte cells that make up the pineal gland are known to produce and secrete the amine hormone melatonin, which is derived from serotonin.
Gonadal and Placental Hormones
The primary hormone produced by the male testes is testosterone, a steroid hormone important in the development of the male reproductive system, the maturation of sperm cells, and the development of male secondary sex characteristics such as a deepened voice, body hair, and increased muscle mass.
In addition, the testes produce the peptide hormone inhibin, which inhibits the secretion of FSH from the anterior pituitary gland.
FSH stimulates spermatogenesis.
The primary hormones produced by the ovaries are estrogens, which include estradiol, estriol, and estrone.
Another significant ovarian hormone is progesterone, which contributes to regulation of the menstrual cycle and is important in preparing the body for pregnancy as well as maintaining pregnancy.
Reproductive Hormones
Gonad | Associated hormones | Chemical class | Effect |
|---|---|---|---|
Testes | Testosterone | Steroid | Stimulates development of male secondary sexcharacteristics and sperm production |
Testes | Inhibin | Protein | Inhibits FSH release from pituitary |
Ovaries | Estrogens and progesterone | Steroid | Stimulate development of female secondary sexcharacteristics and prepare the body for childbirth |
Placenta | Human chorionic gonadotropin | Protein | Promotes progesterone synthesis during pregnancy and |
The Endocrine Pancreas
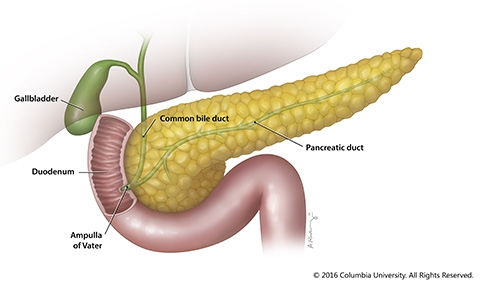
The pancreas is a long, slender organ, most of which is located posterior to the bottom half of the stomach.
Its pancreatic islets clusters of cells formerly known as the islets of Langerhans secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide (PP).
Cells and Secretions of the Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet.
Glucagon plays an important role in blood glucose regulation; low blood glucose levels stimulate its release.
The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet.
Elevated blood glucose levels stimulate the release of insulin.
The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin.
The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone.
Glucagon - Receptors in the pancreas can sense the decline in blood glucose levels, such as during periods of fasting or during prolonged labor or exercise.
Insulin
The primary function of insulin is to facilitate the uptake of glucose into body cells.
Precisely how insulin facilitates glucose uptake is not entirely clear.
Hormones of the Pancreas
Associated hormones | Chemical class | Effect |
|---|---|---|
Insulin (beta cells) | Protein | Reduces blood glucose levels |
Glucagon (alpha cells) | Protein | Increases blood glucose levels |
Somatostatin (delta cells) | Protein | Inhibits insulin and glucagon release |
Pancreatic polypeptide (PP cells) | Protein | Role in appetite |
Organs with Secondary Endocrine Functions
Heart
When the body experiences an increase in blood volume or pressure, the cells of the heart’s atrial wall stretch.
In response, specialized cells in the wall of the atria produce and secrete the peptide hormone atrial natriuretic peptide (ANP).
Gastrointestinal Tract
The endocrine cells of the GI tract are located in the mucosa of the stomach and small intestine.
Some of these hormones are secreted in response to eating a meal and aid in digestion.
Kidneys
The kidneys participate in several complex endocrine pathways and produce certain hormones. A decline in blood flow to the kidneys stimulates them to release the enzyme renin, triggering the renin-angiotensin-aldosterone (RAAS) system, and stimulating the reabsorption of sodium and water.
The reabsorption increases blood flow and blood pressure.
The kidneys produce the hormone erythropoietin (EPO) in response to low oxygen levels.
EPO stimulates the production of red blood cells (erythrocytes) in the bone marrow, thereby increasing oxygen delivery to tissues.
Skeleton: Although bone has long been recognized as a target for hormones, only recently have researchers recognized that the skeleton itself produces at least two hormones.
Adipose Tissue
Adipose tissue produces and secretes several hormones involved in lipid metabolism and storage.
One important example is leptin, a protein manufactured by adipose cells that circulates in amounts directly proportional to levels of body fat.
Skin
The skin functions as an endocrine organ in the production of the inactive form of vitamin D3, cholecalciferol.
When cholesterol present in the epidermis is exposed to ultraviolet radiation, it is converted to cholecalciferol, which then enters the blood.
Thymus
The thymus is an organ of the immune system that is larger and more active during infancy and early childhood, and begins to atrophy as we age.
Its endocrine function is the production of a group of hormones called thymosins that contribute to the development and differentiation of T lymphocytes, which are immune cells.
Liver
The liver is responsible for secreting at least four important hormones or hormone precursors: insulin-like growth factor (somatomedin), angiotensinogen, thrombopoetin, and hepcidin.
Development and Aging of the Endocrine System
The endocrine system arises from all three embryonic germ layers.
The pituitary gland arises from two distinct areas of the ectoderm: the anterior pituitary gland arises from the oral ectoderm, whereas the posterior pituitary gland arises from the neural ectoderm at the base of the hypothalamus.
As the body ages, changes occur that affect the endocrine system, sometimes altering the production, secretion, and catabolism of hormones.
 Knowt
Knowt