
Chapter 10: Dysphagia
Dysphagia
Dysphagia - a difficulty in swallowing or an inability to swallow
A swallowing problem affects a person’s ability to eat, which serves 2 primary purposes:
Nutrition and hydration
Pleasure
Dysphagia impairs a person’s ability to participate in social gatherings or events
Examples of Dysphagia
Aspiration - when food enters the airway
Aspiration occurs because - weak or paralyzed pharyngeal and laryngeal muscles
Role of the SLP
Approximately 30% of SLP are involved in the management of swallowing
SLPs are a key component of a dysphagia team (ENT, OT, SLP, radiologist, PT, primary care physicians, nutritionist, nurses)
Communication and swallowing problems co-occur because these two activities share some common structures and functions

Stages of Swallowing
The Anticipatory Stage
Occurs before the food reaches the mouth
Sensory information
“prepare to eat”
The Oral Stage
Voluntary control
Preparatory phase part of the oral stage, the bolus is being readied for the swallow
Transport phase begins when the tongue pushes the bolus against the palate, moving it in a backward direction toward the pharynx
The Pharyngeal Stage
Begins with the triggering of the pharyngeal swallow
Purposes - to protect the airway, to direct the bolus toward the stomach
Velum elevates and contracts to close off the velopharynx so that food cannot enter the nasal cavity
Larynx and hyoid bone move upward and forward
Larynx closes to prevent food from entering the airway
Epiglottis comes over the larynx to provide additional airway protection
When the swallow is triggered, pharyngeal peristalsis is initiated - contractions that move the bolus through the pharynx toward the esophagus
The Esophageal Stage
Begins with the lowering and backward movement of the larynx and the resumption of breathing
Upper esophageal sphincter contracts
Bolus moves through the esophagus to the stomach in a series of peristaltic waves
Dysphagia in Adults
Swallowing requires both cognitive and motor skills
Causes of Swallowing Disorders
Cerebrovascular Accident (CVA) - aka stroke
Brain Stem Stroke
TBI
Dementia - cognitive issues/hold food in mouth
Neuromuscular Disease - MS, ALS, PD, MG
Cancer - surgery changes the anatomy, radiation causes tissues to become “stiff”
Symptoms of Dysphagia
coughing or choking during swallowing
change in voice or speech (sounds gurgle-y)
repetitive swallows or progressive need to clear throat
regurgitation, immediate or delayed (pharyngeal and nasal or esophageal and gastric)
weakness; lack of control of head and neck musculature
fullness/tightness in throat
pain, localized or radiating (e.g., functional chest pain may occur in patients with somatic concerns, anxiety, or depression)
odynophagia (pain on passage of bolus)
Management of Adult Dysphagia
History
Bedside evaluation
Instrumental evaluation
Determine treatment plan based on these results
Team - SLP, OT, PT, nurses, nutritionists, radiologists, neurologists, gastroenterologists, pulmonologists
Assessment
Questions to be Determined
Is the patient aware of the food on his plate, can he feed himself?
Are the muscles of the tongue, lips, and jaw able to adequately prepare a bolus?
Do the pharyngeal and laryngeal muscles have enough strength and movement to elevate the larynx to close off the airway and direct the bolus to the esophagus?
Can the patient eat safely (with no aspiration) and maintain adequate nutrition?
History
Collect relevant feeding, behavioral, and medical information
Pre-existing conditions, medications
Medically stable?
Respiratory status
Current cognitive functioning
Current Medical Status
How the person is presently receiving nutrition
IV
NG tube - placed in the nose and goes to the stomach
G tube - tube surgically placed directly into the stomach
People can still aspirate on an NG or G tube if they have reflux
Bedside Clinical Assessment
Meets with the patient and assesses his/her ability to take food off the plate, prepare the bolus, and safely swallow
Oral Mech Exam, assesses ability to follow directions, level of alertness
Directly observe the oral phase
Unable to view the pharyngeal phase, but can watch for signs:
Neck along with placement of 2 fingers under the chin to determine whether there is upward and forward laryngeal movement
Listening for coughing, which would mean the bolus went down the wrong way
There could be a silent aspirator - they aspirate but do not cough
Listening for a “gurgly” sound after swallowing which might indicate that part of the bolus is on the vocal folds
Pharyngeal stage of the swallow can not be diagnosed by the bedside evaluation
When pharyngeal stage problems are suspected, the SLP can conduct an additional assessment procedures
Instrumental Assessment of Dysphagia
An instrumental assessment is used to gain a better understanding of pharyngeal stage functioning
Modified Barium Swallow Study (MBS/MBSS): this procedure is a fluoroscopic image that is recorded on videotape
SLP and radiologist perform this procedure together
SLP places barium coated food and liquids into the patient’s mouth
Radiologists takes a moving picture
Pharyngeal stage functioning can be visualized
Endoscopy (FEES)
Flexible scope is inserted through the nose and positioned just above the epiglottis
Patient is given food mixed with dye
Patient east the examiner observes the pharyngeal structures and functions
Treatment Planning
Team determines treatment
Plans often include:
Positioning - chin tuck
Environmental modifications - eat in a quiet environment (need more cognitive status to follow strategies)
Adaptive feeding equipment - Provale cup, Safe straw
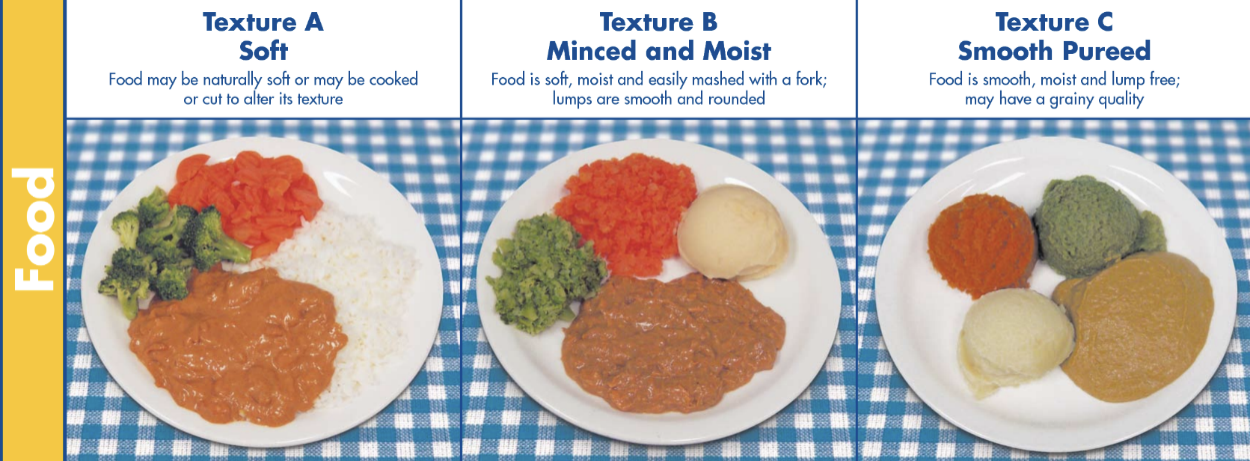
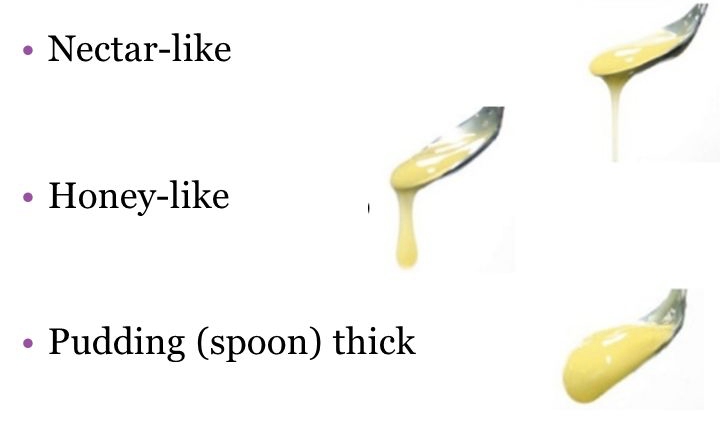
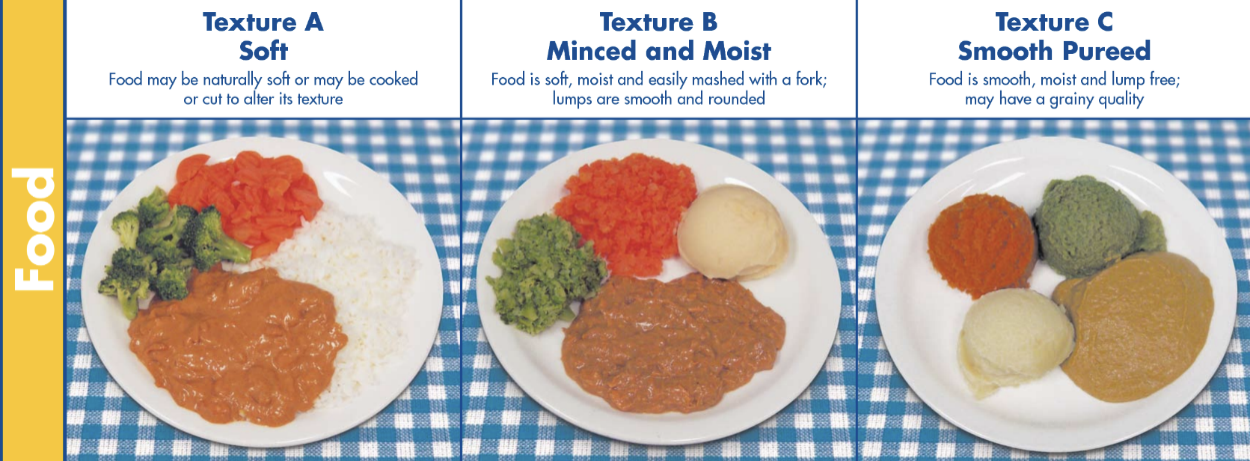
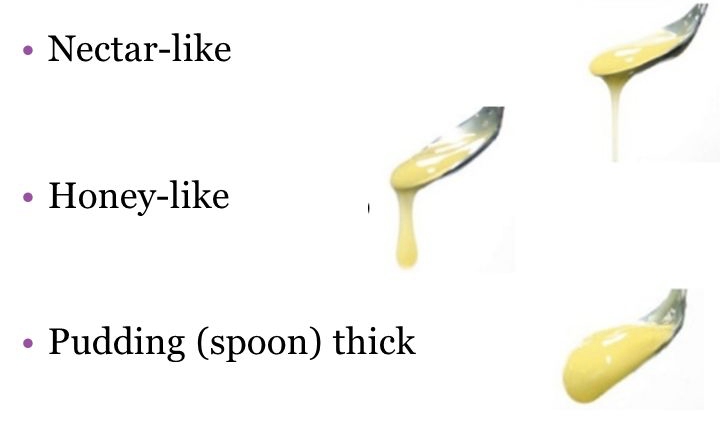
Bolus modification
Swallowing techniques - ex. effortful swallow - concentrate on tensing all of the throat during swallows
Chin Tuck - Decreases airway diameter
Safe Straw - Limits sip size
Provale Cup - Limits sip size
Examples of Modified Diets
Dysphagia in Children
Pediatric dysphagia: the SLP treats children who have yet to acquire normal eating skills
Various etiologies have prevented the development of normal swallowing patterns
Respiratory: suck/swallow/breathe
Sensory deficits: food textures
Cleft Lip/Palate
Goal of dysphagia assessment and treatment with children is to - Aid in the development of skills needed to keep the child safe and well nourished
Prematurity
Ability to suck/swallow develops prenatally
Premature baby may not have the ability to suck milk from a nipple
Weak facial muscles, underdeveloped lungs
Uncoordinated suck/swallow, weak suck, breathing disruptions
CP
Wide range depending upon the degree of motor deficit
Often see increase in muscle tone, decrease in ROM
Cognitive deficits
Child with CP is often a slow, inefficient eater with a high risk for aspiration
Pediatric Dysphagia Evaluation
Review Medical and Feeding History and Current Feeding Methods
Bedside Clinical Assessment
Instrumental Assessment
Conduct the MBS in the child’s current seating system
Use food textures that are similar to what the child currently eats
Use the child’s own utensils- bottle, special cup, spoon, etc.
Pediatric Treatment Planning
First goal - Child meet current nutritional needs while remaining safe so the child can grow and remain healthy
Second goal - Normalizing the child’s eating and swallowing skills
Dietician, SLP, Physical Therapist
Chapter 10: Dysphagia
Dysphagia
Dysphagia - a difficulty in swallowing or an inability to swallow
A swallowing problem affects a person’s ability to eat, which serves 2 primary purposes:
Nutrition and hydration
Pleasure
Dysphagia impairs a person’s ability to participate in social gatherings or events
Examples of Dysphagia
Aspiration - when food enters the airway
Aspiration occurs because - weak or paralyzed pharyngeal and laryngeal muscles
Role of the SLP
Approximately 30% of SLP are involved in the management of swallowing
SLPs are a key component of a dysphagia team (ENT, OT, SLP, radiologist, PT, primary care physicians, nutritionist, nurses)
Communication and swallowing problems co-occur because these two activities share some common structures and functions

Stages of Swallowing
The Anticipatory Stage
Occurs before the food reaches the mouth
Sensory information
“prepare to eat”
The Oral Stage
Voluntary control
Preparatory phase part of the oral stage, the bolus is being readied for the swallow
Transport phase begins when the tongue pushes the bolus against the palate, moving it in a backward direction toward the pharynx
The Pharyngeal Stage
Begins with the triggering of the pharyngeal swallow
Purposes - to protect the airway, to direct the bolus toward the stomach
Velum elevates and contracts to close off the velopharynx so that food cannot enter the nasal cavity
Larynx and hyoid bone move upward and forward
Larynx closes to prevent food from entering the airway
Epiglottis comes over the larynx to provide additional airway protection
When the swallow is triggered, pharyngeal peristalsis is initiated - contractions that move the bolus through the pharynx toward the esophagus
The Esophageal Stage
Begins with the lowering and backward movement of the larynx and the resumption of breathing
Upper esophageal sphincter contracts
Bolus moves through the esophagus to the stomach in a series of peristaltic waves
Dysphagia in Adults
Swallowing requires both cognitive and motor skills
Causes of Swallowing Disorders
Cerebrovascular Accident (CVA) - aka stroke
Brain Stem Stroke
TBI
Dementia - cognitive issues/hold food in mouth
Neuromuscular Disease - MS, ALS, PD, MG
Cancer - surgery changes the anatomy, radiation causes tissues to become “stiff”
Symptoms of Dysphagia
coughing or choking during swallowing
change in voice or speech (sounds gurgle-y)
repetitive swallows or progressive need to clear throat
regurgitation, immediate or delayed (pharyngeal and nasal or esophageal and gastric)
weakness; lack of control of head and neck musculature
fullness/tightness in throat
pain, localized or radiating (e.g., functional chest pain may occur in patients with somatic concerns, anxiety, or depression)
odynophagia (pain on passage of bolus)
Management of Adult Dysphagia
History
Bedside evaluation
Instrumental evaluation
Determine treatment plan based on these results
Team - SLP, OT, PT, nurses, nutritionists, radiologists, neurologists, gastroenterologists, pulmonologists
Assessment
Questions to be Determined
Is the patient aware of the food on his plate, can he feed himself?
Are the muscles of the tongue, lips, and jaw able to adequately prepare a bolus?
Do the pharyngeal and laryngeal muscles have enough strength and movement to elevate the larynx to close off the airway and direct the bolus to the esophagus?
Can the patient eat safely (with no aspiration) and maintain adequate nutrition?
History
Collect relevant feeding, behavioral, and medical information
Pre-existing conditions, medications
Medically stable?
Respiratory status
Current cognitive functioning
Current Medical Status
How the person is presently receiving nutrition
IV
NG tube - placed in the nose and goes to the stomach
G tube - tube surgically placed directly into the stomach
People can still aspirate on an NG or G tube if they have reflux
Bedside Clinical Assessment
Meets with the patient and assesses his/her ability to take food off the plate, prepare the bolus, and safely swallow
Oral Mech Exam, assesses ability to follow directions, level of alertness
Directly observe the oral phase
Unable to view the pharyngeal phase, but can watch for signs:
Neck along with placement of 2 fingers under the chin to determine whether there is upward and forward laryngeal movement
Listening for coughing, which would mean the bolus went down the wrong way
There could be a silent aspirator - they aspirate but do not cough
Listening for a “gurgly” sound after swallowing which might indicate that part of the bolus is on the vocal folds
Pharyngeal stage of the swallow can not be diagnosed by the bedside evaluation
When pharyngeal stage problems are suspected, the SLP can conduct an additional assessment procedures
Instrumental Assessment of Dysphagia
An instrumental assessment is used to gain a better understanding of pharyngeal stage functioning
Modified Barium Swallow Study (MBS/MBSS): this procedure is a fluoroscopic image that is recorded on videotape
SLP and radiologist perform this procedure together
SLP places barium coated food and liquids into the patient’s mouth
Radiologists takes a moving picture
Pharyngeal stage functioning can be visualized
Endoscopy (FEES)
Flexible scope is inserted through the nose and positioned just above the epiglottis
Patient is given food mixed with dye
Patient east the examiner observes the pharyngeal structures and functions
Treatment Planning
Team determines treatment
Plans often include:
Positioning - chin tuck
Environmental modifications - eat in a quiet environment (need more cognitive status to follow strategies)
Adaptive feeding equipment - Provale cup, Safe straw
Bolus modification
Swallowing techniques - ex. effortful swallow - concentrate on tensing all of the throat during swallows
Chin Tuck - Decreases airway diameter
Safe Straw - Limits sip size
Provale Cup - Limits sip size
Examples of Modified Diets
Dysphagia in Children
Pediatric dysphagia: the SLP treats children who have yet to acquire normal eating skills
Various etiologies have prevented the development of normal swallowing patterns
Respiratory: suck/swallow/breathe
Sensory deficits: food textures
Cleft Lip/Palate
Goal of dysphagia assessment and treatment with children is to - Aid in the development of skills needed to keep the child safe and well nourished
Prematurity
Ability to suck/swallow develops prenatally
Premature baby may not have the ability to suck milk from a nipple
Weak facial muscles, underdeveloped lungs
Uncoordinated suck/swallow, weak suck, breathing disruptions
CP
Wide range depending upon the degree of motor deficit
Often see increase in muscle tone, decrease in ROM
Cognitive deficits
Child with CP is often a slow, inefficient eater with a high risk for aspiration
Pediatric Dysphagia Evaluation
Review Medical and Feeding History and Current Feeding Methods
Bedside Clinical Assessment
Instrumental Assessment
Conduct the MBS in the child’s current seating system
Use food textures that are similar to what the child currently eats
Use the child’s own utensils- bottle, special cup, spoon, etc.
Pediatric Treatment Planning
First goal - Child meet current nutritional needs while remaining safe so the child can grow and remain healthy
Second goal - Normalizing the child’s eating and swallowing skills
Dietician, SLP, Physical Therapist
 Knowt
Knowt
