
Chapter 16: Identification of Vaginal Secretions and Menstrual Blood
16.1: Identification of Vaginal Stratified Squamous Epithelial Cells
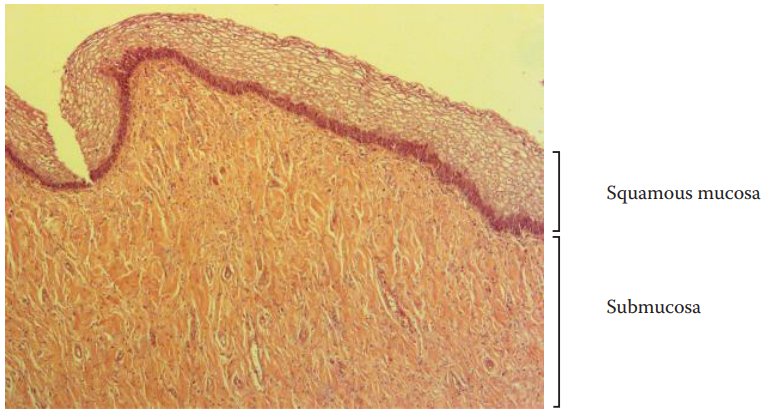
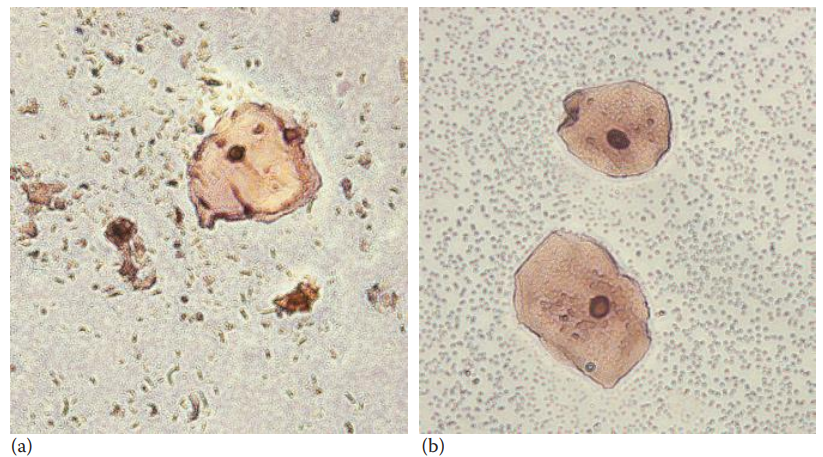
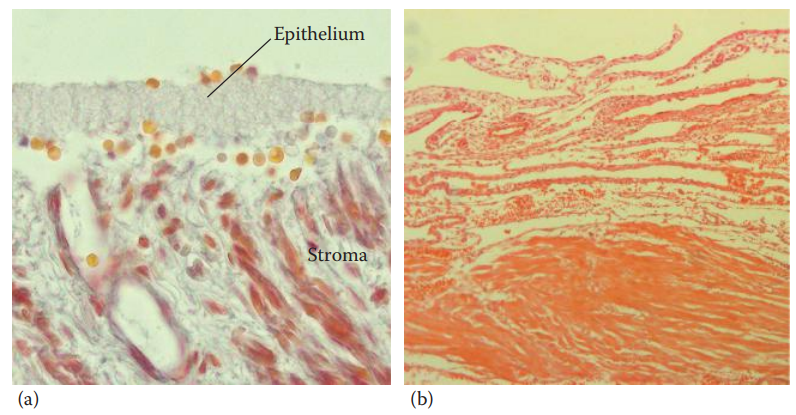
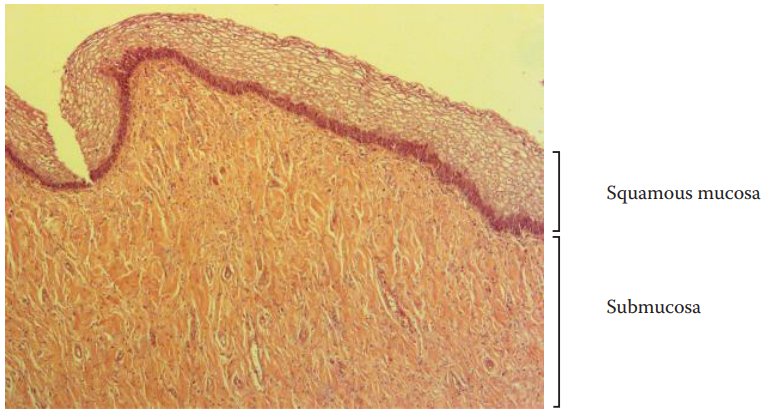
A normal human vagina is covered by the squamous mucosa, which is composed of stratified squamous epithelial tissue.
Lying under the squamous mucosa is the submucosa, which contains an abundance of connective tissue and capillaries.
Below the submucosa is the muscularis, which is made up of smooth muscle.
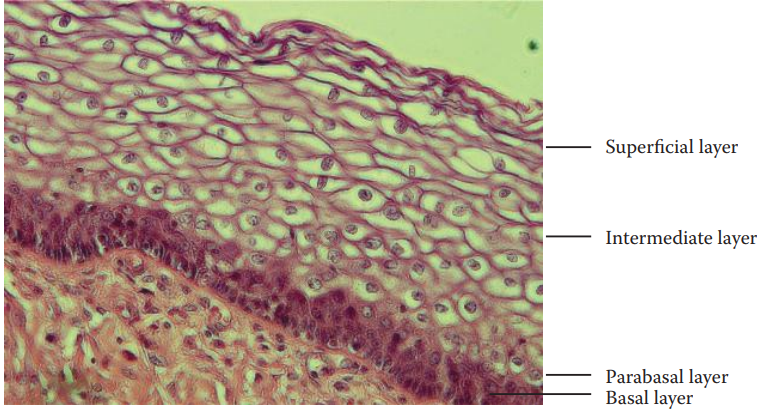
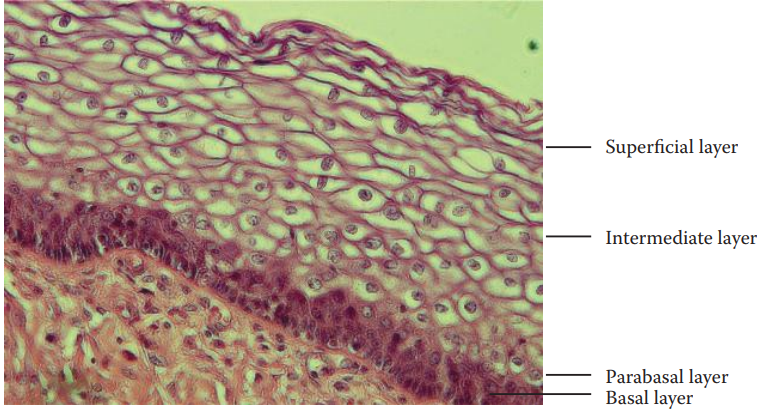
The squamous mucosa consists of multiple layers of cells:
Basal Layer: In this layer, basal cells are anchored to the basement membrane that separates the squamous mucosa from the submucosa.
Basal Cells: Are small in size with relatively large nuclei and are highly proliferative.
Parabasal Layer: This is where cells undergo differentiation.
Intermediate Layer: The cells are flattened and their nuclei are compressed.
Superficial Layer: This is where the cells are fully differentiated with small and dense nuclei.
Lugol’s Iodine Staining and Periodic Acid–Schiff Method
Lugol’s iodine solution: Named after the French physician Jean Lugol, is originally used as an antiseptic that is applied to skin or tissue to prevent infection.
It is utilized for the identification of glycogenated vaginal epithelial cells.
The technique is based on the principle that iodine reacts with intracellular glycogen to exhibit a color.
Glycogen is the principal storage form of glucose in animal and human cells and is found in the granules in the cytoplasm of the cells of many tissues.
In addition to squamous epithelial cells, glycogen is also found in hepatocytes, which have the highest glycogen content, as well as muscle cells.
Lugol’s stock solution is an aqueous solution of 5% iodine (I2) and 10% potassium iodide (KI).
Potassium iodide allows the iodine to be soluble in water through the formation of the triiodide ion.
Dane’s Staining Method
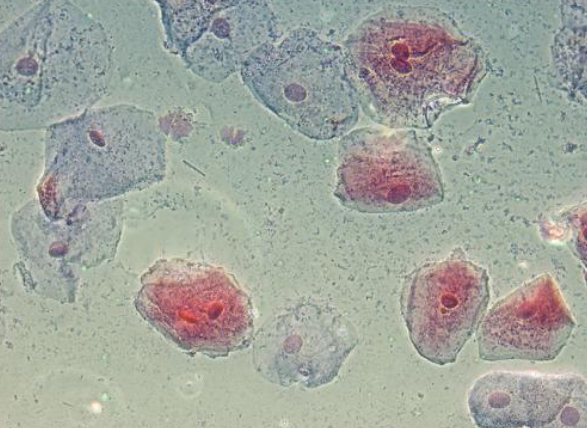
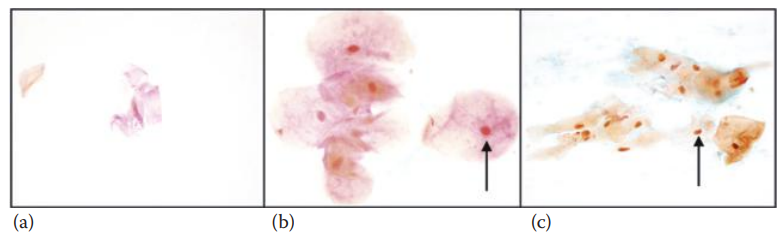
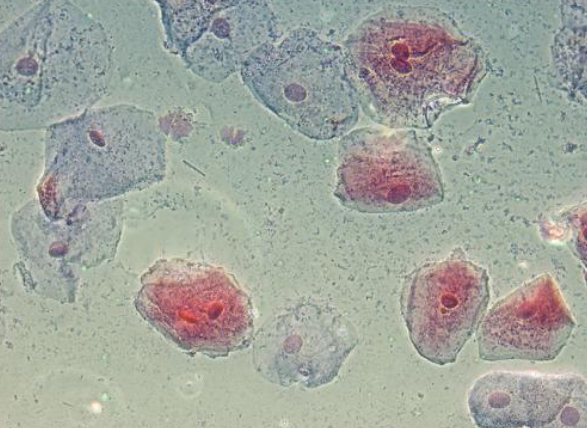
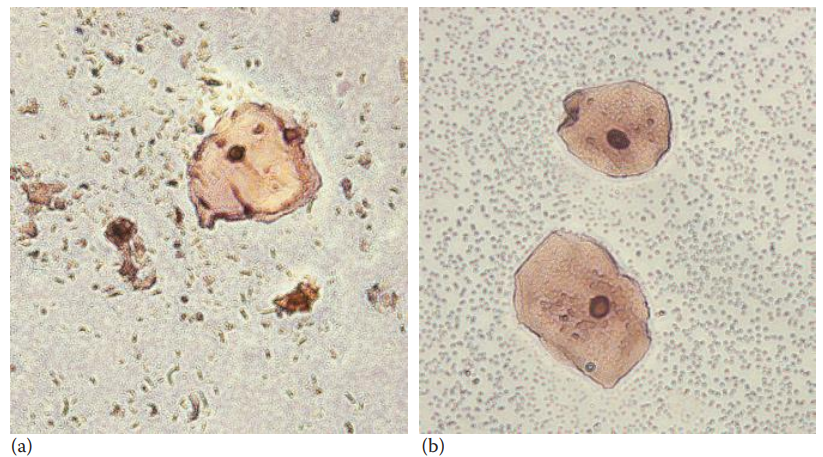
Skin, buccal, and vaginal epithelial cells belong to stratified squamous epithelium.
Differentiated skin epithelial cells are keratinized and are classified as keratinizing squamous epithelial cells, while buccal and vaginal epithelial cells are nonkeratinizing squamous epithelial cells.
The skin epithelial cells lose nuclei and other cellular organelles during differentiation.
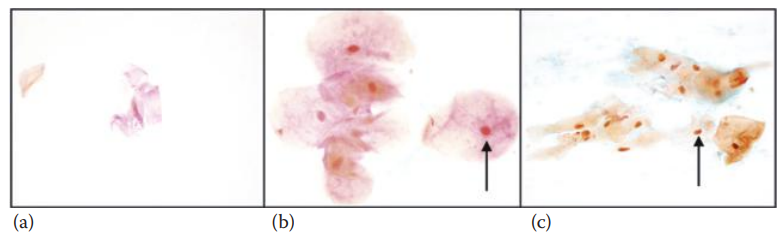
Dane’s staining method has been developed to distinguish all three types of cells.
Skin cells are stained red and orange;
Buccal cells are stained predominantly orange-pink with red nuclei; and
Vaginal cells are stained bright orange with orange nuclei.
16.2: Identification of Vaginal Acid Phosphatase
Acid phosphatases are a group of enzymes that are capable of hydrolyzing a variety of small organic phosphomonoesters under acidic conditions.
Five different acid phosphatase isoenzymes identified in human tissues:
erythroid acid phosphatase;
lysosomal acid phosphatase;
prostate acid phosphatase;
macrophage acid phosphatase;
testicular acid phosphatase.
Human prostatic acid phosphatase is found in large quantities in seminal fluid and is used as a biomarker for semen identification.
Prostatic acid phosphatase: A homodimer containing two identical subunits with a molecular weight of 50 kDa. Small amounts of acid phosphatase can be detected in vaginal fluid, which is produced in normal cervical epithelial cells.
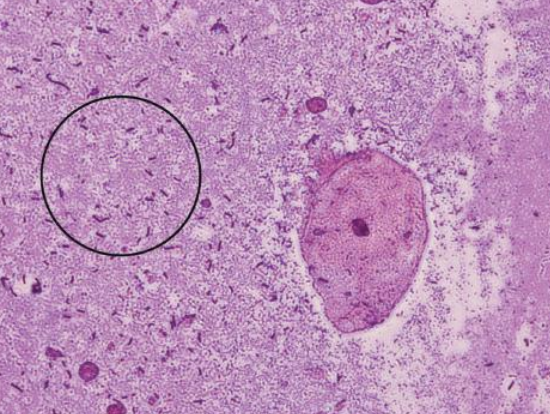
16.3: Identification of Vaginal Bacteria
Lactobacillus: It can be found in the respiratory, the gastrointestinal, and the urogenital tract of healthy humans and animals.
Lactobacillus taxa: These are the predominant bacteria in the vagina of women of reproductive age, and they play an important role in protecting the host against invasive pathogenic organisms.
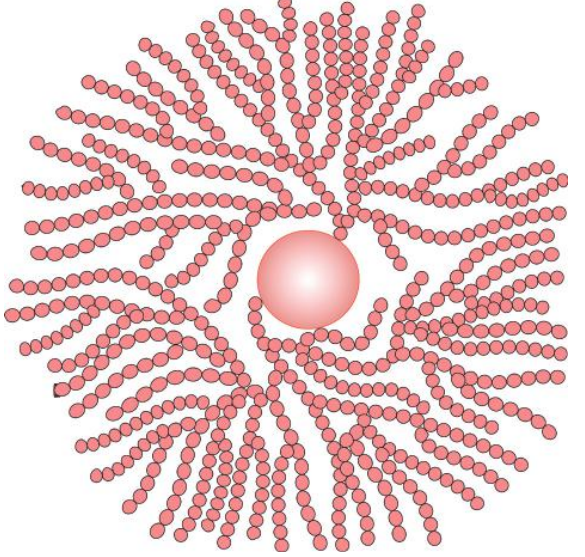
Lactobacillus consists of rod-shaped, nonmotile, and non-spore-forming gram-positive bacteria.
Lactobacillus bacteria produce lactic acid.
16.4: Outlook for Confirmatory Assays of Vaginal Secretions
Nondestructive confirmatory identification methods such as fluorescence spectroscopy and Raman spectroscopy can potentially be useful for the identification of vaginal secretions.
The analysis of tissue-specific gene expression has been utilized for the identification of vaginal secretions.
Using the reverse transcription polymerase chain reaction (RT-PCR) technique, the mRNAs of the tissue-specific genes of vaginal epithelial cells can be detected.
The commonly used markers for vaginal secretion identification are:
MUC4: Encodes a mucin protein that is a major component of vaginal mucus.
HBD1: Encodes a vaginal antimicrobial peptide.
16.5: Menstruation
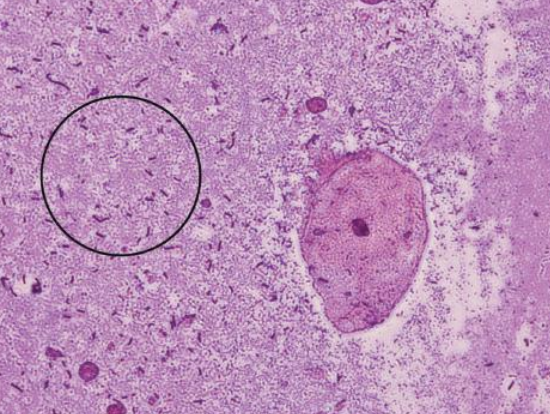
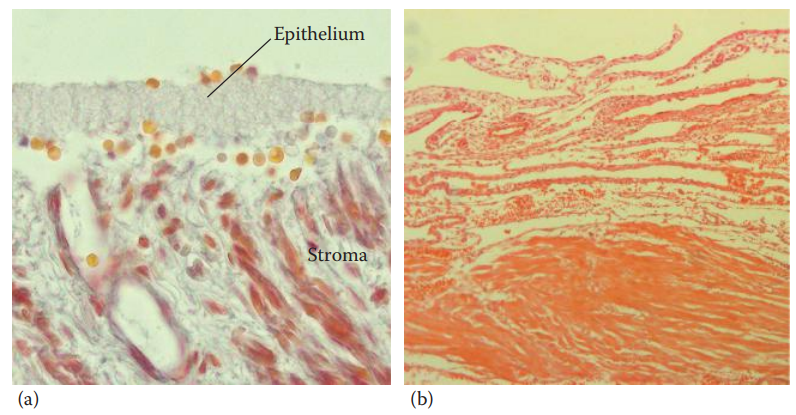
Menstruation: The periodic discharge of blood and the elimination of the degenerated lining of the endometrium from the uterus of nonpregnant women.
From menarche to menopause, women may menstruate up to 400 times during their reproductive age.
The uterus plays an important role in preparing the uterine endometrium for the possible implantation of a developing embryo.
The linings of the uterus are composed of the myometrium and the endometrium.
Myometrium: Consists of the muscle fibers of the uterus.
Endometrium: Consists of the simple columnar epithelium and the stroma.
The endometrium consists of the simple columnar epithelium and the stroma.
Simple columnar epithelium: Formed by single-layered elongated cells located at the apical surface of the endometrium.
Stroma: It consists of connective tissues as well as spiral arteries.
Spiral arteries: These are small arteries that ascend through the endometrium and form a coil-like structure, which supplies blood to the endometrium.
Representative Markers of mRNA-Based Assays for Vaginal Secretions and Menstrual Blood Identification
Vaginal Secretions:
CYP2B7P1: Cytochrome P450, family 2, subfamily B, polypeptide 7, pseudogene 1.
DKK4: Dickkopf homolog 4
FUT6: Fucosyltransferase 6
HBD1: β Defensin 1
IL19: Interleukin 19
MUC4: Mucin 4
MYOZ1: Myozenin 1
SFTA2: Surfactant associated 2
Menstrual blood:
MMP7: Matrix metalloproteinase 7
MMP11: Matrix metalloproteinase 11
miRNA Markers for Vaginal Secretions and Menstrual Blood Identification
Vaginal secretions:
miR124a: UAAGGCACGCGGUGAAUGCC
miR372: AAAGUGCUGCGACAUUUGAGCGU
miR617: AGACUUCCCAUUUGAAGGUGGC
miR891a: UGCAACGAACCUGAGCCACUGA
Menstrual Blood:
miR214: UGCCUGUCUACACUUGCUGUGC
miR412: ACUUCACCUGGUCCACUAGCCGU
miR451: AAACCGUUACCAUUACUGAGUU
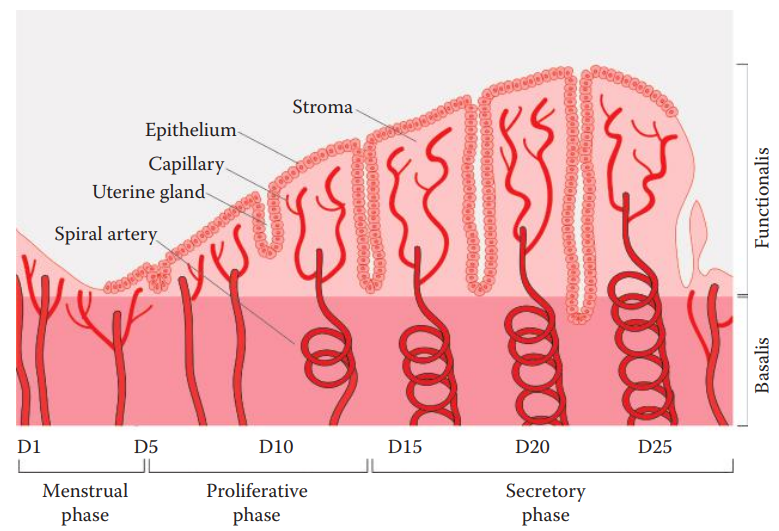
Uterine Cycle
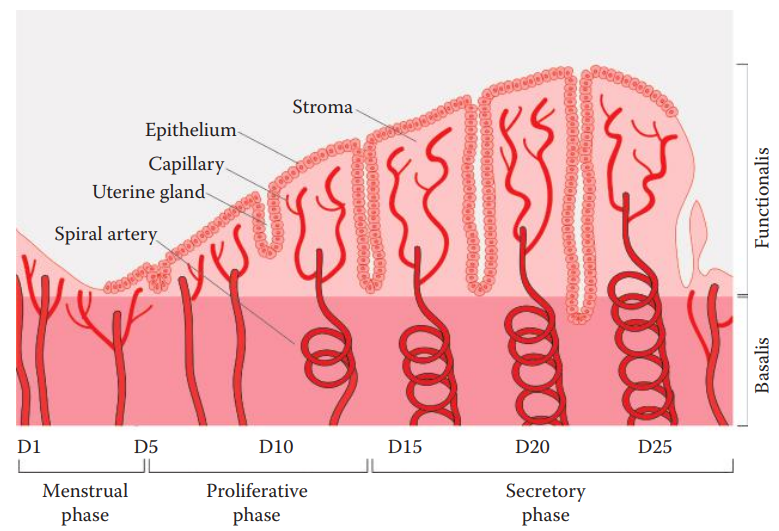
The endometrium can be divided into two zones:
Functionalis: The luminal part of the endometrium. It is the zone of cyclic changes in the endometrium and is shed during menstruation.
Basalis: The basal part of the endometrium and is not shed during menstruation. This zone produces cells to regenerate the functionalis during the next cycle.
During the uterine cycle, repetitive physiological changes occur in the functionalis.
The cycle is divided into three phases:
During the menstrual phase, the functionalis degenerates and is sloughed off from the uterine wall and bleeding occurs, known as menses.
During the proliferative phase, the functionalis begins regeneration in which the spiral arteries are proliferated.
During the secretory phase, the spiral arteries are further developed and coiled.
In the absence of pregnancy, a decrease in the progesterone level leads to the constriction of the spiral arteries. As a result, the functionalis becomes ischemic, leading to hypoxia.
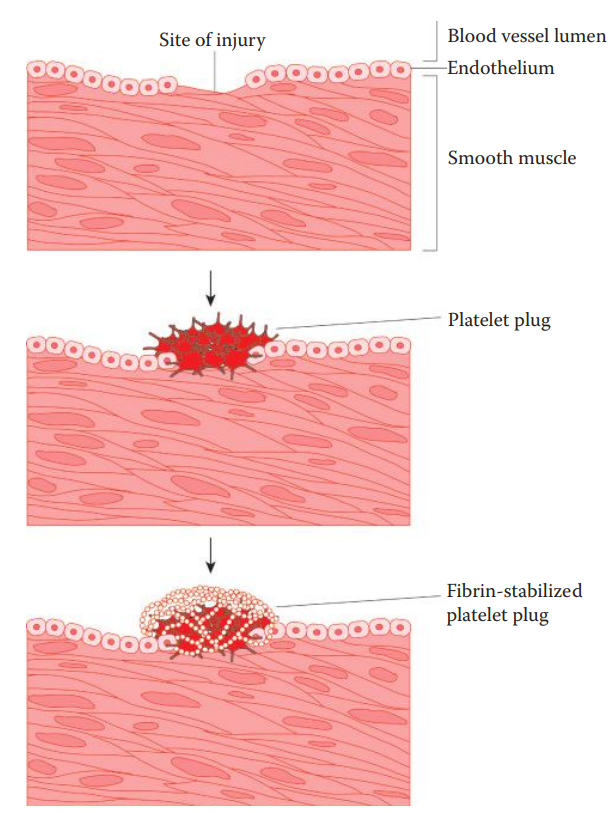
Uterine Endometrial Hemostasis
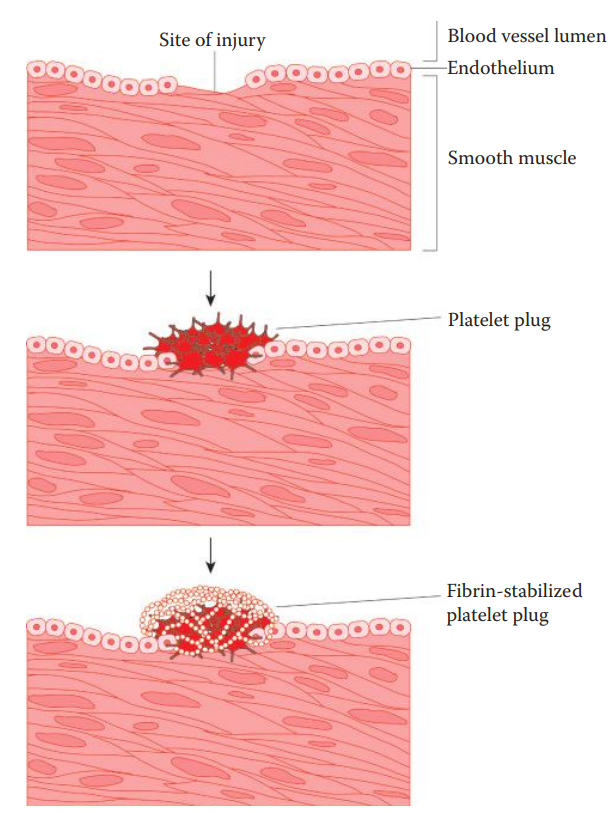
The cessation of menstrual bleeding is achieved by endometrial hemostasis that is initiated when injury occurs due to the shedding of the endometrium.
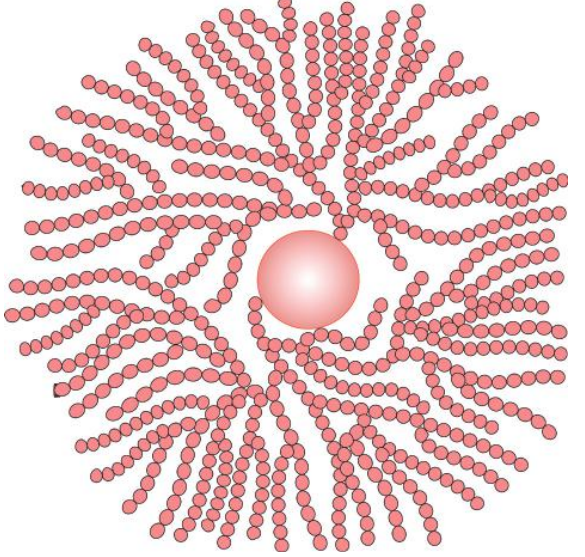
Hemostasis begins with platelet activation and aggregation to form platelet plugs at the site of injury.
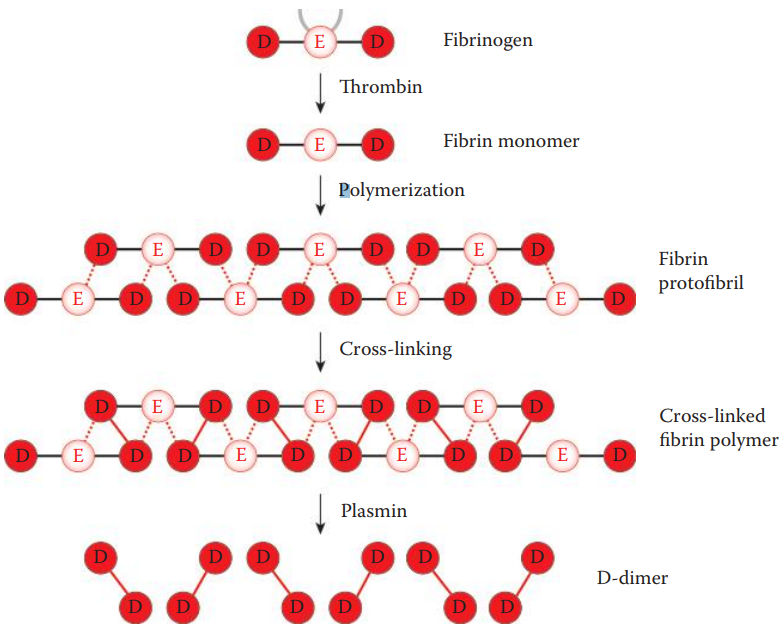
The blood coagulation cascade is activated to produce thrombin.
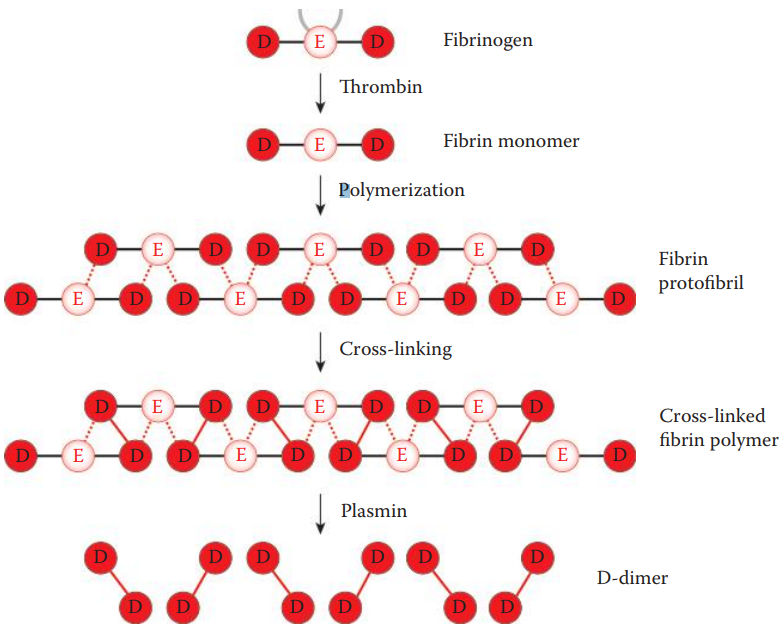
Thrombin: A serine protease, converts soluble fibrinogen into fibrin.
Fibrin: A protein involved in blood clotting, aggregates with the platelet plugs and leads to the cessation of bleeding by forming blood clots, known as thrombi.
Under normal physiological conditions, uterine endometrial hemostasis is a balanced process between blood coagulation and clot dissolution to control blood loss and to prevent clot accumulation within the uterus.
Blood clots are prevented from accumulating during menstruation by forming low amounts of platelet plugs and synthesizing coagulation factor inhibitors that inhibit blood coagulation.
Fibrinolysis is activated, during which the thrombus is broken down by a protease known as plasmin. Plasmin cleaves fibrin, generating soluble degradation products.
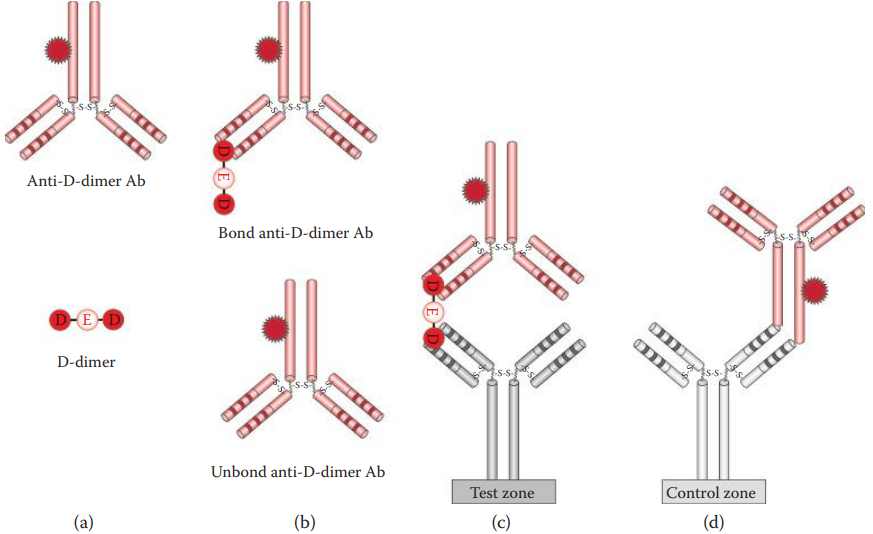
16.6: D-dimer Assay
D-dimer: A degradation product produced during fibrinolysis when cross-linked fibrin is cleaved by plasmin.
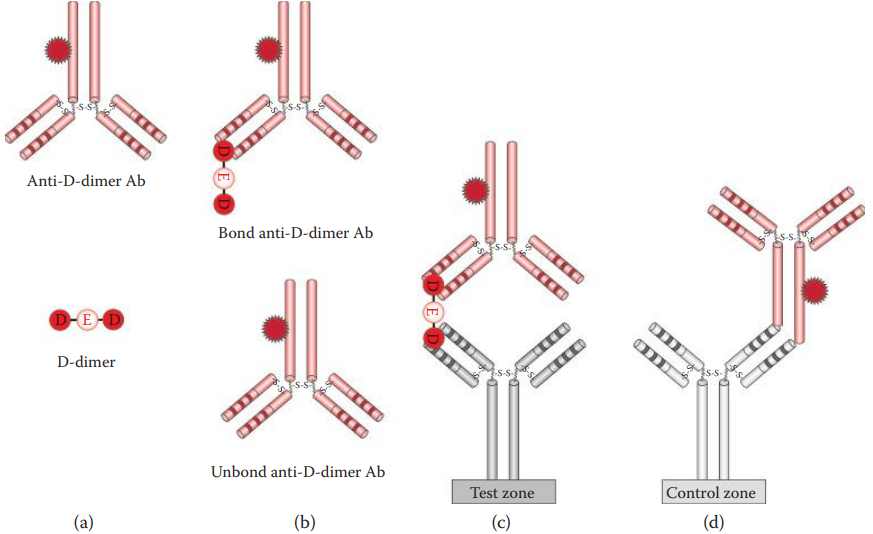
In ELISA, antibodies bind to the D-dimer antigens on the solid phase.
The D-dimer–antibody complex is subsequently analyzed using an antibody-based detection system. This method is highly sensitive, but is time-consuming.
Latex agglutination assays are based on the interaction of antibodies and D-dimers that are located on carriers to form aggregates during the agglutination process.
Immunochromatographic assays utilize monoclonal antibodies specific to D-dimers, which have been developed recently. It is very specific, sensitive, and rapid, and can be completed within minutes.
Although peripheral blood contains low levels of D-dimer, these assays do not show positive reactions with peripheral blood.
Menstrual blood can be distinguished from peripheral blood using D-dimer assays.
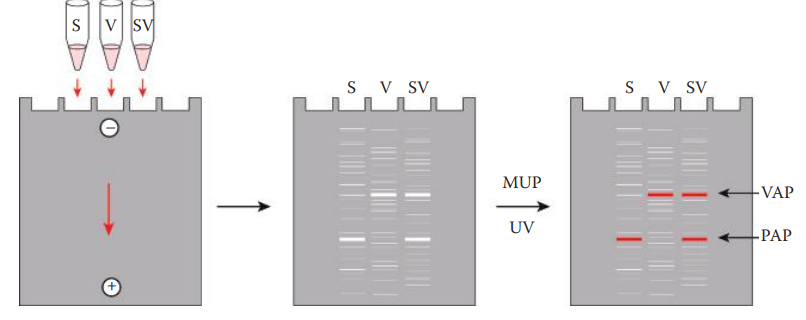
16.7: Lactate Dehydrogenase Assay
Lactate dehydrogenase (LDH): An enzyme that plays an important role in glycolysis. It catalyzes the reversible reduction of pyruvate into lactate when the amount of oxygen is limited.
It is tetrameric enzyme consisting of three different types of subunits.
A subunit: It is encoded by the LDHA gene and is primarily expressed in skeletal muscle.
B subunit: It is encoded by the LDHB gene and is primarily expressed in cardiac muscle.
C subunit: It is encoded by the LDHC gene, is expressed restrictively in the testes.
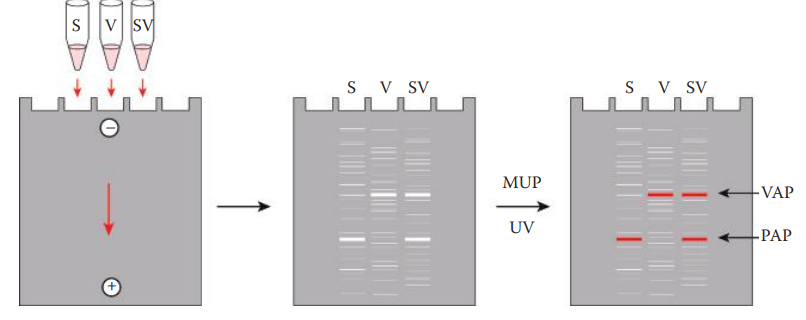
LDHs are found in various human tissues. Five isoenzymes can be found in blood:
LDH1 consists of four identical B subunits;
LDH2 consists of one A and three B subunits;
LDH3 consists of two A and two B subunits;
LDH4 consists of three A and one B subunits; and
LDH5 consists of four identical A subunits.
According to their electrophoretic mobility, five bands can be identified.
LDH1 has the highest electrophoretic mobility.
LDH5 has the lowest electrophoretic mobility.
LDH1, 2, and 3 are the predominant forms of the isoenzymes in peripheral blood.
LDH4 and 5 are consistently the predominant isoenzymes in menstrual blood.
16.8: RNA-Based Assays
Matrix metalloproteinase (MMP) genes are considered tissue-specific markers for human endometrium tissues.
These are zinc-dependent endopeptidases that degrade extracellular matrix components. They
Extracellular matrix (ECM): The extracellular space of tissue that is filled by macromolecules such as collagens, laminins, fibronectins, and proteoglycans.
Interstitial Matrix: These matrices are located in the intercellular spaces.
Basement membrane: These are thin layers of macromolecule fibers that usually lie under the epithelium and the endothelium.
The most commonly used markers for the forensic identification of menstrual blood are MMP7 and MMP11.
The patterns of the MMP gene expressions are correlated with their functions in endometrium tissue breakdown during menstruation.
MMP7 is predominantly expressed in epithelial cells, while MMP11 is expressed in the stromal cells of the endometrium.
is also known that MMPs’ mRNA may be elevated in postpartum, wound healing, and metastatic cancer conditions, which may potentially lead to a false-positive identification of menstrual blood.
In menstrual blood samples, MMP11 is the most sensitive and specific marker for distinguishing menstrual blood from peripheral blood.
MMP11 mRNA can be detected in menstrual blood from the first to the eighth day of menstruation but it is absent in peripheral blood and vaginal secretions.
Chapter 16: Identification of Vaginal Secretions and Menstrual Blood
16.1: Identification of Vaginal Stratified Squamous Epithelial Cells
A normal human vagina is covered by the squamous mucosa, which is composed of stratified squamous epithelial tissue.
Lying under the squamous mucosa is the submucosa, which contains an abundance of connective tissue and capillaries.
Below the submucosa is the muscularis, which is made up of smooth muscle.
The squamous mucosa consists of multiple layers of cells:
Basal Layer: In this layer, basal cells are anchored to the basement membrane that separates the squamous mucosa from the submucosa.
Basal Cells: Are small in size with relatively large nuclei and are highly proliferative.
Parabasal Layer: This is where cells undergo differentiation.
Intermediate Layer: The cells are flattened and their nuclei are compressed.
Superficial Layer: This is where the cells are fully differentiated with small and dense nuclei.
Lugol’s Iodine Staining and Periodic Acid–Schiff Method
Lugol’s iodine solution: Named after the French physician Jean Lugol, is originally used as an antiseptic that is applied to skin or tissue to prevent infection.
It is utilized for the identification of glycogenated vaginal epithelial cells.
The technique is based on the principle that iodine reacts with intracellular glycogen to exhibit a color.
Glycogen is the principal storage form of glucose in animal and human cells and is found in the granules in the cytoplasm of the cells of many tissues.
In addition to squamous epithelial cells, glycogen is also found in hepatocytes, which have the highest glycogen content, as well as muscle cells.
Lugol’s stock solution is an aqueous solution of 5% iodine (I2) and 10% potassium iodide (KI).
Potassium iodide allows the iodine to be soluble in water through the formation of the triiodide ion.
Dane’s Staining Method
Skin, buccal, and vaginal epithelial cells belong to stratified squamous epithelium.
Differentiated skin epithelial cells are keratinized and are classified as keratinizing squamous epithelial cells, while buccal and vaginal epithelial cells are nonkeratinizing squamous epithelial cells.
The skin epithelial cells lose nuclei and other cellular organelles during differentiation.
Dane’s staining method has been developed to distinguish all three types of cells.
Skin cells are stained red and orange;
Buccal cells are stained predominantly orange-pink with red nuclei; and
Vaginal cells are stained bright orange with orange nuclei.
16.2: Identification of Vaginal Acid Phosphatase
Acid phosphatases are a group of enzymes that are capable of hydrolyzing a variety of small organic phosphomonoesters under acidic conditions.
Five different acid phosphatase isoenzymes identified in human tissues:
erythroid acid phosphatase;
lysosomal acid phosphatase;
prostate acid phosphatase;
macrophage acid phosphatase;
testicular acid phosphatase.
Human prostatic acid phosphatase is found in large quantities in seminal fluid and is used as a biomarker for semen identification.
Prostatic acid phosphatase: A homodimer containing two identical subunits with a molecular weight of 50 kDa. Small amounts of acid phosphatase can be detected in vaginal fluid, which is produced in normal cervical epithelial cells.
16.3: Identification of Vaginal Bacteria
Lactobacillus: It can be found in the respiratory, the gastrointestinal, and the urogenital tract of healthy humans and animals.
Lactobacillus taxa: These are the predominant bacteria in the vagina of women of reproductive age, and they play an important role in protecting the host against invasive pathogenic organisms.
Lactobacillus consists of rod-shaped, nonmotile, and non-spore-forming gram-positive bacteria.
Lactobacillus bacteria produce lactic acid.
16.4: Outlook for Confirmatory Assays of Vaginal Secretions
Nondestructive confirmatory identification methods such as fluorescence spectroscopy and Raman spectroscopy can potentially be useful for the identification of vaginal secretions.
The analysis of tissue-specific gene expression has been utilized for the identification of vaginal secretions.
Using the reverse transcription polymerase chain reaction (RT-PCR) technique, the mRNAs of the tissue-specific genes of vaginal epithelial cells can be detected.
The commonly used markers for vaginal secretion identification are:
MUC4: Encodes a mucin protein that is a major component of vaginal mucus.
HBD1: Encodes a vaginal antimicrobial peptide.
16.5: Menstruation
Menstruation: The periodic discharge of blood and the elimination of the degenerated lining of the endometrium from the uterus of nonpregnant women.
From menarche to menopause, women may menstruate up to 400 times during their reproductive age.
The uterus plays an important role in preparing the uterine endometrium for the possible implantation of a developing embryo.
The linings of the uterus are composed of the myometrium and the endometrium.
Myometrium: Consists of the muscle fibers of the uterus.
Endometrium: Consists of the simple columnar epithelium and the stroma.
The endometrium consists of the simple columnar epithelium and the stroma.
Simple columnar epithelium: Formed by single-layered elongated cells located at the apical surface of the endometrium.
Stroma: It consists of connective tissues as well as spiral arteries.
Spiral arteries: These are small arteries that ascend through the endometrium and form a coil-like structure, which supplies blood to the endometrium.
Representative Markers of mRNA-Based Assays for Vaginal Secretions and Menstrual Blood Identification
Vaginal Secretions:
CYP2B7P1: Cytochrome P450, family 2, subfamily B, polypeptide 7, pseudogene 1.
DKK4: Dickkopf homolog 4
FUT6: Fucosyltransferase 6
HBD1: β Defensin 1
IL19: Interleukin 19
MUC4: Mucin 4
MYOZ1: Myozenin 1
SFTA2: Surfactant associated 2
Menstrual blood:
MMP7: Matrix metalloproteinase 7
MMP11: Matrix metalloproteinase 11
miRNA Markers for Vaginal Secretions and Menstrual Blood Identification
Vaginal secretions:
miR124a: UAAGGCACGCGGUGAAUGCC
miR372: AAAGUGCUGCGACAUUUGAGCGU
miR617: AGACUUCCCAUUUGAAGGUGGC
miR891a: UGCAACGAACCUGAGCCACUGA
Menstrual Blood:
miR214: UGCCUGUCUACACUUGCUGUGC
miR412: ACUUCACCUGGUCCACUAGCCGU
miR451: AAACCGUUACCAUUACUGAGUU
Uterine Cycle
The endometrium can be divided into two zones:
Functionalis: The luminal part of the endometrium. It is the zone of cyclic changes in the endometrium and is shed during menstruation.
Basalis: The basal part of the endometrium and is not shed during menstruation. This zone produces cells to regenerate the functionalis during the next cycle.
During the uterine cycle, repetitive physiological changes occur in the functionalis.
The cycle is divided into three phases:
During the menstrual phase, the functionalis degenerates and is sloughed off from the uterine wall and bleeding occurs, known as menses.
During the proliferative phase, the functionalis begins regeneration in which the spiral arteries are proliferated.
During the secretory phase, the spiral arteries are further developed and coiled.
In the absence of pregnancy, a decrease in the progesterone level leads to the constriction of the spiral arteries. As a result, the functionalis becomes ischemic, leading to hypoxia.
Uterine Endometrial Hemostasis
The cessation of menstrual bleeding is achieved by endometrial hemostasis that is initiated when injury occurs due to the shedding of the endometrium.
Hemostasis begins with platelet activation and aggregation to form platelet plugs at the site of injury.
The blood coagulation cascade is activated to produce thrombin.
Thrombin: A serine protease, converts soluble fibrinogen into fibrin.
Fibrin: A protein involved in blood clotting, aggregates with the platelet plugs and leads to the cessation of bleeding by forming blood clots, known as thrombi.
Under normal physiological conditions, uterine endometrial hemostasis is a balanced process between blood coagulation and clot dissolution to control blood loss and to prevent clot accumulation within the uterus.
Blood clots are prevented from accumulating during menstruation by forming low amounts of platelet plugs and synthesizing coagulation factor inhibitors that inhibit blood coagulation.
Fibrinolysis is activated, during which the thrombus is broken down by a protease known as plasmin. Plasmin cleaves fibrin, generating soluble degradation products.
16.6: D-dimer Assay
D-dimer: A degradation product produced during fibrinolysis when cross-linked fibrin is cleaved by plasmin.
In ELISA, antibodies bind to the D-dimer antigens on the solid phase.
The D-dimer–antibody complex is subsequently analyzed using an antibody-based detection system. This method is highly sensitive, but is time-consuming.
Latex agglutination assays are based on the interaction of antibodies and D-dimers that are located on carriers to form aggregates during the agglutination process.
Immunochromatographic assays utilize monoclonal antibodies specific to D-dimers, which have been developed recently. It is very specific, sensitive, and rapid, and can be completed within minutes.
Although peripheral blood contains low levels of D-dimer, these assays do not show positive reactions with peripheral blood.
Menstrual blood can be distinguished from peripheral blood using D-dimer assays.
16.7: Lactate Dehydrogenase Assay
Lactate dehydrogenase (LDH): An enzyme that plays an important role in glycolysis. It catalyzes the reversible reduction of pyruvate into lactate when the amount of oxygen is limited.
It is tetrameric enzyme consisting of three different types of subunits.
A subunit: It is encoded by the LDHA gene and is primarily expressed in skeletal muscle.
B subunit: It is encoded by the LDHB gene and is primarily expressed in cardiac muscle.
C subunit: It is encoded by the LDHC gene, is expressed restrictively in the testes.
LDHs are found in various human tissues. Five isoenzymes can be found in blood:
LDH1 consists of four identical B subunits;
LDH2 consists of one A and three B subunits;
LDH3 consists of two A and two B subunits;
LDH4 consists of three A and one B subunits; and
LDH5 consists of four identical A subunits.
According to their electrophoretic mobility, five bands can be identified.
LDH1 has the highest electrophoretic mobility.
LDH5 has the lowest electrophoretic mobility.
LDH1, 2, and 3 are the predominant forms of the isoenzymes in peripheral blood.
LDH4 and 5 are consistently the predominant isoenzymes in menstrual blood.
16.8: RNA-Based Assays
Matrix metalloproteinase (MMP) genes are considered tissue-specific markers for human endometrium tissues.
These are zinc-dependent endopeptidases that degrade extracellular matrix components. They
Extracellular matrix (ECM): The extracellular space of tissue that is filled by macromolecules such as collagens, laminins, fibronectins, and proteoglycans.
Interstitial Matrix: These matrices are located in the intercellular spaces.
Basement membrane: These are thin layers of macromolecule fibers that usually lie under the epithelium and the endothelium.
The most commonly used markers for the forensic identification of menstrual blood are MMP7 and MMP11.
The patterns of the MMP gene expressions are correlated with their functions in endometrium tissue breakdown during menstruation.
MMP7 is predominantly expressed in epithelial cells, while MMP11 is expressed in the stromal cells of the endometrium.
is also known that MMPs’ mRNA may be elevated in postpartum, wound healing, and metastatic cancer conditions, which may potentially lead to a false-positive identification of menstrual blood.
In menstrual blood samples, MMP11 is the most sensitive and specific marker for distinguishing menstrual blood from peripheral blood.
MMP11 mRNA can be detected in menstrual blood from the first to the eighth day of menstruation but it is absent in peripheral blood and vaginal secretions.
 Knowt
Knowt
