Other Subject
anatomy
physiology
science
nervous system
autonomic
Divisions of the Autonomic Nervous System
Sympathetic Division of the Autonomic Nervous System
Parasympathetic Division of the Autonomic Nervous System
Chemical Signaling in the Autonomic Nervous System
reflexes
structure of reflexes
Drugs that Affect the Autonomic System
sympathetic division
parasympathetic division
fight-or-flight response
thoracolumbar system
central neuron
target effector
ganglionic neuron
paravertebral ganglia
Collateral ganglia
University/Undergrad

Chapter 15: The Autonomic Nervous System
Divisions of the Autonomic Nervous System
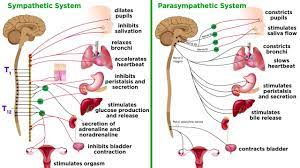
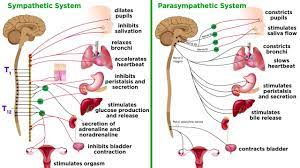
The autonomic nervous system regulates many of the internal organs through a balance of two aspects, or divisions.
The two divisions of the autonomic nervous system are the sympathetic division and the parasympathetic division.
The sympathetic system is associated with the fight-or-flight response, and parasympathetic activity is referred to by the epithet of rest and digest.
Homeostasis is the balance between the two systems.
Sympathetic Division of the Autonomic Nervous System
The sympathetic division of the autonomic nervous system influences the various organ systems of the body through connections emerging from the thoracic and upper lumbar spinal cord.
It is referred to as the thoracolumbar system to reflect this anatomical basis.
A central neuron in the lateral horn of any of these spinal regions projects to ganglia adjacent to the vertebral column through the ventral spinal roots.
The majority of ganglia of the sympathetic system belong to a network of sympathetic chain ganglia that runs alongside the vertebral column.
The first type is most direct: the sympathetic nerve projects to the chain ganglion at the same level as the target effector (the organ, tissue, or gland to be innervated).
The fibers of this branch are called white rami communicantes (singular = ramus communicans); they are myelinated and therefore referred to as white.
The axon from the central neuron (the preganglionic fiber shown as a solid line) synapses with the ganglionic neuron (with the postganglionic fiber shown as a dashed line).
This neuron then projects to a target effector—in this case, the trachea—via gray rami communicantes, which are unmyelinated axons.
The spinal nerve tracks up through the chain until it reaches the superior cervical ganglion, where it synapses with the postganglionic neuron
The cervical ganglia are referred to as paravertebral ganglia, given their location adjacent to prevertebral ganglia in the sympathetic chain.
Additional branches from the ventral nerve root continue through the chain and on to one of the collateral ganglia as the greater splanchnic nerve or lesser splanchnic nerve.
Collateral ganglia, also called prevertebral ganglia, are situated anterior to the vertebral column and receive inputs from splanchnic nerves as well as central sympathetic neurons.
The three collateral ganglia are the celiac ganglion, the superior mesenteric ganglion, and the inferior mesenteric ganglion.
An axon from the central neuron that projects to a sympathetic ganglion is referred to as a preganglionic fiber or neuron, and represents the output from the CNS to the ganglion.
A postganglionic fiber—the axon from a ganglionic neuron that projects to the target effector—represents the output of a ganglion that directly influences the organ.
The cells in the adrenal medulla that are contacted by the preganglionic fibers are called chromaffin cells.
Parasympathetic Division of the Autonomic Nervous System
The parasympathetic system can also be referred to as the craniosacral system (or outflow) because the preganglionic neurons are located in nuclei of the brain stem and the lateral horn of the sacral spinal cord.
The preganglionic fibers from the cranial region travel in cranial nerves, whereas preganglionic fibers from the sacral region travel in spinal nerves.
The targets of these fibers are terminal ganglia, which are located near—or even within—the target effector.
These ganglia are often referred to as intramural ganglia when they are found within the walls of the target organ.
In the midbrain, the Edinger–Westphal nucleus is part of the oculomotor complex, and axons from those neurons travel with the fibers in the oculomotor nerve (cranial nerve III) that innervate the extraocular muscles.
The preganglionic parasympathetic fibers within cranial nerve III terminate in the ciliary ganglion, which is located in the posterior orbit.
Neurons in the dorsal nucleus of the vagus nerve and the nucleus ambiguus project through the vagus nerve (cranial nerve X) to the terminal ganglia of the thoracic and abdominal cavities.
The postganglionic fibers from the ganglia activated by the vagus nerve are often incorporated into the structure of the organ, such as the mesenteric plexus of the digestive tract organs and the intramural ganglia.
Chemical Signaling in the Autonomic Nervous System
Synapses of the autonomic system are classified as either cholinergic, meaning that acetylcholine (ACh) is released, or adrenergic, meaning that norepinephrine is released.
The cholinergic system includes two classes of receptor: the nicotinic receptor and the muscarinic receptor.
The nicotinic receptor is a ligand-gated cation channel and the muscarinic receptor is a G protein–coupled receptor.
The adrenergic system also has two types of receptors, named the alpha (α)-adrenergic receptor and beta (β)-adrenergic receptor.
An additional aspect of the adrenergic system is that there is a second signaling molecule called epinephrine.
The Structure of Reflexes
One difference between a somatic reflex, such as the withdrawal reflex, and a visceral reflex, which is an autonomic reflex, is in the efferent branch.
The other part of a reflex, the afferent branch, is often the same between the two systems.
Afferent Branch: The afferent branch of a reflex arc does differ between somatic and visceral reflexes in some instances.
Efferent Branch
The efferent branch of the visceral reflex arc begins with the projection from the central neuron along the preganglionic fiber.
This fiber then makes a synapse on the ganglionic neuron that projects to the target effector.
Short and Long Reflexes
A long reflex has afferent branches that enter the spinal cord or brain and involve the efferent branches, as previously explained.
A short reflex is completely peripheral and only involves the local integration of sensory input with motor output.
Central Control
Central control of autonomic reflexes is different than for somatic reflexes. The hypothalamus, along with other CNS locations, controls the autonomic system.
The Hypothalamus
The hypothalamus is the control center for many homeostatic mechanisms. It regulates both autonomic function and endocrine function.
Output from the hypothalamus follows two main tracts, the dorsal longitudinal fasciculus and the medial forebrain bundle
The Amygdala: The amygdala is a group of nuclei in the medial region of the temporal lobe that is part of the limbic lobe.
The Medulla
The medulla contains nuclei referred to as the cardiovascular center, which controls the smooth and cardiac muscle of the cardiovascular system through autonomic connections.
The preganglionic sympathetic fibers that are responsible for increasing heart rate are referred to as the cardiac accelerator nerves, whereas the preganglionic sympathetic fibers responsible for constricting blood vessels compose the vasomotor nerves.
Drugs that Affect the Autonomic System
An important way to understand the effects of native neurochemicals in the autonomic system is in considering the effects of pharmaceutical drugs.
A chemical that the body produces to interact with those receptors is called an endogenous chemical, whereas a chemical introduced to the system from outside is an exogenous chemical.
Sympathetic Effect
A drug that enhances adrenergic function is known as a sympathomimetic drug, whereas a drug that interrupts adrenergic function is a sympatholytic drug.
Phenylephrine is known as an α1-adrenergic agonist, meaning that it binds to a specific adrenergic receptor, stimulating a response.
Drugs that interfere with sympathetic function are referred to as sympatholytic, or sympathoplegic, drugs. They primarily work as an antagonist to the adrenergic receptors.
Parasympathetic Effects
Drugs that enhance cholinergic effects are called parasympathomimetic drugs, whereas those that inhibit cholinergic effects are referred to as anticholinergic drugs.
Atropine and scopolamine are part of a class of muscarinic antagonists that come from the Atropa genus of plants that include belladonna or deadly nightshade.
Chapter 15: The Autonomic Nervous System
Divisions of the Autonomic Nervous System
The autonomic nervous system regulates many of the internal organs through a balance of two aspects, or divisions.
The two divisions of the autonomic nervous system are the sympathetic division and the parasympathetic division.
The sympathetic system is associated with the fight-or-flight response, and parasympathetic activity is referred to by the epithet of rest and digest.
Homeostasis is the balance between the two systems.
Sympathetic Division of the Autonomic Nervous System
The sympathetic division of the autonomic nervous system influences the various organ systems of the body through connections emerging from the thoracic and upper lumbar spinal cord.
It is referred to as the thoracolumbar system to reflect this anatomical basis.
A central neuron in the lateral horn of any of these spinal regions projects to ganglia adjacent to the vertebral column through the ventral spinal roots.
The majority of ganglia of the sympathetic system belong to a network of sympathetic chain ganglia that runs alongside the vertebral column.
The first type is most direct: the sympathetic nerve projects to the chain ganglion at the same level as the target effector (the organ, tissue, or gland to be innervated).
The fibers of this branch are called white rami communicantes (singular = ramus communicans); they are myelinated and therefore referred to as white.
The axon from the central neuron (the preganglionic fiber shown as a solid line) synapses with the ganglionic neuron (with the postganglionic fiber shown as a dashed line).
This neuron then projects to a target effector—in this case, the trachea—via gray rami communicantes, which are unmyelinated axons.
The spinal nerve tracks up through the chain until it reaches the superior cervical ganglion, where it synapses with the postganglionic neuron
The cervical ganglia are referred to as paravertebral ganglia, given their location adjacent to prevertebral ganglia in the sympathetic chain.
Additional branches from the ventral nerve root continue through the chain and on to one of the collateral ganglia as the greater splanchnic nerve or lesser splanchnic nerve.
Collateral ganglia, also called prevertebral ganglia, are situated anterior to the vertebral column and receive inputs from splanchnic nerves as well as central sympathetic neurons.
The three collateral ganglia are the celiac ganglion, the superior mesenteric ganglion, and the inferior mesenteric ganglion.
An axon from the central neuron that projects to a sympathetic ganglion is referred to as a preganglionic fiber or neuron, and represents the output from the CNS to the ganglion.
A postganglionic fiber—the axon from a ganglionic neuron that projects to the target effector—represents the output of a ganglion that directly influences the organ.
The cells in the adrenal medulla that are contacted by the preganglionic fibers are called chromaffin cells.
Parasympathetic Division of the Autonomic Nervous System
The parasympathetic system can also be referred to as the craniosacral system (or outflow) because the preganglionic neurons are located in nuclei of the brain stem and the lateral horn of the sacral spinal cord.
The preganglionic fibers from the cranial region travel in cranial nerves, whereas preganglionic fibers from the sacral region travel in spinal nerves.
The targets of these fibers are terminal ganglia, which are located near—or even within—the target effector.
These ganglia are often referred to as intramural ganglia when they are found within the walls of the target organ.
In the midbrain, the Edinger–Westphal nucleus is part of the oculomotor complex, and axons from those neurons travel with the fibers in the oculomotor nerve (cranial nerve III) that innervate the extraocular muscles.
The preganglionic parasympathetic fibers within cranial nerve III terminate in the ciliary ganglion, which is located in the posterior orbit.
Neurons in the dorsal nucleus of the vagus nerve and the nucleus ambiguus project through the vagus nerve (cranial nerve X) to the terminal ganglia of the thoracic and abdominal cavities.
The postganglionic fibers from the ganglia activated by the vagus nerve are often incorporated into the structure of the organ, such as the mesenteric plexus of the digestive tract organs and the intramural ganglia.
Chemical Signaling in the Autonomic Nervous System
Synapses of the autonomic system are classified as either cholinergic, meaning that acetylcholine (ACh) is released, or adrenergic, meaning that norepinephrine is released.
The cholinergic system includes two classes of receptor: the nicotinic receptor and the muscarinic receptor.
The nicotinic receptor is a ligand-gated cation channel and the muscarinic receptor is a G protein–coupled receptor.
The adrenergic system also has two types of receptors, named the alpha (α)-adrenergic receptor and beta (β)-adrenergic receptor.
An additional aspect of the adrenergic system is that there is a second signaling molecule called epinephrine.
The Structure of Reflexes
One difference between a somatic reflex, such as the withdrawal reflex, and a visceral reflex, which is an autonomic reflex, is in the efferent branch.
The other part of a reflex, the afferent branch, is often the same between the two systems.
Afferent Branch: The afferent branch of a reflex arc does differ between somatic and visceral reflexes in some instances.
Efferent Branch
The efferent branch of the visceral reflex arc begins with the projection from the central neuron along the preganglionic fiber.
This fiber then makes a synapse on the ganglionic neuron that projects to the target effector.
Short and Long Reflexes
A long reflex has afferent branches that enter the spinal cord or brain and involve the efferent branches, as previously explained.
A short reflex is completely peripheral and only involves the local integration of sensory input with motor output.
Central Control
Central control of autonomic reflexes is different than for somatic reflexes. The hypothalamus, along with other CNS locations, controls the autonomic system.
The Hypothalamus
The hypothalamus is the control center for many homeostatic mechanisms. It regulates both autonomic function and endocrine function.
Output from the hypothalamus follows two main tracts, the dorsal longitudinal fasciculus and the medial forebrain bundle
The Amygdala: The amygdala is a group of nuclei in the medial region of the temporal lobe that is part of the limbic lobe.
The Medulla
The medulla contains nuclei referred to as the cardiovascular center, which controls the smooth and cardiac muscle of the cardiovascular system through autonomic connections.
The preganglionic sympathetic fibers that are responsible for increasing heart rate are referred to as the cardiac accelerator nerves, whereas the preganglionic sympathetic fibers responsible for constricting blood vessels compose the vasomotor nerves.
Drugs that Affect the Autonomic System
An important way to understand the effects of native neurochemicals in the autonomic system is in considering the effects of pharmaceutical drugs.
A chemical that the body produces to interact with those receptors is called an endogenous chemical, whereas a chemical introduced to the system from outside is an exogenous chemical.
Sympathetic Effect
A drug that enhances adrenergic function is known as a sympathomimetic drug, whereas a drug that interrupts adrenergic function is a sympatholytic drug.
Phenylephrine is known as an α1-adrenergic agonist, meaning that it binds to a specific adrenergic receptor, stimulating a response.
Drugs that interfere with sympathetic function are referred to as sympatholytic, or sympathoplegic, drugs. They primarily work as an antagonist to the adrenergic receptors.
Parasympathetic Effects
Drugs that enhance cholinergic effects are called parasympathomimetic drugs, whereas those that inhibit cholinergic effects are referred to as anticholinergic drugs.
Atropine and scopolamine are part of a class of muscarinic antagonists that come from the Atropa genus of plants that include belladonna or deadly nightshade.
 Knowt
Knowt