
Excretion in Humans (2.43-2.44)
Excretion: removal of the waste substances of metabolic reactions, toxic materials and substances in excess of requirements
Lungs excrete carbon dioxide
Carbon dioxide dissolves in water and forms an acidic solution which can lower the pH of the cells
Kidneys excrete urea and excess water and salts to form urine
Urea is the waste product formed in the liver, urine is made in the kidneys and is the combination of urea with water and other salts
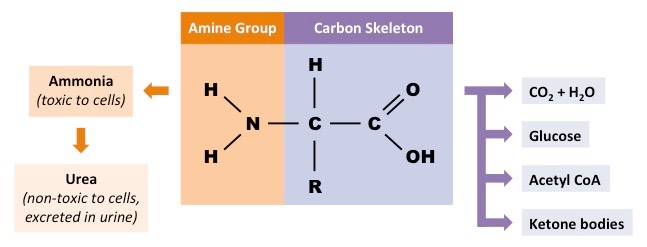
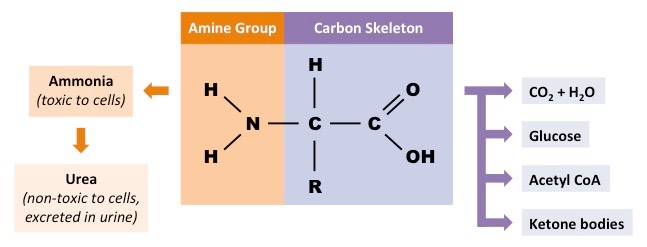
Urea is formed by deamination
Digested food molecules absorbed in the blood are carried to the liver for assimilation
Amino acids are converted into proteins eg. fibrinogen
Excess amino acids cannot be stored so are they are broken down by DEAMINATION OF AMINO ACIDS
Deamination: the removal of the nitrogen containing part of excess amino acids to form urea
Enzymes in the liver split up the amino acid molecules and remove the nitrogen containing part and convert it into ammonia (which is highly toxic) and then urea (less toxic)
Urea dissolves in the blood and is sent to the kidney to be excreted
The nitrogen-containing amino group is removed and converted into ammonia and then urea to be excreted
Urinary System
Kidney: Two bean shaped organs that filter the blood
Ureter: Carries urine from kidneys to bladder
Bladder: Stores urine as it is produced by kidneys
Urethra: Connects bladder to exterior
Renal artery: Carries unfiltered oxygenated blood to the kidneys
Renal vein: Carries filtered deoxygenated blood away from the kidneys

Blood is brought to the kidney in the renal artery
The kidneys filter the blood and then reabsorb useful materials such as glucose.
After it has been purified, the blood returns to the circulation through the renal vein.
Urine is taken from the kidneys to the bladder by the ureters.
The bladder stores the urine until it is convenient to expel it from the body
The volume and concentration of urine may depend on certain factors:
Hydration
More water intake leads to more excess water. This means the volume of urine will increase and the concentration will decrease
large quantity of pale yellow dilute urine
Warm temperature or Excercise (dehydration)
Dehydration results in less excess water. This means the volume of urine will decrease and the concentration will increase
smaller quantity of dark yellow, concentrated urine
Kidney
Role of Kidney:
Regulate the water content of the blood (vital for maintaining blood pressure)
Excrete the toxic waste products of metabolism (urea) and substances in excess of requirements (salts)


The medulla of the kidneys are made of kidney tubules called nephrons
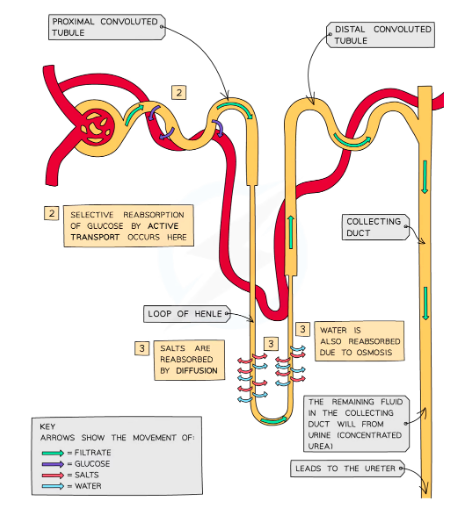
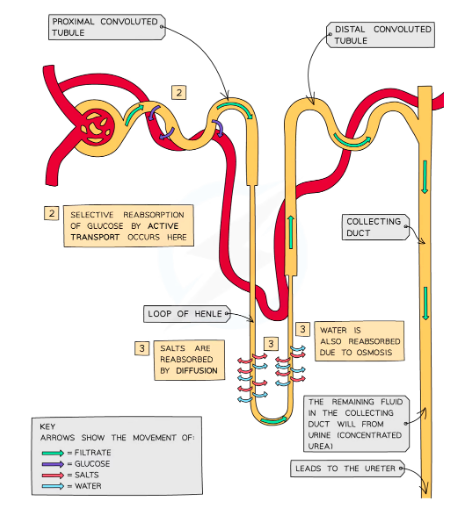
Ultrafiltration
The renal artery branches off to form a knot of capillaries in each nephron (the glomerulus) that sits inside Bowman's capsule.
Because of the high blood pressure in the capillaries, smaller molecules are forced into the Bowman's capsule, where they form the filtrate.
Glucose, water, urea and salts are forced out of the capillaries
Selective reabsorbtion
Glucose reabsorbed at the proximal (first) convoluted tubule (PCT) by active transport
Nephrons have many mitochondria to provide energy for active transport
Reabsorption of Water & Salts
Filtrate goes through Loop of Henle where some salts are reabsorbed back into the blood by diffusion and water by osmosis
Water is also reabsorbed from the collecting duct in different amounts depending on how much water the body needs at that time (controlled by ADH)

ADH: Antidiuretic hormone controlls the water content of the blood
Hypothalamus detects water level
Pituitary gland releases ADH
More water reabsorbed by kidneys
Less water lost in urine
OR
Hypothalamus detects water level
Pituitary gland releases less ADH
Less water reabsorbed by kidneys
More water lost in urine
(Negative feedback)
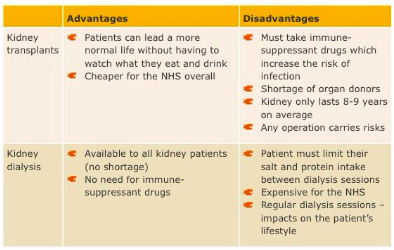
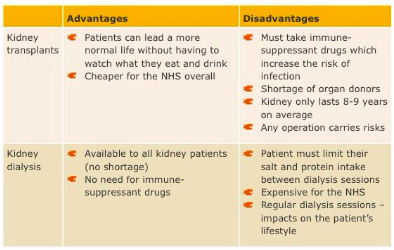
Kidney Failure and Treatment
Kidney Failure
If both kidneys are damaged toxic wastes will build up in the body and lead to death if not removed
Kidney Dialysis:
Unfiltered blood is taken from the human
→ taking unfiltered blood from the arm
The blood is filtered in a dialysis machine
The blood then enters the dialysis machine. The machine contains a circuit for the blood, and a surrounding dialysis fluid
A semi-permeable membrane seperates the blood from the dialysis fluid
Dialysis fluid contains: a glucose concentration similar to a normal level in blood, a concentration of salts similar to a normal level in blood and no urea
To maintain concentration gradients and ensure only urea diffuses across the membrane
Waste products pass from blood to dialysis fluid
Fluids flow in opposite directions; aids diffusion as it keeps the concentration gradient going.
Maintains a high concentration of urea in the blood, and a low concentration of urea in the dialysis fluid, so that urea is always moving out of the blood

Excretion in Humans (2.43-2.44)
Excretion: removal of the waste substances of metabolic reactions, toxic materials and substances in excess of requirements
Lungs excrete carbon dioxide
Carbon dioxide dissolves in water and forms an acidic solution which can lower the pH of the cells
Kidneys excrete urea and excess water and salts to form urine
Urea is the waste product formed in the liver, urine is made in the kidneys and is the combination of urea with water and other salts
Urea is formed by deamination
Digested food molecules absorbed in the blood are carried to the liver for assimilation
Amino acids are converted into proteins eg. fibrinogen
Excess amino acids cannot be stored so are they are broken down by DEAMINATION OF AMINO ACIDS
Deamination: the removal of the nitrogen containing part of excess amino acids to form urea
Enzymes in the liver split up the amino acid molecules and remove the nitrogen containing part and convert it into ammonia (which is highly toxic) and then urea (less toxic)
Urea dissolves in the blood and is sent to the kidney to be excreted
The nitrogen-containing amino group is removed and converted into ammonia and then urea to be excreted
Urinary System
Kidney: Two bean shaped organs that filter the blood
Ureter: Carries urine from kidneys to bladder
Bladder: Stores urine as it is produced by kidneys
Urethra: Connects bladder to exterior
Renal artery: Carries unfiltered oxygenated blood to the kidneys
Renal vein: Carries filtered deoxygenated blood away from the kidneys

Blood is brought to the kidney in the renal artery
The kidneys filter the blood and then reabsorb useful materials such as glucose.
After it has been purified, the blood returns to the circulation through the renal vein.
Urine is taken from the kidneys to the bladder by the ureters.
The bladder stores the urine until it is convenient to expel it from the body
The volume and concentration of urine may depend on certain factors:
Hydration
More water intake leads to more excess water. This means the volume of urine will increase and the concentration will decrease
large quantity of pale yellow dilute urine
Warm temperature or Excercise (dehydration)
Dehydration results in less excess water. This means the volume of urine will decrease and the concentration will increase
smaller quantity of dark yellow, concentrated urine
Kidney
Role of Kidney:
Regulate the water content of the blood (vital for maintaining blood pressure)
Excrete the toxic waste products of metabolism (urea) and substances in excess of requirements (salts)


The medulla of the kidneys are made of kidney tubules called nephrons
Ultrafiltration
The renal artery branches off to form a knot of capillaries in each nephron (the glomerulus) that sits inside Bowman's capsule.
Because of the high blood pressure in the capillaries, smaller molecules are forced into the Bowman's capsule, where they form the filtrate.
Glucose, water, urea and salts are forced out of the capillaries
Selective reabsorbtion
Glucose reabsorbed at the proximal (first) convoluted tubule (PCT) by active transport
Nephrons have many mitochondria to provide energy for active transport
Reabsorption of Water & Salts
Filtrate goes through Loop of Henle where some salts are reabsorbed back into the blood by diffusion and water by osmosis
Water is also reabsorbed from the collecting duct in different amounts depending on how much water the body needs at that time (controlled by ADH)

ADH: Antidiuretic hormone controlls the water content of the blood
Hypothalamus detects water level
Pituitary gland releases ADH
More water reabsorbed by kidneys
Less water lost in urine
OR
Hypothalamus detects water level
Pituitary gland releases less ADH
Less water reabsorbed by kidneys
More water lost in urine
(Negative feedback)
Kidney Failure and Treatment
Kidney Failure
If both kidneys are damaged toxic wastes will build up in the body and lead to death if not removed
Kidney Dialysis:
Unfiltered blood is taken from the human
→ taking unfiltered blood from the arm
The blood is filtered in a dialysis machine
The blood then enters the dialysis machine. The machine contains a circuit for the blood, and a surrounding dialysis fluid
A semi-permeable membrane seperates the blood from the dialysis fluid
Dialysis fluid contains: a glucose concentration similar to a normal level in blood, a concentration of salts similar to a normal level in blood and no urea
To maintain concentration gradients and ensure only urea diffuses across the membrane
Waste products pass from blood to dialysis fluid
Fluids flow in opposite directions; aids diffusion as it keeps the concentration gradient going.
Maintains a high concentration of urea in the blood, and a low concentration of urea in the dialysis fluid, so that urea is always moving out of the blood

 Knowt
Knowt
