Robbins: Chapter 3 Inflammation and Repair
What is Inflammation?
inflammation is a protective response to damage or infection of vascularized tissue
it triggers immune cells from the circulatory system to eliminate offending agents
phagocytic leukocytes, antibodies, complement proteins
What are the four cardinal signs of inflammation?
redness
swelling
heat
pain
function ( later added)
What are some causes for inflammation?
infections
tissue necrosis
foreign bodies
immune reaction (hypersensitivity)
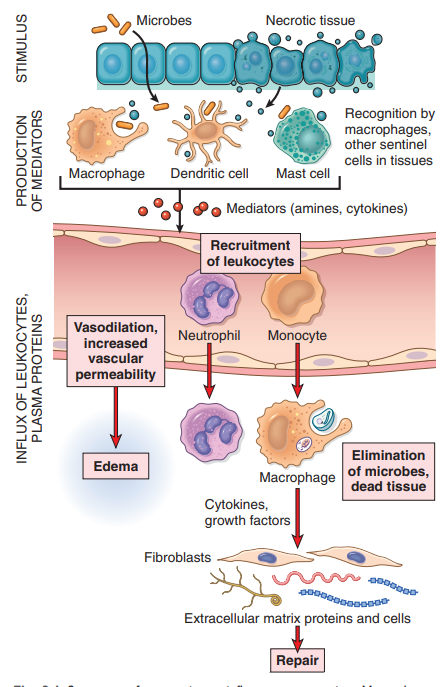
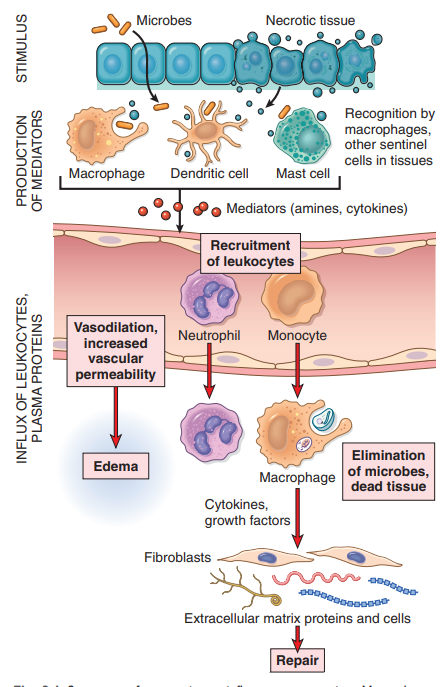
Steps in inflammation?
microbe enters body/ trauma
Recognition the skin barrier is broken and macrophage, dendritic cells, and Mast cells
cellular receptors for microbes → PAMPs(pathogen-associated molecular patterns)
senores of cell damage → DAMPs( damage-associated molecular patterns)
They recognize the microbe and trigger mediates amiens and cytokines) to recruit leukocytes
cytokines → what to do!
chemokines → where to go!
Removal of stimulus Monocytes → macrophages and Granulocytes eliminate microbes.
Repair of possible damaged tissue
3 major components of acute inflammation?
dilation of small vessels leading to an increase in blood flow
increased permeability of the microvasculature, enabling plasma proteins and leukocytes from the circulation
emigration of leukocytes from the microcirculation, their accumulation in the focus of injury, and their activation to eliminate the offending agent
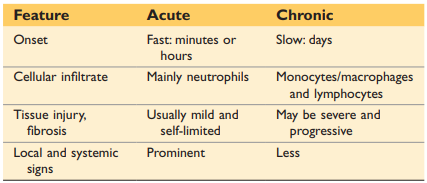
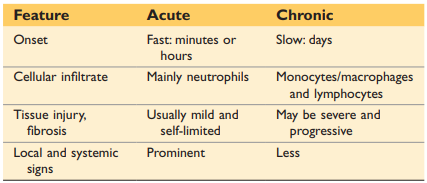
Difference between acute and chronic inflammation?
acute inflammation: is the initial rapid response (within minutes or hours) to eliminate offenders
characteristic:
vasodilation
edema (increased vascular permeability)
emigration of leucocytes( predominantly neutrophils)
Chronic inflammation: is triggered when the initial response fails to clear the stimulus
characteristics:
longer duration
more tissue destruction
dominated by lymphocytes and macrophages
more proliferation of blood vessels and fibrosis
What is exudate and transudate? how is it related to acute inflammation?
exudate: extravascular fluid that has high protein concentration and contains cellular debris → implies existence of inflammatory process
in big amounts it is called pus
transudate: fluid with low protein content with little to no cellular material → produced due to hydrostatic imbalance but not due to inflammation
in big amounts called edema
what are changes in vascular flow in response to inflammation?
increased blood flow → vasodilation → cause of heat and redness
increased permeability: exudate of fluid into extravascular tissue
loss of fluid → slower blood flow(stasis) + increased viscosity
as stasis develops neutrophils accumulate along the vascular endothelium( more this in a later question)
What is the multistep journey of leukocytes?
(1) rolling → from center to endothelium walls with the help of selectins, which are the ligands found on leucocyte
(2) integrin activation by chemokines
(3) stable adhesion → integrins are the ligands found on leukocyte membrane that attach to the receptors on endothelial cells
(4) migration through endothelium (diaphyses/transmigration)
What are chemoattractants? And give some examples.
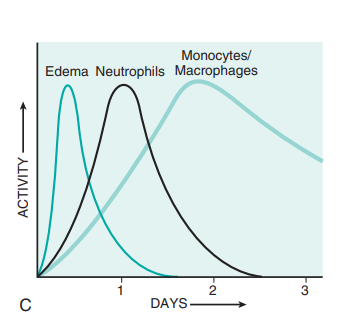
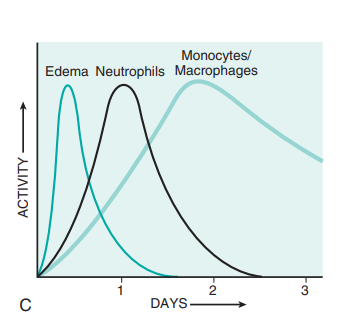
Chemoatractes are produced by microbes and by host cells in response to n infections r tissue damage. They signal neutrophils and leukocytes towards which direction the inflammatory site is. First, neutrophils arrive to the site, but due to their short half-life, they are then replaced by Monocytes/Macrophages.
examples:
LTB4
C5a
IL-8
What is key when terminating the inflammation and what are the associated steps?
Phagocytosis and clearance of the offending agent
(1) recognitions and attachment of the particle to be ingested by the leukocyte
(2) engulfment, with subsequent formation of a phagocytic vacuole
(3) killing or degradation of the ingested material with lysomome
What is the function compliant system?
it only destroys bacteria by drilling holes into the cell walls of the bacteria
if this happens in normal healthy cell this causes major tissue damage
What are the possible outcomes of acute inflammation ?
complete resolution
restoration of the site to normal tissue
removal of cellular debris
no edema
healing by connective tissue replacement
scarring or fibrosis
Progression of the response to chronic inflammation
How can you recognize inflamed tissue under a microscope?
fluid-filled space → edema
fibrinous exudate
accumulation of granulocytes
purulent inflammation → pus( dead granulocytes)
ulcer → local tissue destruction
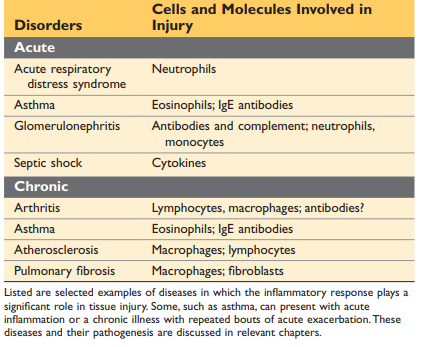
Name different acute and chronic inflammatory diseases:
What causes chronic inflammation?
Immune-mediated inflammatory( hypersensitivity)
autoimmune disease
allergies
Persistent or prolonged exposure to microbial infections by microorganisms that are difficult to eradicate
Due to a delayed response immune reaction
development if granulomatous inflammation
walling of epithelial cells due to dead granulocytes
What are two types of macrophage activation?
what are systemic effects of inflation
production of proteins: acute-pashe protein
C-reactive protein (CRP) and serum amyloid A protein( SAA)
Fever
when does the repair of damage start?
the work simoultainsly and can´t be seen as separate processes
inflammatory vs anti
autoimmune lymphocytes that recognize cells falsely
autoinflammatory aggressive cells that just fire but it is not targeted
each phase of the inflammatory response are associated with disease with the off switch of proteins is faulty
What happens when microbo flora crosses the one cell layer that protects
the first line of defense: innate immune → 99% of invasive microbes are depleted
epithelium
macrophages
neutrophils
adapt system is triggered by an innate system via chemokines( signaling molecules)
b and t cells
Tuberculosis is a bacterium that causes a chronic inflammatory response
in crohns the histology looks similar because the body falsely reacts to microbes because the body confuses the two → genetic defects
If you have impairment in innate response than their is a bigger/faster response of the auqired immune system to make up for the work
lazy leukocyte syndrome
leuity work slower ad, therefore, cause chronic inflammation because they fulfill they job to slow
post-infectious autoimmune disease!!
a microbe is recognized by t cell; however, after that the body confuses its own body causing chronic inflammation
granuloma
to prevent spreading through the body
chronic granular disease
Hermans putlock disease
neutrophils love shortly
regulatory t cell -→ controls immune response (dampens it)
T-cell diseases → organ specific
too many t cells or too little regulatory t cells
repair and regeneration
repair → with scaring
regeneration → exact copy of what was damaged
cholangiocytes: scar cells
remodeling: differences in tissue in organs
why repair and not regeneration
repair is faster
Kupfer cells are macrophages in liver
what happens after liver failure?
edema
turn yellow
very sensitive to toxins
steps after cutting skin
clotting
epithelial cells
granulation tissue
Robbins: Chapter 3 Inflammation and Repair
What is Inflammation?
inflammation is a protective response to damage or infection of vascularized tissue
it triggers immune cells from the circulatory system to eliminate offending agents
phagocytic leukocytes, antibodies, complement proteins
What are the four cardinal signs of inflammation?
redness
swelling
heat
pain
function ( later added)
What are some causes for inflammation?
infections
tissue necrosis
foreign bodies
immune reaction (hypersensitivity)
Steps in inflammation?
microbe enters body/ trauma
Recognition the skin barrier is broken and macrophage, dendritic cells, and Mast cells
cellular receptors for microbes → PAMPs(pathogen-associated molecular patterns)
senores of cell damage → DAMPs( damage-associated molecular patterns)
They recognize the microbe and trigger mediates amiens and cytokines) to recruit leukocytes
cytokines → what to do!
chemokines → where to go!
Removal of stimulus Monocytes → macrophages and Granulocytes eliminate microbes.
Repair of possible damaged tissue
3 major components of acute inflammation?
dilation of small vessels leading to an increase in blood flow
increased permeability of the microvasculature, enabling plasma proteins and leukocytes from the circulation
emigration of leukocytes from the microcirculation, their accumulation in the focus of injury, and their activation to eliminate the offending agent
Difference between acute and chronic inflammation?
acute inflammation: is the initial rapid response (within minutes or hours) to eliminate offenders
characteristic:
vasodilation
edema (increased vascular permeability)
emigration of leucocytes( predominantly neutrophils)
Chronic inflammation: is triggered when the initial response fails to clear the stimulus
characteristics:
longer duration
more tissue destruction
dominated by lymphocytes and macrophages
more proliferation of blood vessels and fibrosis
What is exudate and transudate? how is it related to acute inflammation?
exudate: extravascular fluid that has high protein concentration and contains cellular debris → implies existence of inflammatory process
in big amounts it is called pus
transudate: fluid with low protein content with little to no cellular material → produced due to hydrostatic imbalance but not due to inflammation
in big amounts called edema
what are changes in vascular flow in response to inflammation?
increased blood flow → vasodilation → cause of heat and redness
increased permeability: exudate of fluid into extravascular tissue
loss of fluid → slower blood flow(stasis) + increased viscosity
as stasis develops neutrophils accumulate along the vascular endothelium( more this in a later question)
What is the multistep journey of leukocytes?
(1) rolling → from center to endothelium walls with the help of selectins, which are the ligands found on leucocyte
(2) integrin activation by chemokines
(3) stable adhesion → integrins are the ligands found on leukocyte membrane that attach to the receptors on endothelial cells
(4) migration through endothelium (diaphyses/transmigration)
What are chemoattractants? And give some examples.
Chemoatractes are produced by microbes and by host cells in response to n infections r tissue damage. They signal neutrophils and leukocytes towards which direction the inflammatory site is. First, neutrophils arrive to the site, but due to their short half-life, they are then replaced by Monocytes/Macrophages.
examples:
LTB4
C5a
IL-8
What is key when terminating the inflammation and what are the associated steps?
Phagocytosis and clearance of the offending agent
(1) recognitions and attachment of the particle to be ingested by the leukocyte
(2) engulfment, with subsequent formation of a phagocytic vacuole
(3) killing or degradation of the ingested material with lysomome
What is the function compliant system?
it only destroys bacteria by drilling holes into the cell walls of the bacteria
if this happens in normal healthy cell this causes major tissue damage
What are the possible outcomes of acute inflammation ?
complete resolution
restoration of the site to normal tissue
removal of cellular debris
no edema
healing by connective tissue replacement
scarring or fibrosis
Progression of the response to chronic inflammation
How can you recognize inflamed tissue under a microscope?
fluid-filled space → edema
fibrinous exudate
accumulation of granulocytes
purulent inflammation → pus( dead granulocytes)
ulcer → local tissue destruction
Name different acute and chronic inflammatory diseases:
What causes chronic inflammation?
Immune-mediated inflammatory( hypersensitivity)
autoimmune disease
allergies
Persistent or prolonged exposure to microbial infections by microorganisms that are difficult to eradicate
Due to a delayed response immune reaction
development if granulomatous inflammation
walling of epithelial cells due to dead granulocytes
What are two types of macrophage activation?
what are systemic effects of inflation
production of proteins: acute-pashe protein
C-reactive protein (CRP) and serum amyloid A protein( SAA)
Fever
when does the repair of damage start?
the work simoultainsly and can´t be seen as separate processes
inflammatory vs anti
autoimmune lymphocytes that recognize cells falsely
autoinflammatory aggressive cells that just fire but it is not targeted
each phase of the inflammatory response are associated with disease with the off switch of proteins is faulty
What happens when microbo flora crosses the one cell layer that protects
the first line of defense: innate immune → 99% of invasive microbes are depleted
epithelium
macrophages
neutrophils
adapt system is triggered by an innate system via chemokines( signaling molecules)
b and t cells
Tuberculosis is a bacterium that causes a chronic inflammatory response
in crohns the histology looks similar because the body falsely reacts to microbes because the body confuses the two → genetic defects
If you have impairment in innate response than their is a bigger/faster response of the auqired immune system to make up for the work
lazy leukocyte syndrome
leuity work slower ad, therefore, cause chronic inflammation because they fulfill they job to slow
post-infectious autoimmune disease!!
a microbe is recognized by t cell; however, after that the body confuses its own body causing chronic inflammation
granuloma
to prevent spreading through the body
chronic granular disease
Hermans putlock disease
neutrophils love shortly
regulatory t cell -→ controls immune response (dampens it)
T-cell diseases → organ specific
too many t cells or too little regulatory t cells
repair and regeneration
repair → with scaring
regeneration → exact copy of what was damaged
cholangiocytes: scar cells
remodeling: differences in tissue in organs
why repair and not regeneration
repair is faster
Kupfer cells are macrophages in liver
what happens after liver failure?
edema
turn yellow
very sensitive to toxins
steps after cutting skin
clotting
epithelial cells
granulation tissue
 Knowt
Knowt