Law, Ethics and Professionalism
Pharmacy Oversight
History of Drug Regulation
In the 19th century, there was not regulation
Opium was liberally used in many medications.
No regulations protected consumers and many “medicines” made claims not backed by science
Laws, oversight agencies, and professional organizations emerged in the 20th century as a way to regulated medicine
Federal and state regulatory agencies include:
Health Canada
Health Protection Branch
Federal Trade Commission
Centers for disease Control and Prevention
Provincial Colleges of Pharmacy
Professional organizations include:
National association of Pharmacy Regulatory Authorities
Canadian Pharmacists Association
Canadian Society of Hospital Pharmacists
There are four primary types of oversight
Laws
Regulations
Standards
Ethics
Laws: overall all rules that are passed by the legislative branches of federal, provincial, and local governments to guide conduct
Regulations: Legislated rules and procedures that exist to carry out the law
Standard: Benchmarks or desired normal level of quality for a product or professional performance
Ethics: following a code of high professional standards
Drug: includes any substance or mixture of substances manufactured, sold or represented for use in:
(a) the diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals,
(b) restoring, correcting or modifying organic functions in human beings or animals, or
(c) disinfection in premises in which food is manufactured, prepared or kept; (drogue)
Professional Pharmacy Organizations & Associations
NBCP http://www.nbpharmacists.ca/
Establishes standards of knowledge and skill for members, keeping pace with medical and pharmaceutical advancements
Serves as the vehicle for public complaints about pharmacists and, where appropriate, provides disciplinary measures
Provides standards of qualification for licensed pharmacists and registered students
Provides standards of practice for licensed pharmacists, licensed certified dispensers and licensed students
Provides and ensures adherence to a code of professional ethics
Requires members to participate in professional development and training programs
Regulates the circumstances under which a licensed pharmacist may prescribe drugs, devices, and treatment and pharmacies may sell them
Establishes and maintains standards for the operation of pharmacies
Establishes regulations for practice agreements with other health professions
NBPA
similar to CPHA
able to purchase liability insurance cheaper
advocating to us as healthcare professionals
advocate to the insurance companies in the business side and image side
NAPRA-http://napra.ca/pages/home/default.aspx
Who they are?
Non profit association established in 1995
Membership includes all provincial/territorial regulatory authorities & the Canadian Armed Forces
Pharmacy Services
Mandate: to protect the public through regulation of pharmacy practice and operation of pharmacies Governed by a board of directors
What they do?
Maintain and administer the National Drug Schedules (NDS)
Develop national model standards, guidelines, frameworks to achieve a
harmonized practice frameworkFacilitate the development and maintenance of reciprocity frameworks for pharmacists
Represent and act as a national voice for pharmacy regulatory issues in Canada
Undertake initiatives of national importance on behalf of its members
CAPT-
http://capt.ca/
Deals with accreditation
Vision: CAPT is the national association providing an influential voice, leadership and support to pharmacy technicians and pharmacy support staff facilitating practice excellence contributing to positive health outcomes
Mission: CAPT will advocate and promote the role of the pharmacy technician and pharmacy support staff and the advancement of the profession CAPT will support and empower pharmacy technicians and pharmacy support staff in the pursuit of practice excellence through:
Communication
Education and professional development opportunities
Partnerships and collaboration with pharmacy stakeholders
PEBC
The Pharmacy Examining Board of Canada (PEBC) is the national certification body for the pharmacy profession in Canada.
PEBC is a non- profit organization with more than 45 years of experience in assessing the qualifications and competence of candidates for licensing by pharmacy provincial regulatory authorities.
The purpose of the Pharmacy Examining Board is to assess qualifications for pharmacists and pharmacy technicians on behalf of participating provincial regulatory authorities
The Board evaluates qualifications, develops and administers examinations
national Qualifying Examination
issues Certificates of Qualification
CPhA-http://www.cshp.ca/
The Canadian Pharmacists Association is the national organization of pharmacists, committed to advancing the profession of pharmacy so as to contribute to the health of Canadians . CPhA’s website is your link to a comprehensive source of drug information, pharmacy practice support material, patient information and news about the world of pharmacy
CSHP-http://www.cshp.ca/
Canadian society of Hospital Pharmacists is the national voice of Pharmacists' committed to the advancement of safe, effective medication use and patient care in hospitals and related health care settings.
ISMP- https://ismpcanada.ca/
The Institute for Safe Medication Practices Canada is an independent national not-for-profit organization committed to the advancement of medication safety in all healthcare setting
Neighborhood Pharmacy Association of Canada- http://www.neighbourhoodpharmacies.ca/
TLDR Run the business side of independent pharmacies to help prevent adverse drug reactions, operating an efficient supply chain and by providing innovative drug therapies and lower-cost generic drugs
They are: focused on the business of neighborhood pharmacy to ensure our members can continue to deliver the convenient, professional patient care products and services on which Canadians rely. Our commitment is repaid in trust, as 80% of Canadians consult their pharmacists for professional healthcare, at nearly 9,000 neighborhood pharmacies across the country.
They represent: the operators of Canada’s approximately 6,500 chain, banner and franchise neighborhood pharmacies, as well as grocery chains and mass merchandisers with pharmacies. Neighborhood pharmacy helps save the Canadian healthcare system more than $12.5 billion annually, preventing adverse drug reactions, operating an efficient supply chain and by providing innovative drug therapies and lower-cost generic drugs
They look at independent pharmacies
HPB
The Health Protection Branch is responsible for the development and implementation of legislation, policies and programs in the areas of Environmental Health Protection Community Care Facilities and Emergency Prepare
Legislation: Canada Health Act
CHA Objective
The Act sets out the primary objective of Canadian Health Care Policy
To protect, promote and restore the physical and mental well-being of residents of Canada and to facilitate reasonable access to health services without financial or other barriers
Was enacted by Health Canada in 1984 and represents the cornerstone of the Canadian Health System
Ensures that all eligible residents of Canada have reasonable access to insured health services on a prepaid basis, without direct charges at the point of service for such services
Provides for criteria and conditions that the provinces and territories must fulfill to receive the full federal cash contribution under the Canada Health Transfer (CHT)
Criteria:
To receive CHT each province/territorial health insurance plan must fulfill the following criteria/conditions
Public administration: must be carried out by a non profit/ by public authority
Comprehensiveness: all necessary services must be insured/covered
Universality: all persons insured must receive uniform coverage
Portability: insured services must be maintained when an insured person moves or travels
Accessibility: services must be unimpeded by financial or other barriers
Implementing the CHA
Provincial/Territorial Role
Canada does not have a single national health care plan, but rather a national health insurance program, which is achieved by a series of thirteen interlocking provincial and territorial health insurance plans, all of which share certain common features and basic standards of coverage
Under the Canada Health Act, our national health insurance program is designed to ensure that all residents of Canada have reasonable access to medically necessary hospital and physician services on a prepaid basis, and on uniform terms and conditions
Insured Services
Provincial and territorial health insurance plans are required to provide insured persons with coverage of insured health services, which are:
Hospital Services: provided to inpatients or outpatients, if the services are medically necessary for the purpose of maintaining health, preventing disease or diagnosing or treating an injury, illness, or disability
medically required physician services rendered by medical practitioners
Other Benefits
Provinces and territories may also offer "additional benefits" under their respective health insurance plans, funded and delivered on their own terms and conditions
These benefits are often targeted to specific population groups (e.g. children, seniors, social assistance recipients), and may be partially or fully covered
While these services vary across different provinces and territories, examples include prescription drugs, dental care, optometric, chiropractic, and ambulance services
Uninsured Services
A number of services provided by hospitals and physicians are not considered medically necessary, and are not insured by provincial and territorial health insurance plans
Uninsured hospital services for which patients may be charged include preferred hospital accommodation unless prescribed by a physician; private duty nursing services; and the provision of telephones and televisions
Uninsured physician services for which patients may be charged include prescription renewals by telephone; the provision of medical certificates required for work, school, insurance purposes and fitness clubs; testimony in court; and cosmetic services
Financing Health Insurance Service
Financing
Provinces and territories have considerable autonomy in determining how to finance health insurance plans
Financing can be addressed through the payment of premiums (as in British Columbia), payroll taxes, sales taxes, other provincial or territorial revenues, or by a combination of methods
Health insurance premiums are permitted as long as residents are not denied coverage for medically necessary hospital and physician services because of an inability to pay such premiums
Provinces/territories that levy premiums also offer financial assistance based on income so that low- income residents can have their payments reduced or be entirely exempted from paying premiums
Federal FDA
Food and Drugs Act
There are 4 Active Schedules
Schedule A: disease stated or conditions for which treatments may not be promoted to the public
asthma, cancer, depression, must comply with specific requirement if they are to be promoted as a treatment or cure
advertising is restricted
Schedule B: Publications describing official or international standards
Any drug or substance to be sold in Canada must meet this criteria and standards
Schedule C: radiopharmaceuticals
Schedule D: Allergenic substances, blood derivatives, immunizing agents
Schedule G: Controlled Drugs
Prescription Drug List
Drugs excluding those found in the Control Drug and Substance Act
FDA Regulations
The most important regulations for the pharmacy are the food and drug regulations, the Natural Health Products regulations and the medical devices regulations
Food and Drug Regulations
Part A: Administration
Part B: food production and food safety
topics such as baby food, alcohol, flavoring and daily products
also overseeing food safety and inspection
Part C: drugs and defined the rules for dispensing
from raw material to the final customers product
much of this part is directed to the manufacturers
Part D: vitamins, minerals and amino acids
Part E: cyclamen and saccharin sweeteners
Part G: controlled drugs
Part J: restricted drugs
For members of the pharmacy profession, the two key sections of the regulations are Part C, which deals with drugs and part G Controlled Drugs
Definitions Under the FDA
Practitioner: refers to a person who is entitled under the laws of a province to treat patients with a prescription drug and is practicing their profession in that province
Child Resistant Package: is a package that meets the child test protocol requirement of the Canadian Standards Association or other standards as specified in the Food and Drug Regulations.
The CSA is an organization that test, certified, and designates containers as child resistant
Part C Symbols
The requirements and symbols used for manufacturers labelling drug packages (i.e. stock bottles) are found in the Food and Drug Regulations.
Pr: refers to the product requiring a prescription for sale
N: narcotic
C: controlled Drug
TC: benzodiazepines or other targeted substances
Manufacturing
The process for approving a drug is regulated from beginning to end from:
providing the clinical evidence for efficacy and safety of the drug,
the raw materials used to manufacture the drug, and to
the final drug product
The Food and Drugs Act and the Food and Drug Regulations describe the regulatory requirements for manufacturers of drug products (i.e. pharmaceutical companies) including Good Manufacturing Practices (GMP)
Once a manufactured drug product is approved by Health Canada, it is given market authorization and a unique Drug Identification Number (DIN). The issuance of a DIN means a drug has been approved for sale in Canada.
Health Canada regulates the distribution of drugs through the issuance of Drug Establishment Licenses (DEL) which permit various activities such as:
fabricate or manufacture drugs;
package and/or label products;
test drugs;
distribute various classes of drugs:
import or wholesale drugs.
Inspections consist of premises, equipment, personnel, sanitation, raw material testing, quality control, finished product testing, sampling, stability, record keeping
Compounding
Are prepared pursuant to a prescription within an established pharmacist-patient relationship.
Require a consultation between the pharmacist and the patient (or patient's agent) in which the pharmacist uses their knowledge and expertise
Provide a customized therapeutic solution to improve patient care.
Do not circumvent a regulatory process or patent laws.
Manufacturing Vs Compounding
Manufacturing: regulated and enforced federally
Compounding: regulated by provincial regulatory authorities , in accordance with guideline and standards to ensure the quality and safety of compounded drug products
Health Canada's Policy on Manufacturing and Compounding Drug Products (POL-0051) provides information on the manufacturing and compounding of drugs in Canada.
Food and Drug Regulations
Health Canada provides warnings and advisories through its database (Recalls and Safety alerts Database) that lists recalls, advisories and safety alerts.
The mandatory health requirements that must be filed by Health Canada includes informing them of the nature of the recall and the actions that are being taken to remove the product
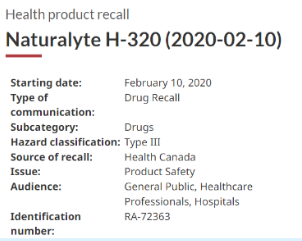
Types of Recalls
Health Canada’s Health Products and Foods Branch will determine what level or depth of recall is required. For drug recalls , this is listed as a Hazard Classification and is based on the risk of harm to the consumer.
Type I Recall
the most serious
This is a situation in which there is a reasonable probability that the use of, or exposure to, a product will cause serious adverse health consequences or death
example 1: medications with incorrect strength of label
Type II Recall
This is a situation in which the use of, or exposure to, a product may cause temporary adverse health consequences or where the probability of serious health consequences is remote.
example 2: foreign matter in tums
Type III Recall
This is a situation in which the use of, or exposure to, a product is not likely to cause any adverse health consequences.
example: incorrect image labeling
Suspected Adverse Drug Reactions
Suspected adverse drug reactions are also a mandatory reporting requirement for manufacturers. Any adverse reaction reports received by the manufacturer must be reported within 15 days to Health Canada. Reporting by the public or health professionals is voluntary although health professionals are encouraged to report adverse drug reactions to MedEffect ™ Canada through the Canada Vigilance Program
Canada Vigilance Program
The Canada Vigilance Program: is Health Canada’s post-market surveillance program that collects and assesses reports of suspected adverse reactions to health products marketed in Canada
This includes both prescription and non-prescription medications, natural health products and vaccines
In addition MedEffect also posts warnings, advisories and recalls that are in effect. When a number of reports are received for a certain drug , Health Canada may order a review of a product and take action where there is a potential risk to the public.
NAPRA
The National Association of Pharmacy Regulatory Authorities (NAPRA) manages and maintains the National Drug Schedules. Scheduling amendments made to the National Drug Scheduling System are immediately effective in New Brunswick
Scheduling amendments (changes) made to the National Drug Scheduling System based on some factors which include clinical experience with use of the product, its dose, package sizes or patient population i.e. adult use vs pediatric use
The National Drug Scheduling Advisory Committee adopted a cascading principle model whereby drugs are assessed, based on a number of risk factors, to determine whether they are considered Schedule I, II or III. If a product does not meet any of the factors to be scheduled, it is considered unscheduled (U).
ALL drugs in Schedule I, II or III MUST be sold in a pharmacy, but conditions for sale range from most strict in Schedule I which require a prescription, to the least strict in Schedule III where they can be sold in the self-selection area of the pharmacy
Products that are unscheduled (U) may be sold from any retail outlet.
Schedules
Schedule I Drugs
require a prescription
are the same as the drugs listed in Schedule I
Include all the drugs listed in Prescription Drug List (PDL)
Also including ALL of the drugs found in the Schedule of the Controlled Drugs and Substances Act
Schedule II Drugs: Only available through professional intervention by a pharmacist
Do not require a prescription
Kept in a restricted area of a pharmacy not accessible to the public
Schedule III Drugs: available without a prescription
However, they can only be sold in a pharmacy from the dispensary or from an area of the pharmacy (as required by the college) that allows for patient self selection.
A member of the college must be available if needed
Schedule U or unscheduled
May be sold without professional supervision or intervention
These substances are not included in Schedules I, II or III and may be sold from any retail outlet
Adequate information is available on the product packaging and labelling for the patient to make a safe choice and to ensure the patient uses the product appropriately
The Schedules change and it is important to keep updated
Monday
CSDA
Includes the Narcotic Control Regulations and the Regulations pertaining to controlled drug and restricted drugs
One law governs all drugs and substances in Canada, and all drugs and substances under this law are called Controlled Substances
The CDSA controls the manufacture of narcotics, controlled and targeted drugs in Canada and regulates the selling of these products from wholesalers and manufacturers to pharmacies
It also regulated who may prescribe controlled substances
a controlled drug is any drug list in the schedule to Part G of the Food and Drug Regulations
8 Schedules
Schedule I: Old Narcotic Schedule
Schedule II: Cannabis, its preparations and derivatives
Schedule III:
Schedule IV: old controlled drugs and targeted drugs
Schedule V: restricted use or banned in Canada
Schedule VI: Ephedrine, pseudoephedrine and 4 other drugs
Schedule VII: Cannabis resin up to 3 kg old Controlled Drugs
and Cannabis marihuana up to 30g
Schedule VIII: Cannabis resin up tp 1g and Cannabis marihuana up to 30g
Schedule I
opium
Codeine
Morphine
Hydrocodone
Cocaine
Methadone
Pentazocine
Fentanyl
Schedule III
Amphetamines
Methylphenidate
Methaqualone
LSD
Psilocybin
Mescaline
Schedule IV
Barbiturates and salts
Thiobarbiturates and salts
diethylpropion
phentermine
butorphanol
nalbuphine
meprobamate
benzodiazepine
anabolic steroids
Schedule VI
Ephedrine, pseudoephedrine and 4 other drugs
Precursor chemical- chemicals that are frequently used in illicit production of controlled substances
ex. ephedrine and pseudoephedrine, commonly used in cold and decongestant medicine, are precursor chemicals that are used to produce methamphetamine
Double Doctoring
an offence under the CDSA
Obtaining a Substance
s.4 (2) No person shall see or obtain a substance included in Schedule I-IV or an authorization to obtain a substance included in Schedules I-IV from a practitioner, unless the person discloses to the practitioner particulars, relating to the acquisition by the person of every substance in those Schedules, and of every authorization to obtain such substances**, from any other practitioner within the proceeding 30 days**
Double Doctoring: Getting a prescription without disclosing to the prescriber your prescription history
the patient MUST inform the prescriber of any controlled substances that they have been prescribed in the last 30 days
Ordering
Only a person with Signing authority may order controlled substances. Persons with signing authority include the owner/manager of the pharmacy or any other staff pharmacist
Any employee of the pharmacy can sign the manifest when controlled drugs are delivered to the pharmacy but the person with signing authority must sign for the drugs within 48 hours
Narcotic and Controlled Drug register
Narcotic and Controlled Drug Register: maintained in the pharmacy in either electronic format or manual format
the register consists of the Narcotic purchase record and the narcotic sales record. All controlled substance drugs must be recorded in the Narcotic Purchase Record
Reportable narcotics and controlled drugs need to be recorded in the narcotic sales record. This would include methadone sales
Sales Records are printed every 2 weeks and maintained on site for audit purposes
What is a Narcotic Drug
Any substance set out in the Schedule to the Narcotic Control Regulations, or anything that contains a substance listed in the schedule
Categories
narcotic drugs/ straight narcotics
Verbal prescription narcotic
OTC narcotic preparation
Filling Narcotic and Controlled Prescriptions
Narcotic and controlled prescription are filed by prescription number in a separate file from other prescriptions and are coded differently than regular prescriptions
If 2 medications are on the same prescription from, other original is stored with the narcotic while the copy is places with the regular prescriptions, cross referencing both prescription number
Narcotics and controlled drugs are to be kept in a locked cupboard or safe
Returning-Destroying Narcotics-Controlled Drugs
Expired drugs are based on manufacturer policy and with prior permission
part bottles can be destroyed and the destruction must be witnessed by a second person
Inventory is signed and dated by both the person destroying and the person witnessing the destruction with a copy placed in files for storage
OTC Narcotics= exempted Narcotics
OTC Narcotics will contain less than 8 mg of codeine if solid and 20mg/ 30ml if liquid and are to be stored in the non-patient access area of the pharmacy where the pharmacist can be involved in the sale of the product and the sale can be documented
Types of Narcotics and Controlled Drugs
Reportable Narcotics= straight narcotics= must be entered in Narcotic sales record
contains at least one Schedule I drug (N) + 1 other non-narcotic ingredient
injectable
from opium- containing heroin, hydrocodone, methadone, oxycodone
All products with pentazocine or dextropropoxyphene
verbal orderrefillspart-fills are allowed if quantity and interval are indicated
Transfers not permitted
NCR: Definition of Prescription
Prescription means, in respect of a narcotic, an authorization given by a practitioner that a stated amount of the narcotic be dispensed for the person named on the prescription
The quantity to dispense MUST be directly stated or it must be written in a way that an exact amount can be calculated
Possession
A person is permitted to possess a narcotic if
it for a Business or profession
receive pursuant to a prescription
if they are a hospital employee
employed as law enforcement- inspector, member of the Royal Canadian Mounted Police, police constable, peace officer or a part of the Government of Canada in purpose and connection with such employment
Narcotic Control Regulations
What is a “STRAIGHT” Narcotic
not defined in legislation
it is defined by what it is not by applying definition for verbal “backwards” and excluding otc narcotics
CONTAINS a single narcotic ingredient only, OR contain a narcotic and only ONE medicinal; ingredient other than a narcotic in a recognized therapeutic dose,
BE INTENDED for parenteral administration, OR
(CONTAIN hydrocodone, methadone, oxycodone or pentazocine
Verbal Narcotic Preparations= verbal prescription narcotics= non-reportable
contains 1 narcotic + 2 non-narcotic drugs
non-injectable
does not contain heroin, methadone, hydrocodone, oxycodone and pentazocine
no refills
part-fills allowed
no transfers
OTC Narcotics= exempted narcotic compounds
Codeine is only narcotic ingredient
less than 8 mg per solid dosses or 20 mg/30 ml in liquid
+2 other non-N ingredients
no Rx required
non-patient access area
sales may be documented
OTC Codeine Preparation (s.36)
(1)Subject to subsection (2), a pharmacist may, without a prescription, sell or provide a preparation containing not more than 8 mg or its equivalent of codeine phosphate per tablet or per unit in other solid form or not more than 20 mg or its equivalent of codeine phosphate per 30 mL in a liquid preparation if
(a) the preparation contains
two additional medicinal ingredients other than a narcotic in a quantity of not less than the regular minimum single dose for one such ingredient or one-half the regular minimum single dose for each such ingredient, or
three additional medicinal ingredients other than a narcotic in a quantity of not less than the regular minimum single dose for one such ingredient or one-third the regular minimum single dose for each such ingredient and
(b) there is legibly and conspicuously printed on the Inner label and the outer label, as those terms are defined in section A.01.010 of the Food and Drug Regulations, a caution to the following effect.
"This preparation contains codeine and should not be administered to children except on the advice of a physician, dentist or nurse practitioner
(2) No pharmacist shall sell or provide a preparation referred to in subsection (1) if the pharmacist has reasonable grounds to believe that the preparation is to be used for purposes other than recognized medical or dental purposes
NCR: Definition of Advertisement
Advertisement: any representation by any means hat ever for the purpose of promoting directly or indirectly the sale or disposal of a narcotic
Advertising of a narcotic to the general public is prohibited
NCR: Licensed Dealers
This section contains regulations pertaining to Licensed Dealers
No person except a licensed dealer shall produce, make, assemble, import, export, sell, provide, send or deliver a narcotic
License Dealer (wholesale Manufacturer) may sell/provide (not methadone) to:
another licensed dealer
pharmacist
practitioner
Hospital Employee
person with s.56 exemptions
*Methadone may be sold to all the above except the practitioner unless stipulated in s.56
Regulations in this section outline the requirement that a licensed dealer must meet in order to obtain a license, and outline the requirements they must meet in order to sell '
Regulations in this section pertain to but are not limited to
methods for ordering
information required to place an order
receipts: the licensed dealer must obtain a signed receipt from the purchaser within 5 working days
Purchaser requirements: the licensed dealer is only permitted to sell to persons registered with the Pharmacy Regulatory Authority
NCR: Pharmacist
This section contains regulations specific to Pharmacists
Regulations in this section pertain but are not limited to
receipt of narcotics
sale of narcotics
records of sale
refills of narcotic prescriptions
transcribing verbal orders
loss and theft of narcotics
Protection of narcotics
emergency supply
Destruction of Narcotics
OTC codeine preparations
Loss and Theft (s.42):
"A pharmacist shall report to the Minister any loss or theft of a narcotic within 10 days of his discovery thereof
Emergency Supply (s. 45)
A pharmacist may, on receiving a written order for a narcotic: > (b)sell or provide to another pharmacist the quantity of the narcotic that is specified in the order as being required for emergency purposes, if the order is signed and dated by the other pharmacist
(2) A pharmacist shall, immediately after returning, selling or providing a narcotic under subsection (1) or after receiving a narcotic under paragraph (1)(b) or subsection 65(4), enter the details of the transaction in a book, register or other record maintained for the purpose of recording such transactions...
Receipt of Narcotics
Process of Receipt of Narcotics (s.30)
A Pharmacist who receives a narcotic from a licensed dealer , shall immediately enter in a book, register or other record maintained for such purposes, the following:
Name of quantity of narc received
was it was received
name and address of person it was received from
Sale of a Straight Narcotic (S.31)
A pharmacist may sell or provide a narcotic other than methadone or dried marihuana to a person
if a person is exempted under section 56 of the act with respect to the possession of that narcotic or
If the pharmacist has first received a written order or prescription therefor signed and dated by a practitioner and the signature of the practitioner, where not known to the pharmacist, has been verified by him
Refills (s.37)
A pharmacist shall not use an order or prescription, written or verbal, to dispense a narcotic after the quantity of the narcotic specified in the order of prescription has been dispensed
Record of Sale (s.38)
Where, pursuant to a written order or prescription, a pharmacist dispenses a narcotic, other than dextropropoxyphene or a verbal prescription narcotic, the pharmacist shall forthwith enter in a book, register or other record maintained for such purposes
the name and address of the person named in the order or prescription:
the name, quantity and form of the narcotic;
the name, initials and address of the practitioner who issued the order or prescription;
the name or initials of the pharmacist who sold or provided the narcotic
the date on which the narcotic was sold or provided, and the number assigned to the order or prescription
Prescription Filling (S.40)
"A pharmacist shall maintain a special narcotic prescription file in which shall be filed in sequence as to date and number all written orders or prescriptions for narcotics dispensed and the written record of all verbal prescription narcotics dispensed pursuant to a verbal order or prescription..."
"A pharmacist shall retain in his possession for a period of at least two years any records which he is required to keep by these Regulations"
Narcotic Sales Registry and Filling
Record the amount dispensed on that day only and original Rx #
Typically done with end of day report in your pharmacies computer
All narcotic prescription must be filed separately from regular prescription
if both a narcotic and regular med on 1 Rx, file original with narcotics and a reference in the regular prescription
Receiving Narcotic Orders
shipped separately
invoiced separately
must order using pharmacist narcotic order #
Invoice must be signed and returned by pharmacist
all narcotics must be stored in locked area
…
Request for Destruction of Narcotics
Destruction of Narcotics and Controlled Drugs
Narcotic and Controlled drugs to be destroyed shall receive prior authorization from health Canada and, at the time of destruction, shall be witnessed and documented by two health care professionals
Destruction
Loss reported within 10 days
TLDR excess of a narcotic that was already given to a patient doesn’t need to be witness as long as it is documented
the remainder of an open ampoule, the partial content of which has been administered to a patient, may be destroyed by a licensed health professional without a witness. Such a destruction needs to be documented. As part of the security measures in place and in order to prevent diversions, a hospital may choose to increase this regulatory requirement.
Narcotic and Controlled medication to be destroyed locally, since 2016, do not require prior authorization from Health Canada but at the time of destruction, shall be witnessed and documented by two health care professionals (one must be pharmacist)
Records maintained for 2 years
Reportable Controlled Drugs= Straight Controlled Drugs= Reportable Sales Record
Drugs that are CNS stimulants such as Ritalin or Dexadrine or amphetamines
Repeats allowed on written if indicated # of repeats and time interval
no repeats allowed on verbal prescriptions
no transfers allowed
combinations containing more than one controlled drug
Controlled Drug Regulation
Found under Food and Drug Regulation Part G
Drug labels must have the Rx symbol
Schedule to Part G of FDR has 3 sections
Part I: amphetamines, methylphenidate plus secobarbital and pentobarbital
Part II: barbiturates and their salts and derivative excluding secobarbital and phenobarbital
Part III: anabolic steroids and derivatives
Controlled Drug Preparations= one Controlled Drug + 1 or more medicinal ingredients
not reportable in sales record
repeats on written if authorized in writing the # of repeats and time interval
No repeats on verbal
transfers not permitted
Controlled Drugs: Schedule IV
barbiturates (except secobarbital and pentobarbital) and other controlled including butorphanol
Anabolic Steroids
Repeats on verbal and written allowed if # of repeats & time interval
Transfers not permitted
Example: Phenobarbital, butorphanol
Benzodiazepines and other Targeted Substances
non reportable
filled with regular prescription
repeats allowed
can only be transferred once
Schedule F drugs= Regular Prescription Drugs
refills allowed
non-reportable
verbal and written Rx
Benzodiazepines and Other targeted Substances Regulations
Benzodiazepines and Other targeted Substances Regulations were implemented in September 2000
Symbol on stock bottle
You can still file Rx records with either N/CD or regular
Regulations in this section pertain to, but are not limited to
refills
sales
prescription transfers
Sale to Another Pharmacy
A quantity may be sold to another pharmacist if the other pharmacist states that the targeted substance is required because of a delay or shortfall in an order for the targeted substance (s. 55 (b) )
Refills: are permitted if number of refills is specific, a record is kept of each refill, less than one year has elapsed since the day on which the prescriber was issued by the practitioner (s.52)
Must abide by any intervals notes by the prescriber
Prescription transfer: A pharmacist may transfer a prescription for a targeted substance to another pharmacist, except a prescription that has already been transferred (S.54)
Destruction (s. 2(2).
There is no need to contact the Compliance, Monitoring, and Liaison Division to request destruction of T/C
Quantities to be destroyed must be recorded
Destruction must be witnessed
Pharmacist, practitioner or individual in charge of a hospital may destroy
Exception: remainder of an open ampoule if the partial contents were administered to a patient in hospital
A pharmacist, a practitioner or the individual in charge of a hospital may destroy a targeted substance if
(a) before the destruction, the pharmacist, practitioner or individual records information with respect to the destruction, including the name, strength per unit and quantity of the targeted substance to be destroyed;
(b) the targeted substance is destroyed using a method of destruction that conforms with all applicable federal, provincial and municipal environmental legislation;
(c) the person records the date of destruction;
(d) subject to subsection (3), the destruction is witnessed by a pharmacist or a practitioner; and
(e) immediately following the destruction, the person who destroyed the targeted substance and the witness referred to in paragraph (d) sign and print their names on a joint statement, indicating that they witnessed the destruction and that the targeted substance destroyed has been altered or denatured to such an extent that its consumption has been rendered impossible or improbable.
NAPRA Guidelines
Perpetual inventory
Manual inventory every 3 months or when changing managers
triplicate prescription program
should discrepancies be identified during inventory counts, the manager shall record the incident on an "incident report" and keep a record at the pharmacy. The manager shall initiate the necessary steps to identify the cause of the shortage, the responsible staff person and the initiate corrective actions. Significant shortages or diversion incidents must be reported to the M.Ph.A. and Health Canada.
Where a patient reports a shortage in their prescription, the inventory control system would verify or refute the shortage. If the prescription is re-dispensed, documentation of the date, time and reason for re-dispensing shall be noted on the prescription and cosigned by the manager and, except in sole practice situations, one other pharmacist.
When a breakage occurs, a report shall be filed on the pharmacy records of perpetual inventory, as a negative quantity. Documentation of the date, time and place of breakage could be co-signed by the manager and, except in sole practice situations, one other pharmacist.
NB Narcotic and Controlled Drug Storage Guidelines
If significant quantities of narcotic or controlled drug products are kept on hand, the bulk of these products should be kept in a safe or locked cabinet.
Narcotic or controlled drug products that are stored in open shelf areas should be dispersed with regular prescription inventory, rather than in one localized shelf area.
The intent of this directive is to prevent or minimize the loss of a significant quantity of product and increase the time necessary to collect the product in the event of a robbery, while not endangering staff faced with such a situation.
This directive does not prevent a pharmacy from choosing to store all narcotic and controlled drug products in a safe or locked cabinet.
CDSA Controlled Drugs and Substances
the controlled drug and substance act is a federal law
applies to the handling of controlled substances in Canada
Loss or theft: reports of any loss or theft of controlled substance or precursors must be submitted to health Canada Office of Controlled Substances (OCS)
Reports of any loss or theft of controlled substances or precursors must be submitted to Health Canada's Office of Controlled Substances (OCS).
Post-Consumer Returns
Post-consumer returns must be received by a pharmacist, pharmacy intern, or pharmacy technician.
Post-consumer returns must be stored in a one way entry container that has a unique identifier. It is recommended that the container is also opaque, inconspicuous and tamper evident.
Containers must be kept in the pharmacy dispensary when in active use and access should be limited to pharmacy staff. Should there be limited space inside the dispensary, the containers may be placed outside of the dispensary as long as they are in plain sight of the pharmacy staff and secured to the floor.
Pharmacists are also encouraged to use other means to enhance security in and around the dispensary area, such as the installation of security cameras.
Post-consumer returns must be received by a pharmacist, pharmacy intern,
or pharmacy technician.Pharmacists are not required to send destruction requests to Health Canada in order to proceed with local destruction.
Pharmacists performing local destruction must follow all applicable municipal, provincial and federal environmental laws and the destruction must render the controlled substances unusable.
Pharmacists should be aware that the destruction process may vary from substance to substance depending on the chemical or physical properties of the substance in question, however a change of state is recommended (i.e., from solid to liquid).
Pharmacists are encouraged to consult Workplace Hazardous Materials Information System (WHMIS) sheets or their respective provincial regulatory colleges for instructions on the appropriate method of destruction of controlled substances.
Once subjected to local destruction, post-consumer returns may be placed in an appropriate container and disposed of in a manner that is safe, environmentally responsible, secure and compliant with legal and professional requirements to protect confidential patient information. Already denatured products need not be sent to licensed dealers for disposal and can be placed in the regular pharmaceutical waste.
All local destructions must be witnessed by a practitioner, pharmacist, a pharmacy intern, or a pharmacy technician.
Pharmacists carrying out local destruction of post-consumer returns must record the date the destruction took place, the unique identifier of the container and the number of containers destroyed.
Records for the local destruction of post-consumer returns should be kept separate from those for post-consumer returns being sent to a licensed dealer.
The generated record must be signed by the pharmacist who carried out the destruction
and the witness present. The destruction must be witnessed in duplicate by the individual
destroying the substances and any other practitioner, pharmacy intern, or pharmacy
technician. Both persons must sign and print their names on the generated record and
indicate that they witnessed the destruction and that the substance was altered or
denatured to such an extent that its consumption was rendered impossible or improbable.This information must be recorded in a register similar to that required to be kept for
orders involving narcotics, controlled drugs and targeted substances, and must be
retained for a period of at least two years, in a manner that permits an audit to be made
35 day Regulation
A pharmacist shall dispense no more than a thirty five-day supply of narcotics, controlled drugs or benzodiazepines to any client. This does not apply to drugs indicated for and being used for the prevention and/or treatment of seizure disorders. Where the signa on the prescription is not clearly defined with respect to days’ supply, the pharmacist shall dispense no more than thirty-five doses.
A pharmacist may dispense more than a thirty-five-day supply of medication provided that (a) in the member’s professional judgement it is safe to do so; and (b) the prescriber has specified the exact quantity to be dispensed in excess of the thirty-five-day limit and has stated a reason for ordering that quantity.
NBCP- Regulations: https://nbpharmacists.ca/wp-content/uploads/2023/02/2022-REGS-bilingual-Nov-2022-Formatted.pdf?x43718
Definitions
Act: means the NB Pharmacy Act
ACPE: means the Accreditation Council for Pharmacy Education
Apprentice: means a registrant in a conditional register or a student (pharmacist or technician) who has entered into training with a preceptor in order to become a pharmacist or pharmacy technician.
Biologicals: means medicinal preparations made from living organisms and their products, which include, but are not limited to serums, vaccines, antigens, antitoxins.
CCAPP: means the Canadian Council of Accreditation of pharmacy programs.
Child resistant container: means a container that meets the Canadian Standards Association standards for child resistant containers
Close supervision: means supervision requiring direct contact with the supervised individual (member, employee) in person for most of the work period at the workplace.
Collaborative practice: means a practice setting in which a member works closely and cooperatively with one or more health professionals.
Collaborative practice agreement: means a written agreement between a pharmacy tech or pharmacists, and one or more health professionals.
Device: means any article, instrument, apparatus or contrivance, including any component, part or accessory thereof, manufactured, sold or represented for use in
The diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals
Restoring, correcting or modifying a body function or the body structure of human beings or animals
The diagnosis of pregnancy in human beings or animals
The care of human beings or animals during pregnancy and at and after birth of the offspring, including care of the offspring
And includes a contraceptive device but does not include a drug
Dispensary: means the area of a pharmacy where
drugs listed in Schedule I and II are stored for sale and/or prepared for dispensing.DIS/PMP: means the provincial drug information/prescription monitoring program.
Drug preparation activities: means reconstituting, diluting or otherwise preparing a drug or combining, admixing or mixing together two or more substances, at least one of which is a drug, to create a final product for the purpose of the sale or provision to another person, other than pursuant to or in anticipation of a prescription
Drug preparation premises: means any place where drug preparation activities take place
under the supervision of a pharmacist which complies with a regulatory framework in that jurisdiction but does not include:(a) a pharmacy in respect of which a certificate of operation has been issued by the regulatory body for that jurisdiction;
(b) a premises in respect of which a valid establishment license has been issued under the Food and Drug Regulations to the Food and Drugs Act (Canada)
Electronic signature: means an electronic sound, symbol, or process attached to or logically associated with a record and executed or adopted by a person with the intent to sign the record. The signature may also be “stylus on screen”. Reproduced images (jpeg, etc.) of signature are not acceptable.
Electronic transmission: of a prescription means communication of an original prescription or refill authorization by electronic means, to include computer-to computer, computer-to-facsimile machine, facsimile machine to facsimile machine, facsimile machine to computer or e-mail transmission which contains the same information it contained when the authorized prescriber transmitted it, but does not include a telephoned order
General supervision: means supervision requiring direct contact with the supervised individual (e.g. member, employee) in person at least monthly with supervision available as needed by other methods.
Pharmacist: Direct Client Care” means a pharmacist in active practice that had direct contact with clients for at least 400 hours during the preceding two-year period
Non-Direct Client Care” means a pharmacist in active practice who does not meet the criteria of a Pharmacist –Direct Client Care (e.g. pharmacists in administrative, management or other nondirected client care positions)
Pharmacy Technician: Direct Client Care” means a pharmacy technician in active practice, under the supervision of a Pharmacist – Direct Client Care, for at least 400 hours during the preceding two-year period
Non-Direct Client Care” means a pharmacy technician in active practice who does not meet the criteria of a Pharmacy technician – Direct Client Care (e.g. pharmacy technicians in administrative, management or other non-direct care positions). Definitions continued
PRA: means a Pharmacy Regulatory Authority of a Canadian province or territory
Preceptor: means a member who
(a) is a member in good standing;
(b) is registered to practice pharmacy in a location approved by Council;
(c) has been registered for a minimum of one year with the College;
(d) has no restrictions on the right to practice; and
(e) meets the requirements of section 12.23
Record: means the records of a pharmacy, whether in written, photographic, magnetic, electronic or other form, and includes, without limitation
(a) the records of the proprietor of the pharmacy, the manager, the regulated members engaged by the proprietor or any other person associated with the pharmacy;
(b) any record required to be kept under the Act, the Controlled Drugs and Substances Act (Canada) or the Food and Drugs Act (Canada) or the regulations or standards under those acts
(c) a record of all prescriptions the pharmacy receives, including an identification of the prescriptions that the pharmacy transfers to another pharmacy or pharmacist;
(d) a record of all drugs dispensed from or through the pharmacy, including the prescription, the name of the drug, the amount dispensed, the name and contact information of the client and the name and contact information of the prescriber;
(e) a record of the pharmacy services provided, including the name of the person or persons who dispensed a drug, or provided a pharmacy service;
(f) a record of the names and contact information of the clients to whom pharmacy services are provided; and
(g) a record of the counselling services provided to a client
Registrant: means a person whose name is entered on any register
Routine supervision: means supervision requiring direct contact with the supervised individual (e.g. member, employee) in person at the work site at various times throughout the work period with indirect contact occurring by other methods, such as telephone or written communication.
Supervision: as defined in the Act, includes close supervision, routine supervision or general supervision, as the case may be
Part II Council
Council shall consist of:
Voting councilors, being:
(i) the President,
(ii) the immediate past-president, or a former president appointed by Council if the past-president is unable or unwilling to serve,
(iii) seven elected pharmacists,
(iv) two elected pharmacy technicians
(v) three lay representatives appointed by the Minister
non-voting councilors, as appointed by Council, who may participate in debate, but are not entitled to vote on any matter before Council, being:
(i) at least one representative of a school of pharmacy
(ii) “ex officio” representatives in the number determined by Council, who shall serve for terms set by Council and at the will of council
Disqualification
2.2 The following persons are disqualified from being councilors:
(a) a person who is less than 19 years of age
(b) a person who is of unsound mind and has been so found by a court in Canada or elsewhere;
(c) a person who is not an individual;
(d) a person who is on the staff of the College
(e) a person who has the status of bankrupt;
(f) a member on a conditional register;
(g) a person convicted of an offence under
(i) the Criminal Code of Canada,
(ii)the Narcotic Control Act (Canada),
(iii) the Food and Drugs Act (Canada),
(iv) the Controlled Drugs and Substances Act, or
(v)the criminal law of any jurisdiction outside of Canada
Members of Council
2.3(1) Pursuant to section 7 of the Act, the
membership shall elect to Council, for two year terms commencing at the conclusion of the annual general meeting
(a) seven pharmacists; and
(b) two pharmacy technicians. 2.3(2) Pursuant to section 8 of the Act, the
Minister shall appoint three lay representatives, for a three-year term commencing at the close of the annual general meeting following their appointment, and may be re appointed for one additional term. (2016)
2.3(3.1) Each elected councilor ceases to hold office at the close of the second annual general meeting following the councilor’s election. (2016)
2.3(3.2) Each lay representative ceases to hold office at the close of the third annual general meeting following the councilor’s appointment. (2016)
2.3(4) No pharmacist or pharmacy technician may be elected to more than five consecutive terms on Council
2.3(5) Presidents, Presidents-Elect or Past Presidents who complete five consecutive terms on Council shall remain on Council until each completes their term as Past-President, resigns or becomes otherwise disqualified. (2018)
Officer and Duties
3.3(2) The President-Elect shall assume the office of President commencing at the end of the preceding President’s term of office
3.3(7) The President-Elect shall:
(a) be vested with all the powers and perform all the duties of the President in the absence, disability or refusal to act of the President;
Removal from office
3.4(1) Any five councilors may seek the removal from office of the President or President-Elect by delivering to the Registrar a notice in writing stating the reason for the proposed removal.
3.4(2) The Registrar shall, upon receipt of such notice, deliver a copy of the notice to the President or President-Elect affected.
3.4(3) Council may, after being satisfied that reasonable notice has been given under subsection 3.4(2), and by the vote of two thirds of those councilors present and eligible to vote on the matter, remove the President or President-Elect from office
Meeting of Council
4.1 Council shall hold at least three meetings annually, one of which is held at the conclusion of the Annual General Meeting.
4.2(1) Meetings of Council may be called from time to time by the order of the President or at the written request of three or more councilors to be held at any convenient place
4.2(2) Notice of meetings of Council shall be delivered by e-mail, by facsimile, electronically or by any other generally accepted means by the Registrar to each member of Council not less than one week before the time appointed for such meeting.
4.2(3) Meetings of Council may be held from time to time without formal notice if all councilors are present, or those absent have signified their consent to such meeting being held in their absence
4.3 The accidental omission to give notice of a meeting to any councilor or the nonreceipt of the notice by any councilor does not invalidate anything done at the meeting.
4.4 A meeting of Council may be held in person, by conference call, video conferencing or other method that ensures that the councilors all have the opportunity to participate in the meeting
4.8 Council shall maintain a policy on the use of in camera for all, or parts, of a meeting
Council members only;observers have to leave
Part V Committees
5.1(1) Council may appoint standing and special committees in addition to those committees required by the Act.
5.1(2) Committees may select their respective Chair unless determined otherwise by legislation, or by Council.
5.1(3) Those serving on Committees need not be members of the College.
5.1(4) Council shall approve Terms of Reference for all committees
Finance Committee
5.2 Council shall appoint a Finance Committee responsible for advising Council on matters pertaining to finance, including budgets, internal controls, investments, staff compensation, and any other matter designated by Council
Continuous Professional Development Committee
5.3 Council shall appoint a Continuous Professional Development Committee to guide and ensure that members registered to practice pharmacy maintain and improve their skills and knowledge base on an on-going basis
Governance Committee
5.4 Council shall appoint a Governance Committee to monitor the functioning of
Council, develop governance policies and ensure policies are followed
Registration Committee
5.6 Council shall appoint a Registration Committee to assess applications for membership and establish requirements that applicants must meet to be entered on a register.
5.7(1) If the term of a Registration Committee member expires before the Committee
concludes a matter before it, the Committee member whose term has expired shall
continue to be a member of the Committee until the matter is concluded by the Committee
Inquiries
5.8 At the request of the Registrar, the Registration Committee shall inquire into
(a) an application for enrolment as a member;
(b) an application for reinstatement in the College by a former member; and
(c) an application for transfer by a member from one register to another
Refusal
5.16 The Registration Committee may direct the Registrar to refuse to issue a certificate and/or registration to, or enter on a register, any applicant who
(a) has been the subject of a decision of a Canadian court finding the applicant guilty of a criminal offence which, in the reasoned opinion of the Registration Committee, is related to the practice of the profession, unless the applicant has obtained a pardon;
(b) has been the subject of a decision of a foreign court finding the applicant guilty of an offence which, if committed in Canada, could have led to criminal proceedings and which, in the reasoned opinion of the Registration Committee, is related to the practice of the profession, unless the applicant has obtained a pardon;
(c) has been the subject of a disciplinary decision by a Complaints or Discipline and Fitness to Practice Committee of another regulatory body, imposing the revocation of a certificate and/or registration; or
(d) has been the subject of any other matter deemed to be significant by the Registration Committee
Restriction or Suspension
5.17 The Registration Committee may direct the Registrar to enter an applicant on a register, but restrict or suspend the applicant’s right to engage in professional activities, if that applicant
(a) is the subject of a disciplinary decision made by the Complaints Committee or the Discipline and Fitness to Practice Committee;
(b) does not meet all of the established criteria for suspension
Restriction or Suspension
(c) is the subject of a disciplinary decision made outside New Brunswick which, if made in New Brunswick, would have had the effect of a restriction or suspension of the right to engage in professional activities imposed by the Complaints Committee or Discipline and Fitness to Practice Committee;
(d) is or has been, as the case may be, the subject of a decision described in section 5.16; or
(e) requests restrictions on, or suspension of, the applicant’s registration
Part VI-Codes of Conduct
Governance
6.1(1) The Governance committee is responsible for developing, and monitoring compliance with, a Code of Conduct (including conflict of interest) and procedures for councilors and of Committees
6.1(2) All councilors, officers and committee members shall exercise the powers and discharge the duties of their office honestly, in good faith, and in the best interest of the College in accordance with the approved Code of Conduct, and in connection therewith shall exercise the degree of care, diligence and skill that a reasonably prudent person would exercise in comparable circumstances.
6.1(3) Each councilor, committee member and office staff shall conduct himself or herself with utmost integrity and professionalism and ethically in relations with the public and……
Conflict of Interest
6.2(1) Council shall ensure a Conflict of Interest policy (part of Code of Conduct) is in place.
6.2(2) Each councilor shall review the Conflict of Interest Policy at least once per year and shall affirm that they have reviewed the policy by completing and signing a conflict-of-interest policy agreement form designated by Council.
6.2(3) A councilor shall abstain from voting or attempting to influence the vote on any matter before Council that places him/her in a conflict of interest.
6.3 Members and managers shall avoid conflicts of interest in their practice
6.4 Subject to section 6.5, a manager or pharmacist is in a conflict of interest,
(a) where a reasonable person knowing the relevant facts would conclude or perceive that the action of the pharmacy in relation to the provision of services was adversely influenced or would likely have been adversely influenced by the financial interests of the pharmacy or of a related person or a related corporation
(b) where the pharmacy or a related person or a related corporation enters into an arrangement or agreement which a reasonable person knowing the relevant facts would conclude or perceive would likely have the effect of adversely influencing the exercise of a member’s professional judgment or influencing or impeding a member’s ability to engage in the practice of pharmacy in an ethical manner or in accordance with the standards of practice of the profession
c) where the pharmacy or a related person or a related corporation enters into an arrangement or agreement which a reasonable person knowing the relevant facts would perceive as directly or indirectly influencing or encouraging a prescriber to promote the use of the pharmacy by a client; or
(d) where the pharmacy or a related person or a related corporation
(i) accepts or receives a benefit by reason of the referral of a client to any other person,
(ii) offers or confers a benefit to a person by reason of the referral of a client to the pharmacy, or
(iii) offers or confers a benefit including but not limited to loyalty programs or redeemable incentives to a client in relation to the sale of a drug referred to in Schedule I or the provision of professional pharmacy services other than
(A) an adjustment in the fee or amount that would otherwise be charged by the pharmacy with regard to that client for that drug or that professional pharmacy service, or
(B) the provision to a client, at no charge, of an item of a nominal value, to be used in maintaining or promoting well-being or health.
Professional Misconduct
6.7 In addition to those activities enumerated in the Act, professional misconduct includes, but is not limited to, the following:
(a) contravening, while engaged in the practice of pharmacy, any federal or provincial law or regulation with respect to the distribution, sale or dispensing of any drug or mixture of drugs;
(b) breach of the Code of advertising;
(c) practicing without maintaining the required professional liability insurance;
(d) failing to pay the appropriate fees to practice pharmacy;
(e) engaging in a conflict of interest;
(f) failing to maintain the Standards of Practice of the profession;
(g) failing to respond to a communication from the Registrar (or designate), or the Administrator of Complaints;
(h) refusing to allow an appointed person to enter at a reasonable time the pharmacy in which the member is engaged in the practice of pharmacy for the purpose of an inspection;
(i) displaying a lack of knowledge, skill or judgment, or disregard for the welfare of the public of a nature or to an extent that demonstrates a member is unfit to carry out the member`s responsibilities; (2017)
(j) selling or dispensing an excessive or unreasonable or improper amount of a drug;
(k) abusing a client, verbally, emotionally, or physically;
(l) discontinuing professional services that are needed, without reasonable cause, unless
(i) the client requests the discontinuation,
(ii) alternative services are arranged, or
(iii) the client is given a reasonable opportunity to arrange alternative services
(m) breaching an agreement with a client relating to professional services for the client, or fees for such services;
(n) falsifying a record in respect of a prescription or the sale of a drug;
(o) sharing fees with a person who has referred a person to a member or to a pharmacy or receiving fees from a person to whom a member has referred a person
(p) participating in a lease of premises for a pharmacy that permits a person other than a member or the owner of the pharmacy to participate in the revenue of the pharmacy except by way of a rent normal for the area in which the premises are located;
q) knowingly submitting a false or misleading account or false or misleading charge for a drug, the compounding of a drug product or dispensing of a prescription;
(r) signing or issuing a certificate or similar document that contains a statement the signing or issuing member knows or ought to know is misleading;
(s) announcing or holding out by a member that the member has special qualifications that are not in fact possessed by the member;
(t) except as specifically permitted in these Regulations, returning to stock or again selling or dispensing a drug previously sold or dispensed and delivered, or a medication sample, or outdated pharmaceutical products
(u) using improperly the authority to sell or dispense a drug or mixture of drugs;
(v) acting as a member while the ability to perform an action as a member is impaired by any substance;
(w) knowingly permitting the premises in which the pharmacy is located to be used for unlawful purposes;
(x) permitting, consenting to or approving either expressly or by implication the commission of an offence under the Act or these Regulations by another person associated with the pharmacy in which the pharmacist practices;
(y) falsifying a record, or failing to maintain the records that are required to be kept respecting clients
z) purchasing a drug other than from a legally authorized source;
(aa) disclosing of information relating to selling or dispensing of drugs to a person other than the person to whom the drugs are sold or dispensed, other than as required by law or these Regulations or with the consent of the person to whom the drugs are sold or dispensed;
(bb) providing a prescriber with prescription blanks which are imprinted with the name of a pharmacy; and
(cc) engaging in conduct, or performing an act, relevant to the practice of pharmacy that, having regard to all the circumstances, would reasonably be regarded by members as disgraceful, dishonorable or unprofessional
Fees
7.1 Council shall establish a dues and fees schedule which shall have force only after the same has been approved, with or without amendment, by majority vote at an annual or special general meeting of the College. (2016)
7.2(1) Every member shall pay the membership fees for the category of membership of the member on or before November 30 in each year, unless otherwise specifically provided
7.2(2) Every member who fails to pay the required fees by November 30 shall also pay to the College an additional late payment fee as specified in the fee schedule, by December 31 of the same year. (2016)
7.2(3) A member who has not paid the applicable fees in any year is suspended from practice on January 1st of the following year, and may be removed from the register
7.3 The manager is responsible for ensuring the annual renewal fee for the certificate of operation is paid by November 30 in each year. Every pharmacy who fails to pay the required fees by November 30 shall also pay to the College an additional late payment fee as specified in the fee schedule, by December 31 of the same year. (2016)
7.4 If any of the fees and dues owed by a pharmacy are not paid on or before December 31 of any year in which they are due,
(a) the pharmacy and the manager may be removed from the applicable register; and
(b) the certificate of operation shall be considered lapsed and the pharmacy shall cease to conduct business immediately
Part IX Registers
Active Pharmacist Direct Client Care
Active Pharmacist Non-Direct Client Care
Non-active Pharmacist
Retired Pharmacist
Active Pharmacy Technician Direct Client Care
Active Pharmacy Technician Non-Direct Client Care
Conditional Register
Non-active Pharmacy Technician
Retired Pharmacy Technician
Pharmacist Student
Pharmacy Technician Student
Retired Certified Dispenser
Life member
Emergency
Register Information
11.4 In addition to information required by the Act, all registers must contain the following information with respect to the member:
(a) the member’s name as it is given on the person’s birth certificate, subject to any change in this name supported by documentation under the Change of Name Act or through the amendment process of the Vital Statistics Act, or equivalent in the Province of New Brunswick or equivalent in another Canadian jurisdiction; (2015)
(b) the address at which the registrant ordinarily resides;
(c) date of birth;
(d) gender
(e) telephone number;
(f) email address;
(g) place of employment;
(h) a notation and date of the retirement from practice or death of a member
(i) registration number;
(j) expiry date of the annual license;
(k) the type of registration issued to the member;
(l) a notation of every voluntary surrender or cancellation of a registration, and the date of surrender or cancellation; and
(m) a notation of every reinstatement and the date of reinstatement.
Duty to Notify the Registrar of Changes to information
11.5 A registrant shall notify the Registrar of any change to information required to be on the register.
11.6 In addition to any information required by the Act, the member must also provide the following information:
(a) all verdicts and recommendations of a coroner’s inquest involving the member;
(b) denials of registration by professional regulatory colleges and denials of membership by professional associations that have regulatory responsibility
Information made available to the public
11.7 The following information contained in a register is considered to be public knowledge
(a) registration number;
(b) person’s name; (2015)
(c) the register in which the person is listed;
(d) whether the person is authorized to administer injections, assess minor ailments or provide other specialized services; (2015)
(e) whether the person is engaged in a collaborative practice agreement; (2015)
(f) results of proceedings from any Complaints Committee or a Discipline and Fitness to Practice Committee hearing where a person has been found to be at fault, for a period of two years;
(g) a notation indicating that a person’s registration has been suspended or revoked; notation remains on the register for five years; and
(h) a notation indicating that a person’s registration has been suspended or revoked for sexual misconduct; notation remains on the member’s file indefinitely, without limitation
Part XII Registration
12.1 All applicants for registration must:
(a) be of good character;
(b) complete an application in the form established by Council;
(c) pay to the College the fees provided for in the fee schedule;
(d) provide evidence that he or she:
(i) is a Canadian citizen, landed immigrant or holds a valid employment visa or valid Canadian work permit;
(ii)is a graduate of a CCAPP or ACPE accredited program, in Canada or the United States, or is authorized to practice pharmacy in another Canadian jurisdiction;
(iii) has passed any examinations or assessments that Council may require
(iv) has served a period of internship as determined by the Registration Committee;
(v) has successfully completed a structured practical training program approved by Council;
(vi) has insurance, as required by Part XXV of these Regulations;
(vii) is proficient in one of the official languages of New Brunswick;
(viii) has knowledge, to the satisfaction of the College, of the Act, Regulations, the Code of Ethics and Standards of Practice and practice directives applicable to the practice of pharmacy in New Brunswick, relevant to the members registration, and provide an undertaking that he will conform to these in practice
(ix) is currently practicing in a direct client care setting if the applicant is requesting admission to a Direct Client Care register; and
(x)meets any other requirement specified for registration in the
applied to register;
(e) disclose by declaration whether he or she
(i) is currently suspended as a result of professional misconduct, or as the result of an allegation of professional misconduct, by a PRA in Canada or elsewhere, or, if the applicant has been so convicted, provide evidence satisfactory to the Registration Committee showing effective rehabilitation
(ii)has been convicted of an offence or been subject to professional discipline which could make the applicant unsuitable for registration as a member;
(iii) is, or has been, the subject of a judicial or disciplinary decision referred to in sections 5.16 or 5.17
(iv) has dependence to alcohol, drugs or other substances;
(v) has an ongoing medical condition (including substance abuse or dependence) of which he or she is aware and knows, or ought reasonably to know, adversely affects the ability to competently and safely practice pharmacy, or which could make the applicant unsuitable for registration;
(vi) has any pending complaint or disciplinary action; or
(vii) complies with the recency of practice requirements in section 12.30; and
(f) supply:
(i) an identification photograph or electronic image issued by a government of a Canadian jurisdiction; and
(ii) a criminal record check (Canadian federal and provincial) effected within the previous six months
(iii) evidence of current First Aid and CPR certification for registration and licensure on an Active: Direct Client Care register.(2021)
Conditional Registers
12.5(1) The following registrants may be entered on a conditional register
(a) Current members with conditions imposed by the College;
(b) International pharmacy graduates (pharmacists and pharmacy technicians);
(c) Registrants pursuing postgraduate training in a formal educational program;
(d) Registrants pursuing a training program not associated with an educational institution;
(e) Members who have conditions resulting from Complaints or Discipline and Fitness to Practice proceedings. (2022
Rights of Conditional Registration
12.7 Where a person is entered on the conditional register, he or she may:
(a) conduct the practice of pharmacy only in accordance with any conditions imposed; and
b) except as set out in section 12.8, exercise all the other rights and privileges of a member
Pharmacy Technician Students
12.19(1) A pharmacy technician student shall register with the New Brunswick College of Pharmacists as a "registered pharmacy technician student" prior to the commencement of any employment and shall not hold themselves out to be other than a registered pharmacy technician student. Pharmacy technician students shall not hold themselves out to be pharmacy technicians/assistants. (2015)
12.19(2) Pharmacy technician students may only provide pharmacy services while under the supervision of an authorized preceptor
12.19(3) Pharmacy technician students must complete a minimum of 14 weeks of practical training, under the supervision of a preceptor, consisting of:
(a) a minimum of eight weeks in a structured practice experience program similar to that for pharmacists as defined in “A Framework for Assessing Canadian Pharmacists’ Competencies at Entry-to Practice through Structured Practical Training Programs” as published by NAPRA, in a direct client care setting in a community pharmacy or hospital pharmacy, or other location approved by Council
(b) a minimum of 6 weeks, which shall be completed in New Brunswick after graduation; and
(c) successful completion of a Structured Practical Evaluation (SPE) as part of the 6 week post-graduate training period, one component of which requires the pharmacy technician student to accurately apply an independent double check to 500 prescription/ orders/ products for final release with 100% accuracy, an activity which allows for a maximum of 50 items per day. (2016)
12.19(4) During a period of internship, a Pharmacy Technician Student must be assigned to a preceptor, who, as the Pharmacy Technician Student’s preceptor, shall ensure that the Pharmacy Technician Student is exposed to areas of the practice of pharmacy relevant to the internship, including:
(a) maintenance of the client medication profile, evaluation of therapy (for example: duplication, adherence), evaluation of new prescriptions, and resolution of potential and existing problems
(b) accurate dispensing of medication according to the prescription;
(c) assistance to the client on the use of medical devices;
(d) communication with clients and/or health professionals regarding drug and health information;
(e) compliance with all legal requirements associated with the distribution of drugs and the operation of a pharmacy;
(f) provision of information and/or referral services in emergencies, and upon request
(g) development and exercise of appropriate professional judgment;
(h) knowledge of, and compliance with, ethical and professional Standards of Practice;
(i) any other areas established by Council. (2015)
Pharmacy technician students becoming pharmacy technicians
12.20 A pharmacy technician student may apply to be a registered pharmacy technician provided all the requirements in section 12.1 and the requirements provided in section 12.19 are met. An educational program having provisional CCAPP or ACPE accreditation in Canada or the United States will be considered to be accredited for the purposes of this section. Pharmacy Technician Students qualifying under Section 12.3 may apply meeting the requirements of Section 12.1 with the exception of subparagraph 12.1(d)(ii), and meeting all requirements of Sections 12.19 and 12.3. (2015) (2019)
Time Limits
12.21 A person applying for registration and licensure who has graduated from an accredited pharmacy program must be registered and licensed with the College within three years of completing the program and within three years of successfully completing PEBC examinations. (2020)
Apprenticeship Agreement
12.22(1) Every person before commencing training with a preceptor shall:
(a) be registered with the College either as a conditional registrant or a student;
(b) enter into an apprenticeship agreement in the form established by Council; and
(c) forward the signed agreement to the College and receive confirmation from the College that the preceptor meets all requirements provided in subsection 12.23(1). (2021)
Preceptor Qualifications
12.23(1) A member, in order to serve as a preceptor, must meet the following requirements:
(a) be a member who practices in New Brunswick for at least 18 hours a week; (average a year)
(b) have been licensed and practicing in New Brunswick for at least one year;
(c) meet the training requirements of the College by either completing a preceptor training program approved by the College, or meeting the requirements to be a preceptor for the structured practical experiential program (SPEP) in the curriculum of an accredited pharmacy education program;
(d) practice in a pharmacy that meets the SPEP Practice Site Criteria established by the educational institution, or at a location approved by Council;
(e) confirm that the apprentice is properly registered with the College
(f) ensure that any apprentice engaged in practice experience has the level of personal supervision or direction that, in the professional judgment of the preceptor, is required to ensure safe and effective client care given the knowledge, skills and experience of the apprentice; and
(g) not have or be perceived by the College to have a conflict of interest or bias with respect to the apprentice they are supervising. (2021)
A preceptor may not:
(a) have any terms, conditions or limitations on his/her certificate of registration and license other than those applicable to all members of that register unless otherwise authorized by the Registration Committee;
(b) have been found to have committed an act of professional misconduct or to be incompetent by the Discipline and Fitness to Practice Committee within the last six years;
(c) have been found to be incapacitated by the Complaints Committee within the last six years
(d) have been the subject of allegations of professional misconduct or incompetence that have been referred to, but not yet decided upon by, the Complaints Committee, or the Discipline and Fitness to Practice Committee
Duration of Registration of Students
12.24(1) The registration of a student (pharmacist and pharmacy technician) shall be revoked by the Registrar if:
(a) the student is registered on another register;
(b) prior to graduation the student ceases to be enrolled in their pharmacy education program; (2015)
(c) the registration is cancelled under Part X of the Act;
(d) the student has otherwise failed to comply with the provisions of the Act or the Regulations
12.24(2) Where a student’s registration is revoked, the student must obtain the permission of Council before reapplying for registration. Council, on application to it by the student, may at its discretion order that the registration of the student be re-instated.
12.24(3) The registration of a student (pharmacist and pharmacy technician) who does not become a member expires one year from the date of graduation, unless an extension is granted by the Registration Committee. (2016; 2017)
Application not Approved
12.29 If an application for registration or conditional registration is not approved, or approved subject to conditions, the applicant must be notified in writing, with reasons for the decision, and advised of the right to appeal the decision to Council.
Change of Workplace or Practice
12.31 A member who changes place of employment for more than 30 consecutive days shall notify the College by updating their member profile within seven days of the change
Pharmacies
Pharmacies are required to register as either community or institutional.
In the registration the pharmacy needs to include:
Name of the pharmacy,
Name(s) of the person(s) who conduct business,
Name of the manager who holds the certificate of operation
Address, telephone number and fax number of the pharmacy
Email addresses of manager and the pharmacy
Certificate of operation number
Initial date and end date of registration and operation
Pharmacy related website address(s)
Owner’s name, phone number and email address
Certificate of Operation
Before a pharmacy can operate it must apply for a certificate of operation at least 30 days prior to operation.
In order to receive a certificate of operation, the pharmacy must provide to the registrar
A completed application form
Demonstrate that the pharmacy will be staffed and managed by members capable of operating a pharmacy
Operate a sufficient number of hours per week to meet the needs of the community
Have internet access for email and research purposes
Be connected to and share information with DIS/PMP
Have a quality management process in place
Meet all requirements related to the practice of pharmacy as described in the application, established by Council in policy or practice directive
Restriction on Operation
N.B.: Council has yet to declare into force section 13.6
13.6(1) A pharmacy may be granted a certificate of operation as offering a specialized type of service.
13.6(2) The pharmacy’s practice is then restricted to the type(s) of service stated on the certificate.
13.6(3) Nothing prevents a pharmacist in a specialized pharmacy from providing care where there is an urgent situation and it is required to meet the needs of clients
Certificates of Operation
N.B.: Council has yet to declare into force section 13.7
13.7 The following categories of certificates of operation are established:
General
Central fill
Mail order
Clinical practice
Satellite pharmacy
Methadone
Specialty compounding
Pharmacy education facility
Correctional service
Nursing home
Hospital
Natural Health/Alternative Care and
Limited service, other
Pharmacy Standards of Operation
Pharmacies that provide direct client care service to the public
are required to:Be accessible to the public in person and by telephone,
Designed to discourage entrance to the dispensary area by unauthorized persons but still encourage and facilitate discussion between client and pharmacist
equipped with a private consultation area where clients may be counselled and their treatment discussed without being overheard by the public, or other staff. (2022)
Quality Management
14.2 The manager must ensure and document ongoing quality management including, but not limited to: evaluating staff performance, equipment and facilities and adherence to Standards of Practice including the following
(a) as of January 1, 2019, anonymous medication error reporting to an external Canadian database for errors that reach patients;
(b) response to individual errors and trends
(c) maintenance of a culture of safety within the practice
(d) provisions to protect the confidentiality of information relating
to clients. (2018) Quality Management
Information to be posted in Pharmacy
The following items are to be displayed in or near the dispensary where clients can view:
Certificate of Operation
Certificate of Registration and annual license of pharmacists, pharmacy technician and any students
Hours of operation
A condensed version of the Code of Ethics; (2022)
Any other information required by Council to be made available for the purpose of informing the public about the practice of pharmacy
Presence of Pharmacist
14.16(1) When the dispensary and the professional service area are open and accessible to the public and Schedule III drugs are displayed, a pharmacist shall be present in the pharmacy. (2022)
After hours, staff may be present in the dispensary to perform limited tasks such as inventory control, generating prescription labels, replenishing drug stock, 3rd party billing etc. No activities that require the presence of a pharmacist may be performed
Security
Every member while on duty is responsible for the security of the pharmacy. The member should protect against unauthorized entry, theft or diversion of medication.
After hours, the pharmacy should be secured with suitable security measures such as locks, alarms, cameras to prevent and detect unauthorized entry
Prescription Dispensing and Records
A prescription may be filled or refilled up to one year from the date issued unless cancelled by the prescriber.
No person except a member within their scope of practice, shall:
Sell a scheduled drug
Prepare written copies of a prescription
Provide or receive verbal copies of a prescription
Assess and approve a prescription for filling or refilling
Receive and record a verbal prescription from a prescriber
Educate a client about a drug and their drug therapy
Adjusting Quantity
A member may in consultation with a client adjust the quantity of the drug to be dispensed when:
The client request a different quantity and its appropriate to do so,
The manufacturers standard package size does not match the prescribed quantity, (boxes do not have to be opened)
The quantity exceeds the amount covered by the client’s drug plan,
A trial quantity is authorized by the client,
The member consults with the prescriber and documents the consultation,
Poor compliance history,
Drug misuse suspected,
The safety of the client is in question due to potential for drug overdose
35 Day Supply Regulation
17.5(2) Subject to subsection 17.5(4), a pharmacist shall dispense no more than a thirty-five day supply of narcotics, controlled drugs or benzodiazepines to any client. (2022)
Subsection 17.5(2)(a) does not apply to drugs indicated for and being used for the prevention and/or treatment of seizure disorders. (2015)
17.5(4) A pharmacist may dispense more than a thirty-five-day supply
of medication provided that:17.5(4) (a) in the member’s professional judgement it is safe to do so; and
(b) the prescriber has specified the exact quantity to be dispensed in excess of the thirty-five-day limit and has stated a reason for ordering that
quantity. (2022)
35 Doses: Where the signa on a prescription does not clearly define the days supply, the pharmacist or certified dispenser shall dispense no more than thirty-five doses
Substitution
When a prescription either written or verbal contains a direction by the prescriber that the prescribed brand of drug is not to be substituted the person dispensing the drug shall not make a substitution unless requested by the client.
Any substitutions must be recorded and forms part of the prescription record
Child Resistant Containers
Any one who fills a prescription in an oral dosage form is required to dispense the drug in a child resistant container.
A child resistant container does not have to be used when:
A client, their prescriber or a responsible agent directs otherwise,
Medications are dispensed in the manufacturers original packaging,
Medications are dispensed in devices or aids to improve compliance,
Medications are being delivered to clients in hospital or nursing home.
If a child resistant container is not being used at the time of filling then a note should be made on the client’s record indicating this.
**Light resistant
Obligations Before Dispensing
17.10 Members must: (a) ensure that a prescription is authentic; (b) refuse to dispense the drug if the member doubts the authenticity of a prescription; (c) review prescriptions for completeness and appropriateness with respect to the drug, dosage, route and frequency of administration; (d) review client personal health for potential drug interactions, allergies, therapeutic duplications and any other drug related issues; (e) consult with clients concerning the client’s drug history and other personal health information (f) consult with the client’s prescriber with respect to the client’s drug therapy where warranted; and (g) follow-up on suspected adverse drug reactions, or other drug related issues
IF the doctors name is illegible write their family doctor and make note
Medication Labels
The label must include:
The drug name and strength,
The name, address and telephone number of the pharmacy,
The prescription number, dispensing date and name of prescriber,
The full name of the client,
The prescriber’s direction for use,
The quantity dispensed,
The DIN, Natural Product Number or Homeopathic Medicine Number as
well as manufacturer’s name or abbreviation,Any other information required to ensure the client takes/uses the
medication appropriately
if the prescription is for a single-entity product, the label must include:
(a) the generic name, strength and the manufacturer’s name,
together on one line(b) if any other drug name, e.g. brand name, is also used, it must be
on a separate line on the label.
17.14(3) In reference to subsection 17.14(1), if the prescription is for a multiple-entity product, the label must include:
(a) the brand name; or
(b) all active ingredients and quantity/strength, and at least one of:
(i) the manufacturer’s name, or
(ii)the drug identification number
If the prescription is for a compounded preparation, the label must include the strength and name of each active ingredient.
Medications dispensed in Compliance aids
Medications dispensed to clients to improve compliance shall conform to the guidance approved by Council with regard to packaging, labelling and storage requirements
Obligations Following Dispensing
Prior to delivering a prescription to the client, the pharmacist has an obligation to ensure the client is counselled in accordance with Standards of Practice and the counselling is
documented in the client’s profile
Client Profile
Minimum information Required
Client’s name
Address
Phone number
Gender
Date of Birth
Any client identification number required for DIS/PMP
Medical conditions and physical limitations
Allergies and drug reactions
Reference to the prescription number for each prescription filled
Documentation on any info collected by the pharmacist relating to med history or info
If the client requests not to use client resistant containers
A client profile is considered property of the pharmacy in which it is prepare
Prescription Verification
The prescription record is to include:
The signature or initials of the person authorizing the prescription to be filled,
The signature or initials of the person preparing the drug for dispensing,
The signature or initials of the person doing the final check,
The signature or initials of the person counselling the client
Prescription Records
The prescription record includes all information recorded in written and electronic format that is pertinent to the prescription being dispensed.
In addition to prescription information, information on a client’s use of Schedule II and Schedule III drugs may also be recorded if its relevant to managing a client’s medication use
Retention of Records
A pharmacy is retain records for a period of two years in written format and electronically for not less than 15 years.
Storage in electronic format means the full original prescription, front and back if applicable and viewable.
The records do not need to be stored in the pharmacy as long as the records are securely stored at a physical location within Canada and are retrievable within a reasonable time.
Records stored electronically need to be encrypted or encoded and access restricted to only authorized personnel
Release of Information
No information contained on a prescription or Client profile should be released to any person without consent of the client.
Information can be released to
Government or agency providing benefits to the client,
Another health care professional,
A police officer on presentation of a search warrant,
Authorized inspectors of Health Canada or NBCP,
A police officer when a forgery, fraud, polypharmacy or double doctoring is suspected or known
Pursuant to the Prescription Monitoring Act
Transfers
A prescription can be transferred in or out of a pharmacy if:
The drug doesn’t contain a controlled drug or narcotic except as
authorized under the CDSAPharmacies providing or receiving the transfer are registered in any
province or territory of Canada.
A prescription can be transferred either verbally or electronically.
When a transfer is made the following info is recorded:
Date of the transfer and name of pharmacist authorizing transfer,
The name of the pharmacist and pharmacy requesting the transfer,
After transfer all remaining refills are cancelled.
The pharmacist, or pharmacy technician who receives the transfer must ensure the authenticity of the person transferring the prescription verbally or electronically and must enter on the transferred prescription record the name of the client, the original prescription date, the date the prescription was last filled by the transferring pharmacy, the initials of the pharmacist who authorized the transfer.
Return to Stock
Any drug or preparation previously delivered to a client cannot be accepted for return to stock.
A drug can be returned for a dosage adjustment or reuse by the same client; or for destruction
Expired Drugs
Expired drugs can not be sold in a pharmacy.
Drugs are considered expired when:
the expiration date has passed,
Its unlikely the drug would be fully consumed before the expiration date
Code of Advertising
Advertising for Pharmacy
Must not be false or misleading
Encourage the misuse or inappropriate use of drugs,
Undermine the integrity of the profession,
Doesn’t make comparisons between pharmacies or pharmacists
Must be verifiable,
Contains no testimonials
Cannot contain information on fee, markup or price
contains no reference to a member’s specialty unless the member is a specialist in a specialty recognized by the College;
contains no information in respect to a fee, markup or price other than descriptive information in respect to a pharmacy’s full retail price for a prescribed medication, which descriptive information must include generic or trade name, manufacturer, strength and quantity.
does not offer any incentive in relation to a prescription drug product or pharmacy services;
does not encourage the transfer of prescriptions by offering the receipt of an incentive associated with filling prescriptions or receiving pharmacy services
Prescribing by Pharmacists
Only pharmacists who have completed the requirements by Council can prescribe.
Types of prescribing
Adapting a prescription,
Altering dose, formulation or regimen,
Renewing a prescription for continuity of care,
Continuing therapy without a prescription for a previously diagnosed condition,
Therapeutic substitution,
Prescribing non-prescription drugs, treatments and devices,
Prescribing in an emergency,
Collaborative practice,
Prescribing for minor ailments
A pharmacist may only prescribe a drug, treatment or device if:
the indication and treatment is within the pharmacist’s scope of practice, knowledge, skills, competencies and experience;
the pharmacist has:
performed an assessment in an environment that is appropriate,
determined treatment is indicated,
discussed treatment options with the client, and
prescribed the most appropriate treatment based on the assessment; and
the drug is appropriate to treat the client’s condition.
a pharmacist shall not prescribe a drug unless the pharmacist has obtained sufficient information by reviewing the client’s medication history and discussing treatment options with the client or, if necessary, and with the client’s consent, obtains pertinent information about the client’s care and treatment from family, friends, or caregivers.
there is an established pharmacist-client relationship
prescription decision of the pharmacist has been consented to by the client, or by the client’s parent or legal guardian,
the pharmacist has successfully completed any training requirements determined by Council, and has available any required reference resources
shall assess the client in person at the time of prescribing.
the pharmacist has seen the client personally in the past and has an established professional relationship with the client;
the pharmacist has sufficient knowledge of the client’s condition and current clinical status relevant to the prescribing decision; and
the pharmacist communicates with the client or their agent at the time of prescribing
the pharmacist has assessed the client in compliance with the Code of Ethics and Standards of Practice and any applicable practice directives;
the drug is prescribed in a circumstance which is within the pharmacist’s area of practice, knowledge and skills, or specialty;
the pharmacist has determined that a prescription is reasonably necessary to treat the client; and
the pharmacist has discussed with the client, or their agent, reasonable and available therapeutic options.
If the pharmacist identifies that the condition being assessed is outside his or her scope of practice, the pharmacist shall refer the client to an appropriate health care practitioner, and shall record the assessment and the referral in the client’s profile
a follow-up plan that is sufficiently detailed to monitor the client’s progress and ensure continuity of care by the pharmacist,
or other regulated health professionals or caregivers, if applicable; and
any other advice or treatment recommended to the client.
The pharmacist, when prescribing a drug, treatment or device, will notify the client’s primary care provider (when such exists) when the order the pharmacist is prescribing is clinically significant.
Prescribing for Minor Ailments
A pharmacist is authorized to prescribe a drug, treatment or device that is in Schedule I, Schedule II or Schedule III or is an unscheduled drug for the treatment of a condition, if the drug, treatment or device is indicated for treatment of a minor ailment
Appendix 2: List of Minor Ailments
Allergic Rhinitis
Calluses and Corns
Contact Allergic Dermatitis
Dandruff
Dysmenorrhea
Dyspepsia
Emergency Contraception
Fungal Infections of the Skin
Gastro-esophageal
Reflux Disease
Hemorrhoids
Herpes Simplex
Impetigo
Mild Acne
Mild Headache
Mild to Moderate Eczema
Mild Urticaria (including bites and stings)
Minor Joint Pain
Minor Muscle Pain
Minor Sleep Disorders
Nasal Congestion
Nausea
Nicotine dependence
Non-infectious Diarrhea
Oral Fungal Infection (thrush)
Oral Ulcer
Threadworms and Pinworms
Upper respiratory tract conditions (cough, nasal congestion and
discharge, sore throat, fever, headache, malaise)Urinary Tract Infection (uncomplicated)
Vaginal Candidiasis
Warts (excluding facial and genital)
Xerophthalmia (dry eyes)
Contraception Management
Paxlovid
Herpes Zoster (Shingles)
Prescribing for Preventable
Diseases
Subject to Sections 2 & 3, pharmacists may prescribe and administer Schedule
I, Schedule II, Schedule III and Unscheduled vaccines (individual or combination
products) and/or drug products for the prevention of the following diseases:Cholera (pharmacist may prescribe only the oral, inactivated vaccine)
Diphtheria
Haemophiles influenzae type B
Hepatitis A
Hepatitis B
Herpes zoster (shingles)
Human Papillomavirus (HPV)
Malaria
Measles
Meningococcal disease
Mumps
Pertussis
Pneumococcal Disease
Polio
Rubella
Seasonal Influenza
Tetanus
Traveler’s Diarrhea (pharmacist may also prescribe pre-emptive treatment)
Varicella zoster (chickenpox)
Pharmacists may ADMINISTER injectable vaccines for the following diseases but they may NOT PRESCRIBE injectable vaccines for the following diseases unless they have successfully completed a training program in travel medicine approved by Council. (These are usually required for international travel.)
Cholera (other than the oral, inactivated vaccine)
European tick-borne encephalitis
Japanese encephalitis
Rabies
Typhoid
Yellow fever
Criteria for Prescribing
the pharmacist has made an assessment to determine whether the drug will be safe and effective in the circumstances of the client, including, but not limited to the following:
the client’s symptoms,
co-existent disease states and chronic conditions,
the client’s allergies and other contraindications and precautions,
other medications the client may be taking,
the client’s gender, age, weight and height (where applicable),
pregnancy and lactation status, if applicable, and
any other inquiries reasonably necessary in the circumstances
Prescribing Restrictions
A pharmacist may not prescribe
for themselves;
for any person with whom there is a close personal or emotional relationship; or (friends/family)
in contravention of federal legislation, including the Narcotic Control Act and its Regulations, the Controlled Drugs and Substances Act and its Regulations or any successor act or regulation
Recording of Prescribing
must make and retain a record of all information necessary for prescriptions PLUS:
the circumstances under which the drug was prescribed;
the rationale for prescribing – diagnosis, treatment plan, clinical indication, or expected outcome;
a summary of the pharmacist’s assessment of the client;
the name, address, and telephone number of the pharmacist issuing the prescription;
pharmacist’s signature and registration number
Part XXII- Administration of Drugs
have successfully completed an educational training program approved by Council;
have policies and procedures in place for administering drugs and dealing with emergencies;
ensure that the environment in which the drug is to be administered is appropriate;
have proper regard for the interests of the client and take all steps necessary to ensure that the drug is administered safely; and
have successfully completed any other requirements specified by Council.
Administration of Drugs
Routes of Administration are:
Orally including sublingual and buccal,
Topically including ophthalmic, Otic and intranasal,
Via inhalation.
A pharmacist who meets requirements of the Administration of Injections
Policy may administer a drug, biological or blood product:Through intra-dermal injection,
Through subcutaneous injection,
Through intramuscular injection or
Intravenously through an established central or peripheral venous access device
Pharmacists may only administer an injectable vaccine to a client who is 5 years of age or older, and only after having successfully completed an injection administration training program approved by Council. (2016)
Record of Drug Administration
must make and retain a record in the pharmacy of:
the name and address of the client;
the name of the drug and total dose administered;
the route, and site, of administration;
the lot number and expiry date of the product administered;
the name of the pharmacist administering the drug;
the date and the time of the administration;
any client counselling provided; and
any adverse events and their management
Part XXIII- Tests
A pharmacist may interpret the results of any clinical test performed by the client, and may give advice to the client regarding the results and implications of those tests.
A pharmacist may administer the clinical tests approved by Council, interpret their results and give advice to the client regarding the results and implications of those tests
Test Interpretation Record
A pharmacist who interprets and makes a recommendation to a client regarding a clinical test must make and retain a record in the pharmacy of:
the name and address of the client;
the nature of the test interpreted;
the date of the test;
the results of the test; the nature of the advice given to the client; and
the pharmacist’s name
Ordering Tests
A pharmacist may administer a test, or order, and receive the results of, a
laboratory screening or diagnostic test when deemed appropriate and
necessary for the care of the client.If test results reveals medical issues requiring attention; or that, the pharmacist is not able to interpret, must
promptly forward the results to any other health professional responsible for the client’s care for the interpretation of the results;
discuss the interpretation and course of action to be followed with the health professional when required;
recommend a course of treatment, if appropriate.
The pharmacist and the other health professional will determine which will advise the client of the test results
Test Ordering and Results Record
A pharmacist who administers a test, or orders and receives the results of a screening or diagnostic test must make and retain a record in the pharmacy of:
the name and address of the client;
the nature of the test administered or ordered;
the name of any health professional to whom the results were forwarded, or a recommendation was made;
the name of the pharmacist requesting the test;
the date the test was ordered;
the date the results were received; the date the results were communicated by the pharmacist to the client, if the pharmacist is able to interpret the results, and other health professionals responsible for the client’s care
Professional Development
Members are to maintain a portfolio documenting ongoing learning activities, as a condition of maintaining membership with the college.
Members may be requested to submit or present in person their portfolio to the college upon request for audit, review and discussion
Insurance
Pharmacy technicians need liability insurance that provides a minimum of $1,000,000 per claim or occurrence and a minimum of $2,000,000 annual aggregate.
Proof of personal professional liability insurance shall be provided to the Registrar upon registration and annually at the time of license renewal, or when requested
NBCP-Pharmacy Act https://nbppharmacists.ca/wp-content/uploads/2020/12/New-Act-with-Table-of-Contents.pdf?x43718
Definitions
administer = the direct application of a drug, or treatment, to the body of a client by ingestion, application, inhalation, injection, or any other =. (administrer)
Administrator= the Administrator of Complaints appointed by Council to carry out the responsibilities set out in Part X. (administrateur)
applicant= a person applying for admission to membership in the College or reinstatement in the College. (postulant)
certificate of operation= a certificate of any category authorizing the operation of a pharmacy, and issued to a manager. (certificate d’exploitation)
Certified dispenser: a person whose name is entered on a register of Certified dispensers. (dispensateur agréé)
Code of Ethics= the Code of Ethics adopted by the College, as amended from time to time. (Code de déontologie)
compound: to prepare components into a drug product, including the preparing of drugs or devices in anticipation of receiving prescriptions based on routine, regularly observed prescribing patterns. (composition)
conduct includes an act or omission. (conduite)
Council= the Council of the College. (Conseil)
Court = the Court of Queen's Bench of New Brunswick. (Cour)
day= a calendar day. (jour)
dispensing = the interpretation and clarification of a prescribers order and the assembly and preparation of the order for delivery to the client. (exécuter une ordonnance ou dispenser)
document includes:
(a) any record containing information whether in legible, visible or audible form, or stored electronically,
(b) files, papers, books, accounting records, banking records, prescriptions, photographs, plans, charts, prints, drawings, films, tapes, video cassettes, diskettes, word processing software and other machine readable records regardless of physical form or characteristics, and
(c) any part of a document. (document)
“Drug”: includes any substance or mixture of substances manufactured, compounded, sold or represented for use in:
(a) the diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals, or
(b) restoring, correcting or modifying organic functions in human beings or animals. (médicament)
employee: a person directly or indirectly providing services to an employer, whether as an independent contractor or employee, and regardless of whether such services are provided on a full-time, part-time or casual basis. (employé)
health professional = a person who provides a service related to:
(a) the preservation or improvement of the health of individuals, or
(b) the diagnosis, treatment or care of
individuals who are injured, sick, disabled or infirm,
and who is regulated under a private Act of a Canadian legislature, or Parliament, with respect to the provision of the service, and includes a social worker registered under the New Brunswick Association of Social Workers Act, 1988. (professionnel de la santé)
inspector = a person appointed by Council or the Registrar, or the Registrar himself or herself, to investigate, audit or inspect matters related to the practice of pharmacy. (inspecteur)
intern = a person whose name is entered in the register of interns. (stagiaire)
internship = a period of practical training under the supervision of a preceptor approved by Council. (stage)
lay representative: a person who is appointed as a public representative under this Act. (représentant du public)
limited access drug = a drug which shall not be sold:
(a) without a prescription, or
(b) without the supervision or intervention
of a member in accordance with this Act and the Schedules established pursuant to section 27. (médicament à accès limité)
manager = the member designated to have authority over and be responsible for the operation of the pharmacy. (gérant)
member = a member of the College as defined in Part VIII. (membre)
Minister = the Minister of Health for New Brunswick, or his or her successor. (ministre)
"person" includes an individual, a partnership, a corporation and any other organization or entity. (personne)
pharmaceutical alternative: is a drug product that contains the same therapeutic moiety, but different salts, esters, or complexes of that moiety, or is a different dosage form or strength. (substitut pharmaceutique)
pharmaceutically equivalent: a drug product that, in comparison with another
drug, contains identical amounts of the identical medicinal ingredients, in comparable dosage forms, but that does not necessarily contain the same non-medicinal ingredients. (équivalent pharmaceutique)pharmacist= a person whose name is entered on a register of pharmacists. (pharmacien)
pharmacy:
(a) the location where distributive, cognitive or consultative services are provided to the general public relating to drugs, medicines, compounding, dispensing prescriptions and/or health, and
(b) other locations as defined in the regulations. (pharmacie)
pharmacy residency is an organized, directed, accredited program that builds upon knowledge, skills, attitudes, and abilities gained from an accredited professional pharmacy degree program, with the purpose of enhancing general competencies in managing medication- use systems and supporting optimal medication therapy outcomes for clients with a broad range of disease states. (résidence en pharmacie )
pharmacy technician: a person whose name is entered on a register of technicians. (technicien en pharmacie)
pharmacy technician student= a person whose name is entered on a register of pharmacy technician students. (étudiant en technique pharmaceutique)
“PEBC” = the Pharmacy Examining Board of Canada. (BEPC)
“Pharmacist – Direct Client Care” = a pharmacist in active practice that had direct contact with clients for at least 400 hours during the preceding two-year period. (pharmacien – ASSISTANCE DIRECTE AUX CLIENTS)
“Pharmacy technician – Direct Client Care” = a pharmacy technician in active practice, under the supervision of a Pharmacist – Direct Client Care, for at least 400 hours during the preceding two-year period. (technicien en pharmacie – ASSISTANCE DIRECTE AUX CLIENTS)
“Pharmacy technician – Non-Direct Client Care” = a pharmacy technician in active practice who does not meet the criteria of a Pharmacy technician – Direct Client Care (e.g. pharmacy technicians in administrative, management or other non-direct care positions). (technicien en pharmacie – SANS ASSISTANCE DIRECTE AUX CLIENTS)
practice directive = a written statement made by Council for the purpose of giving practice direction to the members. (directive professionnelle)
preceptor = a person who meets the qualifications prescribed in the regulations (précepteur)
prescriber = a legally qualified health professional or a veterinarian, authorized to prescribe drugs or devices in any Canadian jurisdiction, and who gives a prescription. (prescripteur)
prescription = a direction given by a prescriber directing that a drug, device, or treatment specified in the direction be dispensed for the person named, or animal described, in the direction. (ordonnance ou prescription)
record includes documents as well as information described in the regulations, but does not include electronic software or any mechanism that produces records. (dossier)
regional health authority or RHA = a regional health authority established under the Regional Health Authorities Act, or as defined by the Minister. (régie régionale de la santé)
register = a register established under Part IX. (registre)
Registrar= the Registrar of the College appointed under section 13. (registraire)
record = the records of a pharmacy, whether in written, photographic, magnetic, electronic or other form, and includes, without limitation,
(a) the records of the proprietor of the pharmacy, the manager, the regulated members engaged by the proprietor or any other person associated with the pharmacy;
(b) any record required to be kept under the Act, the Controlled Drugs and Substances Act (Canada) or the Food and Drugs Act (Canada) or the regulations or standards under those acts;
(c) a record of all prescriptions the pharmacy receives, including an identification of the prescriptions that the pharmacy transfers to another pharmacy or pharmacist
d) a record of all drugs dispensed from or through the pharmacy, including the prescription, the name of the drug, the amount dispensed, the name and contact information of the client and the name and contact information of the prescriber;
(e) a record of the pharmacy services provided, including the name of the person or persons who dispensed a drug, or provided a pharmacy service;
(f) a record of the names and contact information of the clients to whom pharmacy services are provided; and
(g) a record of the counselling services provided to a client. (dossier)
regulations= the regulations of the College made under Part VI, and includes
the Code of Ethics. (règlement)restriction= a limitation placed on privileges to practice. (restriction)
retailer= a person who sells consumer goods to the public within the Province of New Brunswick and does not operate a pharmacy under the authority of a certificate of operation issued under this Act. (détaillant)
sell= to sell, advertise for sale, offer for sale, offer to arrange for another person to sell, expose for sale, have in possession for sale, or distribute, whether or not the distribution is made for consideration. (vendre)
standards of practice = the standards regarding the practice of members and the operation of pharmacies established in the regulations. (norme d’exercice)
supervision is a process in which two or more persons (one of whom is the person being supervised) participate in a joint effort to promote, establish, maintain and evaluate a level of performance, at levels defined in the regulations. (encadrement)
suspension = loss of privileges for a specified period of time. (suspension)
therapeutic equivalent: a drug product that can be expected to have the same clinical effect and safety profile as another drug. (équivalent thérapeutique)
wholesaler = a person who sells or distributes drugs and devices mainly for resale or business use, but excludes a manufacturer. (grossiste)
Part III: Objects and Duties of the College
(a) promote and protect the health and well-being of the public, in collaboration with other health disciplines, through regulation and development of the pharmacy profession;
(b) require that for the safety of the public, all persons engaged in the practice of pharmacy within the Province are acquainted with the processes of the profession and possess a competent practical knowledge of pharmacy;
(c) require that the profession of pharmacy is practised by its members in accordance with standards set by the College;
(d) regulate the practice of pharmacy and govern its members;
(e) maintain and develop standards of practice for members;
(f) establish, maintain and develop standards of professional ethics for its members;
(g) administer this Act and perform such other duties and exercise such other powers as are imposed or conferred on the College by or under any Act;
(h) uphold and protect the public interest in the practice of pharmacy;
(i) hold forth the independence, integrity and honour of the profession;
(j) establish and maintain standards for the education, knowledge, qualifications,
professional responsibility and competence of its members and applicants; and(k) ensure the safe, rational and effective use of drugs and devices, and support members in the continued improvement of pharmacy services to the public.
Part IV: Council
6(1) The College shall be governed by a Council consisting of Councilors who shall be:
(a) members of the College elected pursuant to section 7, being not fewer than six and not more than twenty-four;
(b) lay representatives appointed pursuant to section 8; and
(c) other persons, in the number and manner provided for in the regulations.
6(2) Council shall exercise all the powers and functions of the College
Part V: Powers of Council
Committees
(12) Council shall establish and appoint as here provided the following
committees:(a) the Complaints Committee,
(b) the Discipline and Fitness to Practice Committee,
(c) other committees deemed necessary by Council.
Regulations respecting pharmacy technician
16(1) As regards to pharmacy technicians, Council shall make regulations that establish
(a) criteria and conditions under which pharmacy technicians are permitted to practice pharmacy, subject to subsection 49(3);
16(2) Council shall make regulations imposing on persons desiring to become pharmacy technicians:
(a) the educational requirements to be met;
(b) a period of internship for a set time period; and
(c) other conditions to be met.
Part VI: Regulations of the College
Regulations respecting pharmacy technicians
16(1) As regards to pharmacy technicians, Council shall make regulations that establish
(a) criteria and conditions under which pharmacy technicians are permitted to practise pharmacy, subject to subsection 49(3);
16(2) Council shall make regulations imposing on persons desiring to become pharmacy
technicians:(a) the educational requirements to be met;
(b) a period of internship for a set time period; and
(c) other conditions to be met.
Coming into effect of regulations
22(1) A new regulation, or the amendment or repeal of a regulation, is not effective unless
(a) a majority of Councilors then in office vote in favour of it; and
(b) it has been approved, with or without amendment, by majority vote at an annual or special meeting of the College, and subject to subsection (2), it comes into force upon approval by the members or at such later date as provided in the regulation.
…the member obtained pursuant to the regulations, and the Minister obtained pursuant to subsection (3), Council may make, amend or repeal regulations relating to matters respecting
(a) Composition of Council and eligibility for Council membership;
(b) admission of members;
(c) setting or expanding the scope of practice for members;
(d) the adoption or deletion, in whole or in part, of any nationally accepted schedule or formulary adopted by reference as a Drug Schedule;
(e) the prescribing or
(f) members' authority to delegate duties;
(g) criteria for the eligibility to be entered in any of the practice registers, including recognition of educational credentials; and
(h) ordering of diagnostic tests
22(3) Upon receiving a written request from the College to make, amend or repeal a
regulation pursuant to subsection (2), the Minister shall, within thirty days, in writing,
either:(a) approve the request;
(b) reject the request with reason; or
(c) extend the time for his or her decision for a period not to exceed a further sixty days.
22(4) If no written response is received from the Minister at the end of the original or extended period provided for in subsection (3), the Minister shall be deemed to have accepted the proposed
Part VII: Meetings
28 An annual general meeting of the members of the College shall be held each year at a time and place designated by Council, convened in accordance with the regulations.
Special General Meeting
31 Council may at any time. convene a special general meeting of the College as provided in…
Part IX: Right to Practice
Interim suspension by registrar
42(1) If the Registrar believes that a matter exists relating to a member's practice that presents or is likely to present a serious risk to the public, the Registrar may:
(a) direct the member to rectify the matter;
(b) suspend the member's licence, pending a review of the matter by the Complaints Committee or the Discipline and Fitness to Practise Committee.
42(2) Failure to rectify the matter contrary to paragraph (1)(a) may constitute professional misconduct.
Referral of Complaints
42(3) Upon suspending a license under paragraph (l)(b), the Registrar shall refer the matter to the Complaints Committee or to the Discipline and Fitness to Practise Committee.
42(4) A panel of the committee shall hold a hearing into the interim suspension within ten days.
Practice of Pharmacy
49(1) The practice of pharmacy promotes health, the prevention and treatment of diseases, dysfunction and disorders through proper drug therapy and non-drug therapy
49(3) The practice of pharmacy by pharmacy technicians is limited to:
(a) the distributive component of the dispensing process (drug and product
distribution);(b) compounding and preparing drug products for dispensing;
(c) ensuring accuracy and quality of the final drug product;
(d) supervising and managing drug distribution systems to optimize the safety and efficiency of operations
(e) accepting activities delegated by another health care professional;
(j) directing clients to consult with other health care providers when appropriate; and
(g) other activities defined in the regulations.
49(6) Honorary members and members on retired or non-active registers are not authorized to practise pharmacy.
49(8) Nothing in this Act or the regulations prevents a pharmacy technician on an active or conditional register, who is employed in the public sector, from delegating
functions to a non-technician who is under the pharmacy technician's supervision.57 No person except a pharmacy technician shall use the title pharmacy technician or a variation of such title or an equivalent in another language
. 58 No person shall 'Use the initials "R.Ph.T." or "RPhT“ or initials which would imply that the person is a pharmacy technician, unless the person is a pharmacy technician
60 No person except a pharmacy technician student shall use the title
pharmacy technician student or student pharmacist technician or a variation of such title or an equivalent in another language
Part X: Discipline and Competency
Interpretation
69(1) The following definitions apply in this Part.
"caution" is intended to express the dissatisfaction of the committee and to forewarn the respondent that if conduct recurs, more serious disciplinary action may be Considered. (avertissement)
"censure" is the expression of strong disapproval or harsh criticism. (remontrance) "conduct deserving censure" includes:
(a) professional misconduct;
(b) conduct unbecoming a member of the College;
(c) acting in breach of this Act, the regulations, the Code of Ethics or practice directives;
(d:) incompetence in the practice of pharmacy; and
(e) any other matter that, in the opinion of the Complaints Committee or the Discipline and Fitness to Practise Committee, does not meet the prevailing standards of practice or conduct expected of a member in the practice of pharmacy. (conduit meritant remontrance)
"counsel" is advice as to how to improve the respondent's practice. (conseils)
"Court of Appeal" means The New Brunswick Court of Appeal. (Cour d'appef)
"incapacitated" means, in relation to a member, that the member has a physical or mental condition or disorder, or substance abuse problem that makes it desirable in the interest of the public that the member no longer be permitted to practise or that the member's practice be restricted, and
"incapacity" has a corresponding meaning. (incapacite)
"incompetence" means, in relation to a member, that the member's professional care of a client displays lack of knowledge, skill or judgement, or disregard for the welfare of the client of a nature, or to an extent, that demonstrates that the member is unfit to continue to practise, or that the member's practice should be restricted. (incompetence)
“Professional Misconduct” means the member has:
(a) pleaded guilty to or been found guilty of an offence that, in the opinion of either the Complaints Committee or the Discipline and Fitness to Practise Committee, is relevant to the member's suitability to practise or carry out professional responsibilities;
(b) been adjudged guilty of an act of professional misconduct by the governing body of a health profession in a jurisdiction other than New Brunswick that would, in the opinion of either the Complaints Committee or the Discipline and Fitness to Practise Committee, constitute professional misconduct under this act
(c) digressed from established or recognized professional standards or ethics of the profession;
(d) committed an act of professional misconduct as defined in the regulations;
(e) violated or failed to comply with this Act or the regulations;
f) violated or failed to comply with a condition or limitation imposed on the member's licence;
(g) failed to submit to an examination ordered by the Committee under subsection 86(1);
(h) sexually abused a client;
(i) failed to file a report pursuant to sections 70, 71 or 72 or paragraphs 18 if) or l4(2)(c); or
(j) continued to practise while knowing himself or herself to be incapacitated. (faux professionnelle) "respondent" means a member, former member, applicant or any
person whose conduct is being inquired into under this Act. (intime)
Mandatory reporting of sexual abuse
70(1) A member who, in the course of practising the profession, has reasonable grounds to believe that another health professional has sexually abused a client; and who fails to file a report in writing in accordance with subsection (4) with the governing body of the health professional within twenty- one days after the circumstances occur that give rise to the reasonable grounds for the belief, commits an act of professional misconduct.
70(2) A member is not required to file a report pursuant to subsection (1) if the member does not know the name of the health professional who would be the subject of the report.
70(3) If the reasonable grounds for filing a report pursuant to subsection (1) have been obtained from one of the member's clients, the member shall use his or her best efforts to advise the client that the member is filing the report before doing so.
70(4) A report filed pursuant to subsection (1) shall contain the following information:
(a) the name of the member filing the report;
(b) the name of the health professional who is the subject of the report;
(c) the information the member has of the alleged sexual abuse; and
(d) subject to subsection (5), if the grounds of the person filing the report are related to a particular client of the health professional who is the subject of the report, the name of the client.
70(5) The name of the client who may have been sexually abused shall not be included in a report unless the client, or if the client is incapable, the client's representative, consents in writing to the inclusion of the client's name.
70(6) No action or other proceeding shall be instituted against a member for filing a
report in good faith pursuant to subsection (1).
Other Mandatory Reports
71(1) A person who terminates or suspends the employment of a member or who imposes restrictions on the practice of a member for reasons of professional misconduct, incompetence or incapacity shall file with the Registrar within thirty days after the termination, suspension r imposition a written report setting out the reasons.
71(2)…employment of a member or to impose restrictions on the practice of a member for reasons of professional misconduct, incompetence or incapacity but did not do so because the member resigned, the person shall file with the Registrar within thirty days after the resignation a written report setting out the reasons upon which the person had intended to act.
71(3) This section applies to every person who employs a member.
72(1) A person who dissolves a partnership or association with another member for reasons of professional misconduct, incompetence or incapacity and who fails to file a written report with the Registrar within thirty days after the dissolution setting out the…
72(2) A member who believes that another member is suffering from a physical or mental condition or disorder of a nature or to an extent that the other member is unfit to continue to practise or that his or her practice or pharmacy operation should be restricted, shall inform the Registrar of that belief and the reasons for it.
72(3) Following any action against a member by any other licensing authority, by any health care institution, by any professional association, by any governmental agency, by any law enforcement agency, or by any court, for any act or conduct which could constitute professional misconduct under this Act, or for any conduct which could lead to a finding under this Act that a member is incapacitated or unfit to practise, the member shall report such information to the Registrar without delay.
73 No action or other proceeding shall be instituted against a person for filing a report in good faith under sections 71 or 72
Complains
76(1) A complaint against a respondent shall be:
(a) in writing; and
(b) delivered to the Administrator.
76(2) A complaint against a pharmacy is a complaint against the manager.
77 Any person may file a complaint, including the Administrator when acting pursuant to section 75, or the Registrar in circumstances where no complaint has been received from any other person, and it is in the public interest that action be taken immediately
78(1) Upon receipt of a complaint, or when acting under sections 75 and 80, the Administrator shall:
(a) if necessary, obtain additional information from the complainant and carry out an investigation; and
(b) provide the respondent with
(i) a copy of the complaint, and
(ii) the date by which a reply must be filed with the Administrator, which date shall not be later than twenty-one days after the date when the Administrator mails or delivers the complaint.
78(2) Upon receipt of the respondent's reply the Administrator may:
(a) investigate the complaint further should circumstances require;
(b) settle the complaint to the satisfaction of the complainant if the complaint alleges conduct deserving sanction that appears to the Administrator not to warrant action by the Complaints Committee or Discipline and Fitness to Practise Committee;
(c) refer the complaint to the Complaints Committee;
(d) refer the complaint to the Discipline and Fitness to Practise Committee if the subject matter is, in the opinion of the Administrator, sufficiently serious to warrant such referral; or
(e) dismiss the complaint if, in the opinion of the Administrator, it is without merit
78(3) A complainant who is dissatisfied with the decision of the Administrator in disposing of the complaint may request in writing a review by the Complaints Committee.
78(4) The Administrator or the Complaints Committee shall advise the complainant and the respondent in writing of the disposition of a complaint under subsections (2) or (3), as the case may be, and shall give reasons.
78(5) When a complaint is referred to the Complaints Committee, the Administrator shall provide the Committee with a full report of the results of any investigation, the complaint, the respondent's reply and any documentation and information relevant to the complaint.
78(6) When a complaint is referred to the Discipline and Fitness to Practise Committee, the Administrator shall comply with sections 93 and 95.
78(7) The Administrator shall report his or her actions on all complaints to Council, without disclosing the names of the parties.
79(1) An apology made by or on behalf of a person in connection with any matter that is or may become the subject of a complaint:
(a) does not constitute an express or implied admission of fault by the person in connection with that matter;
(b) does not, despite any wording to the contrary in any contract of insurance or indemnity and despite any other Act or law, void, impair or otherwise affect any insurance or indemnity coverage for any person in connection with that matter; and
(c) shall not be taken into account in any investigation or…
TLDR An Apology is not proof of wrongdoing
79(2) Despite any other Act or law, evidence of an apology made by or on behalf
of a person in connection with any matter that is or may become the subject of a
complaint, including the factual admissions made in the document containing the
apology, is not admissible in any civil or administrative proceeding, in a criminal prosecution or in an arbitration as evidence of the fault, liability or culpability of any person in connection with that matter.
TLDR Doesn’t count if it is during a court case
79(3) Notwithstanding subsection (2), if a person makes an apology while testifying at a civil proceeding, including while testifying at an out of court examination in the context of the civil proceeding, at an administrative proceeding, in a criminal trial or at an arbitration, this section does not apply to the apology for the purposes of that proceeding or arbitration.
Investigation Complaints
80 The Administrator shall investigate all matters that may constitute conduct deserving sanction, notwithstanding that no complaint has been received under section 78, or the complaint has been withdrawn, and may carry out investigations on the request of any person or of Council.
81 If an investigation under section 80 discloses that a respondent may deserve sanction, the Administrator shall cause a complaint to be filed with the Complaints Committee or refer the complaint directly to the Discipline and Fitness to Practise Committee, as per subsection 78(2).
Product Selection and Privacy
128(1) - A pharmacist may dispense a pharmaceutically equivalent, a pharmaceutical alternative or a therapeutic equivalent, all as defined in this Act or in the regulations, unless otherwise directed by the prescriber, or requested by the client.
No liability for dispensing pharmaceutically equivalent products
129 - No action or other proceeding lies or shall be instituted against a prescriber, pharmacist or any member under the supervision of a pharmacist, on the grounds that a pharmaceutically equivalent or a pharma ceutical alternative other than the one prescribed was dispensed in accordance with this part
What is personal information?
Be careful what we share and use for information
Under PIPEDA, personal information includes any factual or subjective information, recorded or not, about an identifiable individual. This includes information in any form, such as:
age, name, ID numbers, income, ethnic origin, or blood type;
opinions, evaluations, comments, social status, or disciplinary actions; and
employee files, credit records, loan records, medical records, existence of a dispute between a consumer and a merchant, intentions (for example, to acquire goods or services, or change
jobs).The principles are:
1.Accountability
2.Identifying Purposes
3.Consent
4.Limiting Collection
5.Limiting Use, Disclosure, and Retention
6.Accuracy
7.Safeguards
8.Openness
9.Individual Access
10.Challenging Compliance
Accountability
Your responsibilities
Comply with all 10 fair information principles.
Appoint someone to be responsible for your organization’s PIPEDA compliance.
Protect all personal information held by your organization, including any personal information you transfer to a third party for processing.
Develop and implement personal information policies and practices.
Identifying Purposes
Identify and document your purposes for collecting personal information. This will help you determine which specific personal information to collect to fulfill those purposes.
Tell your customers why your organization needs their personal information before or at the time of collection. Depending on how the information is collected, this can be done orally or in writing.
Obtain their consent again should you identify a new purpose.
Consent
Meaningful consent is an essential element of PIPEDA. Organizations are generally required to obtain meaningful consent for the collection, use and disclosure of personal information.
To make consent meaningful, people must understand what they are consenting to. It is only considered valid if it is reasonable to expect that your customers will understand the nature, purpose and consequences of the collection, use or disclosure of their personal information.
Consent can only be required for collections, uses or disclosures that are necessary to fulfil an explicitly specified and legitimate purpose. For non-integral collections, uses and disclosures, individuals must be given a choice.
The form of consent must take into account the sensitivity of the personal information. The way you seek consent will depend on the circumstances and type of information you are collecting. Individuals can withdraw consent at any time, subject to legal or contractual restrictions and reasonable notice, and you must inform individuals of the implications of withdrawal.
Limiting Collection
Collect only the personal information your organization needs to fulfill a legitimate identified purpose.
Be honest about the reasons you are collecting personal information.
Collect personal information by fair and lawful means. This requirement is intended to prevent organizations from collecting information by misleading or deceiving about the purpose
Limiting Use, Disclosure, and Retention
Unless someone consents otherwise—or unless doing so is required by law—your organization may use or disclose personal information only for the identified purposes for which it was collected.
Keep personal information only as long as it is needed to serve those purposes. Know what personal information you have, where it is, and what you are doing with it.
Obtain fresh consent if you intend to use or disclose personal information for a new purpose.
Collect, use or disclose personal information only for purposes that a reasonable person would consider appropriate in the circumstances.
Put guidelines and procedures in place for retaining and destroying personal information.
Accuracy: Minimize the possibility of using incorrect information when making a decision about an individual or when disclosing information to third parties.
Safeguards
Protect personal information in a way that is appropriate to how sensitive it is.
Protect all personal information (regardless of how it is stored) against loss, theft, or any unauthorized access, disclosure, copying, use or modification
Openness: Inform your customers and employees that you have policies and practices for managing personal information.
Make these policies and practices easily understandable and easily available.
Individual Access:When asked, advise people about the personal information about them your organization holds.
Explain where the information was obtained.
Explain how that information is or has been used and to whom it has been disclosed.
Give people access to their information at minimal or no cost, or explain your reasons for not providing access. Providing access can take different forms. For example, you may provide a
written or electronic copy of the information, or allow the individual to view the information or listen to a recording of the information.
Correct or amend personal information in cases where accuracy and completeness is deficient.
Note any disputes on the file and advise third parties where appropriate.
Challenging Compliance
Provide recourse by developing simple complaint handling and investigation procedures.
Tell complainants about their avenues of recourse. These include your organization’s own complaint procedures, along with those related to industry associations, regulatory bodies and the OPC.
Investigate all complaints you receive. Improve any information-handling practices and policies that are found to be problematic
Non-Disclosure of Confidential information and documents
140(1) A person who, in the course of carrying out duties under this Act or the regulations, becomes aware of information Or a document that is confidential has the same obligation
respecting disclosure of that information or document as the member from whom the information or document was obtained.140(2) A member who, in accordance with this Act or the regulations, provides the College with information or a document that is confidential shall be deemed not to have breached any duty or obligation that the member would otherwise have had to the College or the client not to disclose the information or document.
140(3) A person who, during the course of any court proceeding with respect to a matter under this Act or the regulations, becomes aware of information or a document that is confidential shall not utilize, produce or disclose the document or information for a purpose other than that for which it was obtained
140(4) In any court proceeding with respect to a matter under this Act or the regulations, the Court may exclude members of the public from the hearing where the Court considers the exclusion is necessary to prevent the disclosure of information or the production of a document that is confidential.
140(5) In giving reasons for judgement in any court proceeding, the Court shall take all reasonable precautions to avoid including in its reasons any information before the Court that is confidential.
140(6) In addition to the requirements in this Act and in the regulations, members shall comply with the requirements of the New Brunswick Personal Health Information Privacy and Access Act, or any successor legislation
Code of Ethics (02/28)
Self-regulation is a privilege granted by government on the condition that the self-regulating profession agrees to put the interests of the public above its own interests collectively, and above registrants’ interests individually. The alternative to self-regulation is unilaterally- imposed government regulation. The Act requires that all decisions and activities of the College be made in the public interest
Acting in the public interest broadly encompasses:
Duties to the public: To promote and protect the health, well-being, safety and
interest of the public (i.e., individuals who utilize pharmacy services or “patients”)Duties of Conduct: To hold forth the independence, integrity and honour of the profession.
Purpose:
Competency and ethics are tightly intertwined and the CoE (code of ethics) is applicable to all pharmacy practice whether direct patient care or otherwise. All registrants are responsible to the College and therefore the public for application of the CoE in the context of their professional environment. This document provided by NBCP is a foundation for practice that interlinks with standards of practice; provincial and federal legislation; and College regulation
The Code of Ethics is used by the Public, Registrants and the College in order to:
Articulate the ethical principles for pharmacy professionals
Serve as an educational resource
Self-evaluate knowledge, skills and attitudes pertaining to ethics in the course of Continued Professional Development
Establish a basis for the evaluation of registratints’ conduct in the course of complaints and discipline proceedings
This CoE purposefully provides a conceptual rather than a granular approach to codifying pharmacy professionals’ ethical practice.
Registrants may not justify unethical behaviour by rationalizing that a given behaviour is not expressly prohibited by this CoE. (Code of Ethics)-pertains where direct or not
Authoring an exhaustive list of ethical rules is unrealistic given the infinite number of situations and scenarios potentially presenting in practice
Value Based Decision Making (00:11:48)
STEP 1 Establish the facts Identify conflicting or competing values
Prioritize core value of promoting and protecting public interest Promoting and protecting the public interest is the core value of pharmacy practice in New Brunswick. Registrants have a duty to embody this value and incorporate it in every aspect of their daily practice, not just when faced with a difficult ethical dilemma.
Registrants should habitually ask themselves: skills can be developed and improved with practice
Will what I am about to do result in promoting and protecting the health, wellbeing, safety and interests of the public and/or patient?
Will what I am about to do hold forth the independence, integrity and honour of the profession?
In determining the correct action, it emphasizes performing that action;
In the correct manner,
At the correct time,
With the correct people
And for the correct reasons
It is a methodology that results in the application of good judgement.
Judgement that is consistently motivated by a duty to promote and protect the public
interest, as well as judgement that holds forth the independence, integrity and honour of the profession.
Process of Values-Based Decision Making (00:20:54)
STEP 1: Establish the Facts
Understand the facts as completely and objectively as possible. The focus is to assemble the relevant factual information without judgement. This is known as identifying the context within which a decision is made.
Although the contextual facts are essential to VBDM, it is crucial to understand that the facts alone will not determine what should be done. Values ultimately determine the result of a given decision
STEP 2: Ensure Everyone Agrees on the Facts
Determine whether the relevant stakeholders agree on the facts or if there are any factual disagreements. This is important because the VBDM methodology cannot function unless there is agreement on the facts. At this point it is possible to have total agreement on the facts but to disagree about the appropriate course of action. This is a values conflict.
STEP 3: Identify the Conflicting or Competing Values of the Parties Involved
Identify and understand the values that are at play in the particular fact situation. The decisive factor in every decision, whether realized or not, is a ”judgement” based on a “value” (i.e., a value judgement). Sometimes these ‘value judgements’ are made instinctively, intuitively, or are the result of our beliefs and/or assumptions. Nevertheless, values are present in every decision and they ultimately determine what course of action will be pursued. Therefore, this step in the process is to understand and identify the values that
are “in play” within the context of the decision to be made.
STEP 4: Prioritize the Core Value of Promoting and Protecting the Public Interest (i.e., duties to the public and/or duties of conduct)
Analyze the values that are in conflict and then determine how to implement the value of promoting and protecting the public interest, in other words, prioritize the duties to the public and/or duties of conduct. All values conflicts should be resolved in favour of promoting and protecting the public interest and hold forth the independence, integrity and honour of the profession. After determining the decision that will promote and protect the public interest, the action must be performed in a contextually appropriate manner; that is, in the correct manner, at the correct time, with the correct people, and for the correct reasons. The exercise of good judgement is paramount
Bioethical Principles (00:26:27)
Beneficence:
Protect the interest of the patient to their benefit
The first foundational principle that forms and guides our commitment to serve and protect the best interests of our patients establishes the fact that our primary role and function as healthcare professionals is to benefit our patients. We need to remember that our patients seek our care and services because they believe and trust that we will apply our knowledge, skills and abilities to help make them better.
Non Maleficence (do no harm, and prevent harm from occurring)
The second foundational principle that guides our commitment to serve and protect the best interests of our patients addresses the reality that as we strive to benefit our patients we must be diligent in our efforts to do no harm and, whenever possible, prevent harm from occurring.
Components of practice that may be ethically fraught include stakeholder’’ financial interests influencing patient care, scope of practice boundaries, disclosing and documenting medication errors and near-misses, transitioning of care between providers or environments,
conscientious objection and allocating sufficient resources to provide comprehensive patient centered pharmaceutical care/medication management.
Respect for Persons (1:25:00)
Respect for persons is generally understood as the requirement that all patients be treated with dignity. There is an inherent vulnerability associated with being a patient and therefore
patients must be able to trust that the health care professional is motivated primarily by the core value of what is best for the patient. The registrant should consider the impact on the dignity of the patient. Would the potential action respect the inherent dignity of the patient or would it be an example of using the patient as a means to achieve an alternative goal? The focus should be on patient-centered care.Particularly challenging aspects of practice that this principle applies to include managing professional patient relationships, informed consent/refusal, substitute decision makers, advanced health directives, freedom of patient choice of pharmacy, and fiduciary duties of the professional.
Justice
The social aspect of the principle of justice is paramount. Justice includes the broader social obligations to protect the public interest and includes facilitating equitable access to services and conducting business ethically. Particularly challenging aspects of practice that justice impacts upon include allocation of rationed medication, patient incentives strategies, gifts, documentation, assumption and abrogation of responsibility, conflict of interest, dual relationships, advertising and referrals.
The four bioethical principles can be brought together with the VBDM methodology. As the professional answers yes or no to the two VBDM questions regarding duty to the patient and duty to the profession, the principles provide the ‘how’ to the answer. If the answer is ‘no’ then a statement can be made, “The individual value held by party X does not adhere to Y bioethical principle”. This is analogous to the statement of a drug-related problem within the Pharmaceutical Care Process.
Conflict of Interest (1:38:00)
A conflict of interest can be defined as any situation, interaction, or decision in which the professional’s personal and/or financial values (or the personal and/or financial values of another person) have the potential to influence or compromise the professional’s judgement. For the purposes of this Code of Ethics, there is no meaningful difference between an actual conflict of
interest and a perceived conflict of interest. The ethical management of the two is identical and typically starts with a “disclosure” to the relevant body, e.g., management or the New Brunswick College of Pharmacists (the College).Perceive conflict and actual conflict are treated the same
Conscientious Objection (00:54:40)
A conscientious objection is an opinion held by a professional that precludes participation in the delivery of an aspect of patient care. Pharmacy professionals may hold sincere beliefs of a conscientious nature that prevent the registrant from performing certain actions. If the service is permitted legally and prescribed by an authorized prescriber, then a claim to conscientious objection means that, “but for”, the conscientious objection the registrant would normally have a duty to provide the service.
that service has to be given to that patient
Fiduciary Relationship, Best Interest of the Patient, and Professional Boundaries (00:58:11)
The health professional and the patient are engaged in a therapeutic relationship. This relationship is characterized by a power imbalance. The professional is in a power position as a result of possessing specialized knowledge that the patient requires and the patient is vulnerable by virtue of being in need of that knowledge. A consequence of this power imbalance is that the professional owes the patient a fiduciary duty, in other words the professional has a duty to act in the patient’s best interest. This will require, amongst other considerations, the establishment of professional boundaries.
Informed Consent (01:00:15)
Informed consent requires the health professional to disclose the amount of information that a reasonable person in the patient’s position would want to know. Informed patient consent can be garnered only if the patient understands treatment benefits and risks. Consent can be implied or expressed
Mental Competency, Proxy and Substitute Decision Makers, and Advanced Health
Care Directives (1:02:07)
TLDR if a person is no longer to make sound decisions they can appoint a proxy to make decisions for them
On December 16th 2016, the New Brunswick Advanced Health Care Directives Act received Royal Assent. This Act allows anyone, who has the capacity, to make an advanced health care directive that would come into effect should that person lose his or her capacity to make health care decisions In addition to permitting advanced health care directives, this Act allows the patient to appoint a proxy to make decisions on behalf of the patient. The term proxy is used in this legislation; however, the term “substitute decision maker” is used in a parallel way in other Acts.
Patient-Centered Care (1:47:00)
Patient-centered care is an approach where health professionals and patients work together to meet the individual healthcare needs of the patient. Patient-centered care is a continual effort to ensure the needs and choices of the patient are being met. The concept of patient centered care is often expanded to include families as well; hence the term “patient and family-centered
care.” Regardless of the label, the insight of this approach is the meaningful inclusion of patients (and often families) in the health care decision making process.
Model for Ethical Decision Making
Ethical Issue Vs. Ethical Dilemma
What is an ethical issue?
A situation that raises an ethical question about what is right or wrong.
What is an ethical dilemma?
An ethical dilemma involves a situation which raises an ethical question about what is right or wrong which also involves a conflict of values.
conflict of value which is person on what you see
When faced with a ethical decision ask yourself the following:
What is the situation? What’s going on here really? What are the facts? What am I assuming?
Is this an ethical issue or an ethical dilemma?
Identify the people involved?
Identify any values or principles involved and any potential conflicts.
look beyond who or what is actually the problem
What are my motives in all of this?
Personal values/principles
Self-aware and honest about your motives and intentions
Are you motivated by your patient’s best interest?
Does a clear answer already exist?
What does the “rules” say regarding this situation?
Code of Ethics
Regulations/legislation
NBCP Policies or guidelines
keep pure motives
can you put feelings aside is it black and white?
Consult with a colleague and ask yourself the following:
How would I feel if I were the patient in this situation?
How would I feel if my action were made public?
What would happen if all healthcare professionals did this?
Ask around
talk to someone you trust and give them the raw situation
What is the best option and why?
Come up with 3 viable options
Doing nothing can be an option
Identify the pro’s and con’s of each option
Pick the option you consider to be the best and document why you consider it to be the best option
What have I learned from this?
Review your decision after some time has passed.
Was the outcome favorable? If it was, why? If it was not, why?
What could I do differently if faced with a similar situation?
sometimes people just leave even if everything was done right
Law, Ethics and Professionalism
Pharmacy Oversight
History of Drug Regulation
In the 19th century, there was not regulation
Opium was liberally used in many medications.
No regulations protected consumers and many “medicines” made claims not backed by science
Laws, oversight agencies, and professional organizations emerged in the 20th century as a way to regulated medicine
Federal and state regulatory agencies include:
Health Canada
Health Protection Branch
Federal Trade Commission
Centers for disease Control and Prevention
Provincial Colleges of Pharmacy
Professional organizations include:
National association of Pharmacy Regulatory Authorities
Canadian Pharmacists Association
Canadian Society of Hospital Pharmacists
There are four primary types of oversight
Laws
Regulations
Standards
Ethics
Laws: overall all rules that are passed by the legislative branches of federal, provincial, and local governments to guide conduct
Regulations: Legislated rules and procedures that exist to carry out the law
Standard: Benchmarks or desired normal level of quality for a product or professional performance
Ethics: following a code of high professional standards
Drug: includes any substance or mixture of substances manufactured, sold or represented for use in:
(a) the diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals,
(b) restoring, correcting or modifying organic functions in human beings or animals, or
(c) disinfection in premises in which food is manufactured, prepared or kept; (drogue)
Professional Pharmacy Organizations & Associations
NBCP http://www.nbpharmacists.ca/
Establishes standards of knowledge and skill for members, keeping pace with medical and pharmaceutical advancements
Serves as the vehicle for public complaints about pharmacists and, where appropriate, provides disciplinary measures
Provides standards of qualification for licensed pharmacists and registered students
Provides standards of practice for licensed pharmacists, licensed certified dispensers and licensed students
Provides and ensures adherence to a code of professional ethics
Requires members to participate in professional development and training programs
Regulates the circumstances under which a licensed pharmacist may prescribe drugs, devices, and treatment and pharmacies may sell them
Establishes and maintains standards for the operation of pharmacies
Establishes regulations for practice agreements with other health professions
NBPA
similar to CPHA
able to purchase liability insurance cheaper
advocating to us as healthcare professionals
advocate to the insurance companies in the business side and image side
NAPRA-http://napra.ca/pages/home/default.aspx
Who they are?
Non profit association established in 1995
Membership includes all provincial/territorial regulatory authorities & the Canadian Armed Forces
Pharmacy Services
Mandate: to protect the public through regulation of pharmacy practice and operation of pharmacies Governed by a board of directors
What they do?
Maintain and administer the National Drug Schedules (NDS)
Develop national model standards, guidelines, frameworks to achieve a
harmonized practice frameworkFacilitate the development and maintenance of reciprocity frameworks for pharmacists
Represent and act as a national voice for pharmacy regulatory issues in Canada
Undertake initiatives of national importance on behalf of its members
CAPT-
http://capt.ca/
Deals with accreditation
Vision: CAPT is the national association providing an influential voice, leadership and support to pharmacy technicians and pharmacy support staff facilitating practice excellence contributing to positive health outcomes
Mission: CAPT will advocate and promote the role of the pharmacy technician and pharmacy support staff and the advancement of the profession CAPT will support and empower pharmacy technicians and pharmacy support staff in the pursuit of practice excellence through:
Communication
Education and professional development opportunities
Partnerships and collaboration with pharmacy stakeholders
PEBC
The Pharmacy Examining Board of Canada (PEBC) is the national certification body for the pharmacy profession in Canada.
PEBC is a non- profit organization with more than 45 years of experience in assessing the qualifications and competence of candidates for licensing by pharmacy provincial regulatory authorities.
The purpose of the Pharmacy Examining Board is to assess qualifications for pharmacists and pharmacy technicians on behalf of participating provincial regulatory authorities
The Board evaluates qualifications, develops and administers examinations
national Qualifying Examination
issues Certificates of Qualification
CPhA-http://www.cshp.ca/
The Canadian Pharmacists Association is the national organization of pharmacists, committed to advancing the profession of pharmacy so as to contribute to the health of Canadians . CPhA’s website is your link to a comprehensive source of drug information, pharmacy practice support material, patient information and news about the world of pharmacy
CSHP-http://www.cshp.ca/
Canadian society of Hospital Pharmacists is the national voice of Pharmacists' committed to the advancement of safe, effective medication use and patient care in hospitals and related health care settings.
ISMP- https://ismpcanada.ca/
The Institute for Safe Medication Practices Canada is an independent national not-for-profit organization committed to the advancement of medication safety in all healthcare setting
Neighborhood Pharmacy Association of Canada- http://www.neighbourhoodpharmacies.ca/
TLDR Run the business side of independent pharmacies to help prevent adverse drug reactions, operating an efficient supply chain and by providing innovative drug therapies and lower-cost generic drugs
They are: focused on the business of neighborhood pharmacy to ensure our members can continue to deliver the convenient, professional patient care products and services on which Canadians rely. Our commitment is repaid in trust, as 80% of Canadians consult their pharmacists for professional healthcare, at nearly 9,000 neighborhood pharmacies across the country.
They represent: the operators of Canada’s approximately 6,500 chain, banner and franchise neighborhood pharmacies, as well as grocery chains and mass merchandisers with pharmacies. Neighborhood pharmacy helps save the Canadian healthcare system more than $12.5 billion annually, preventing adverse drug reactions, operating an efficient supply chain and by providing innovative drug therapies and lower-cost generic drugs
They look at independent pharmacies
HPB
The Health Protection Branch is responsible for the development and implementation of legislation, policies and programs in the areas of Environmental Health Protection Community Care Facilities and Emergency Prepare
Legislation: Canada Health Act
CHA Objective
The Act sets out the primary objective of Canadian Health Care Policy
To protect, promote and restore the physical and mental well-being of residents of Canada and to facilitate reasonable access to health services without financial or other barriers
Was enacted by Health Canada in 1984 and represents the cornerstone of the Canadian Health System
Ensures that all eligible residents of Canada have reasonable access to insured health services on a prepaid basis, without direct charges at the point of service for such services
Provides for criteria and conditions that the provinces and territories must fulfill to receive the full federal cash contribution under the Canada Health Transfer (CHT)
Criteria:
To receive CHT each province/territorial health insurance plan must fulfill the following criteria/conditions
Public administration: must be carried out by a non profit/ by public authority
Comprehensiveness: all necessary services must be insured/covered
Universality: all persons insured must receive uniform coverage
Portability: insured services must be maintained when an insured person moves or travels
Accessibility: services must be unimpeded by financial or other barriers
Implementing the CHA
Provincial/Territorial Role
Canada does not have a single national health care plan, but rather a national health insurance program, which is achieved by a series of thirteen interlocking provincial and territorial health insurance plans, all of which share certain common features and basic standards of coverage
Under the Canada Health Act, our national health insurance program is designed to ensure that all residents of Canada have reasonable access to medically necessary hospital and physician services on a prepaid basis, and on uniform terms and conditions
Insured Services
Provincial and territorial health insurance plans are required to provide insured persons with coverage of insured health services, which are:
Hospital Services: provided to inpatients or outpatients, if the services are medically necessary for the purpose of maintaining health, preventing disease or diagnosing or treating an injury, illness, or disability
medically required physician services rendered by medical practitioners
Other Benefits
Provinces and territories may also offer "additional benefits" under their respective health insurance plans, funded and delivered on their own terms and conditions
These benefits are often targeted to specific population groups (e.g. children, seniors, social assistance recipients), and may be partially or fully covered
While these services vary across different provinces and territories, examples include prescription drugs, dental care, optometric, chiropractic, and ambulance services
Uninsured Services
A number of services provided by hospitals and physicians are not considered medically necessary, and are not insured by provincial and territorial health insurance plans
Uninsured hospital services for which patients may be charged include preferred hospital accommodation unless prescribed by a physician; private duty nursing services; and the provision of telephones and televisions
Uninsured physician services for which patients may be charged include prescription renewals by telephone; the provision of medical certificates required for work, school, insurance purposes and fitness clubs; testimony in court; and cosmetic services
Financing Health Insurance Service
Financing
Provinces and territories have considerable autonomy in determining how to finance health insurance plans
Financing can be addressed through the payment of premiums (as in British Columbia), payroll taxes, sales taxes, other provincial or territorial revenues, or by a combination of methods
Health insurance premiums are permitted as long as residents are not denied coverage for medically necessary hospital and physician services because of an inability to pay such premiums
Provinces/territories that levy premiums also offer financial assistance based on income so that low- income residents can have their payments reduced or be entirely exempted from paying premiums
Federal FDA
Food and Drugs Act
There are 4 Active Schedules
Schedule A: disease stated or conditions for which treatments may not be promoted to the public
asthma, cancer, depression, must comply with specific requirement if they are to be promoted as a treatment or cure
advertising is restricted
Schedule B: Publications describing official or international standards
Any drug or substance to be sold in Canada must meet this criteria and standards
Schedule C: radiopharmaceuticals
Schedule D: Allergenic substances, blood derivatives, immunizing agents
Schedule G: Controlled Drugs
Prescription Drug List
Drugs excluding those found in the Control Drug and Substance Act
FDA Regulations
The most important regulations for the pharmacy are the food and drug regulations, the Natural Health Products regulations and the medical devices regulations
Food and Drug Regulations
Part A: Administration
Part B: food production and food safety
topics such as baby food, alcohol, flavoring and daily products
also overseeing food safety and inspection
Part C: drugs and defined the rules for dispensing
from raw material to the final customers product
much of this part is directed to the manufacturers
Part D: vitamins, minerals and amino acids
Part E: cyclamen and saccharin sweeteners
Part G: controlled drugs
Part J: restricted drugs
For members of the pharmacy profession, the two key sections of the regulations are Part C, which deals with drugs and part G Controlled Drugs
Definitions Under the FDA
Practitioner: refers to a person who is entitled under the laws of a province to treat patients with a prescription drug and is practicing their profession in that province
Child Resistant Package: is a package that meets the child test protocol requirement of the Canadian Standards Association or other standards as specified in the Food and Drug Regulations.
The CSA is an organization that test, certified, and designates containers as child resistant
Part C Symbols
The requirements and symbols used for manufacturers labelling drug packages (i.e. stock bottles) are found in the Food and Drug Regulations.
Pr: refers to the product requiring a prescription for sale
N: narcotic
C: controlled Drug
TC: benzodiazepines or other targeted substances
Manufacturing
The process for approving a drug is regulated from beginning to end from:
providing the clinical evidence for efficacy and safety of the drug,
the raw materials used to manufacture the drug, and to
the final drug product
The Food and Drugs Act and the Food and Drug Regulations describe the regulatory requirements for manufacturers of drug products (i.e. pharmaceutical companies) including Good Manufacturing Practices (GMP)
Once a manufactured drug product is approved by Health Canada, it is given market authorization and a unique Drug Identification Number (DIN). The issuance of a DIN means a drug has been approved for sale in Canada.
Health Canada regulates the distribution of drugs through the issuance of Drug Establishment Licenses (DEL) which permit various activities such as:
fabricate or manufacture drugs;
package and/or label products;
test drugs;
distribute various classes of drugs:
import or wholesale drugs.
Inspections consist of premises, equipment, personnel, sanitation, raw material testing, quality control, finished product testing, sampling, stability, record keeping
Compounding
Are prepared pursuant to a prescription within an established pharmacist-patient relationship.
Require a consultation between the pharmacist and the patient (or patient's agent) in which the pharmacist uses their knowledge and expertise
Provide a customized therapeutic solution to improve patient care.
Do not circumvent a regulatory process or patent laws.
Manufacturing Vs Compounding
Manufacturing: regulated and enforced federally
Compounding: regulated by provincial regulatory authorities , in accordance with guideline and standards to ensure the quality and safety of compounded drug products
Health Canada's Policy on Manufacturing and Compounding Drug Products (POL-0051) provides information on the manufacturing and compounding of drugs in Canada.
Food and Drug Regulations
Health Canada provides warnings and advisories through its database (Recalls and Safety alerts Database) that lists recalls, advisories and safety alerts.
The mandatory health requirements that must be filed by Health Canada includes informing them of the nature of the recall and the actions that are being taken to remove the product
Types of Recalls
Health Canada’s Health Products and Foods Branch will determine what level or depth of recall is required. For drug recalls , this is listed as a Hazard Classification and is based on the risk of harm to the consumer.
Type I Recall
the most serious
This is a situation in which there is a reasonable probability that the use of, or exposure to, a product will cause serious adverse health consequences or death
example 1: medications with incorrect strength of label
Type II Recall
This is a situation in which the use of, or exposure to, a product may cause temporary adverse health consequences or where the probability of serious health consequences is remote.
example 2: foreign matter in tums
Type III Recall
This is a situation in which the use of, or exposure to, a product is not likely to cause any adverse health consequences.
example: incorrect image labeling
Suspected Adverse Drug Reactions
Suspected adverse drug reactions are also a mandatory reporting requirement for manufacturers. Any adverse reaction reports received by the manufacturer must be reported within 15 days to Health Canada. Reporting by the public or health professionals is voluntary although health professionals are encouraged to report adverse drug reactions to MedEffect ™ Canada through the Canada Vigilance Program
Canada Vigilance Program
The Canada Vigilance Program: is Health Canada’s post-market surveillance program that collects and assesses reports of suspected adverse reactions to health products marketed in Canada
This includes both prescription and non-prescription medications, natural health products and vaccines
In addition MedEffect also posts warnings, advisories and recalls that are in effect. When a number of reports are received for a certain drug , Health Canada may order a review of a product and take action where there is a potential risk to the public.
NAPRA
The National Association of Pharmacy Regulatory Authorities (NAPRA) manages and maintains the National Drug Schedules. Scheduling amendments made to the National Drug Scheduling System are immediately effective in New Brunswick
Scheduling amendments (changes) made to the National Drug Scheduling System based on some factors which include clinical experience with use of the product, its dose, package sizes or patient population i.e. adult use vs pediatric use
The National Drug Scheduling Advisory Committee adopted a cascading principle model whereby drugs are assessed, based on a number of risk factors, to determine whether they are considered Schedule I, II or III. If a product does not meet any of the factors to be scheduled, it is considered unscheduled (U).
ALL drugs in Schedule I, II or III MUST be sold in a pharmacy, but conditions for sale range from most strict in Schedule I which require a prescription, to the least strict in Schedule III where they can be sold in the self-selection area of the pharmacy
Products that are unscheduled (U) may be sold from any retail outlet.
Schedules
Schedule I Drugs
require a prescription
are the same as the drugs listed in Schedule I
Include all the drugs listed in Prescription Drug List (PDL)
Also including ALL of the drugs found in the Schedule of the Controlled Drugs and Substances Act
Schedule II Drugs: Only available through professional intervention by a pharmacist
Do not require a prescription
Kept in a restricted area of a pharmacy not accessible to the public
Schedule III Drugs: available without a prescription
However, they can only be sold in a pharmacy from the dispensary or from an area of the pharmacy (as required by the college) that allows for patient self selection.
A member of the college must be available if needed
Schedule U or unscheduled
May be sold without professional supervision or intervention
These substances are not included in Schedules I, II or III and may be sold from any retail outlet
Adequate information is available on the product packaging and labelling for the patient to make a safe choice and to ensure the patient uses the product appropriately
The Schedules change and it is important to keep updated
Monday
CSDA
Includes the Narcotic Control Regulations and the Regulations pertaining to controlled drug and restricted drugs
One law governs all drugs and substances in Canada, and all drugs and substances under this law are called Controlled Substances
The CDSA controls the manufacture of narcotics, controlled and targeted drugs in Canada and regulates the selling of these products from wholesalers and manufacturers to pharmacies
It also regulated who may prescribe controlled substances
a controlled drug is any drug list in the schedule to Part G of the Food and Drug Regulations
8 Schedules
Schedule I: Old Narcotic Schedule
Schedule II: Cannabis, its preparations and derivatives
Schedule III:
Schedule IV: old controlled drugs and targeted drugs
Schedule V: restricted use or banned in Canada
Schedule VI: Ephedrine, pseudoephedrine and 4 other drugs
Schedule VII: Cannabis resin up to 3 kg old Controlled Drugs
and Cannabis marihuana up to 30g
Schedule VIII: Cannabis resin up tp 1g and Cannabis marihuana up to 30g
Schedule I
opium
Codeine
Morphine
Hydrocodone
Cocaine
Methadone
Pentazocine
Fentanyl
Schedule III
Amphetamines
Methylphenidate
Methaqualone
LSD
Psilocybin
Mescaline
Schedule IV
Barbiturates and salts
Thiobarbiturates and salts
diethylpropion
phentermine
butorphanol
nalbuphine
meprobamate
benzodiazepine
anabolic steroids
Schedule VI
Ephedrine, pseudoephedrine and 4 other drugs
Precursor chemical- chemicals that are frequently used in illicit production of controlled substances
ex. ephedrine and pseudoephedrine, commonly used in cold and decongestant medicine, are precursor chemicals that are used to produce methamphetamine
Double Doctoring
an offence under the CDSA
Obtaining a Substance
s.4 (2) No person shall see or obtain a substance included in Schedule I-IV or an authorization to obtain a substance included in Schedules I-IV from a practitioner, unless the person discloses to the practitioner particulars, relating to the acquisition by the person of every substance in those Schedules, and of every authorization to obtain such substances**, from any other practitioner within the proceeding 30 days**
Double Doctoring: Getting a prescription without disclosing to the prescriber your prescription history
the patient MUST inform the prescriber of any controlled substances that they have been prescribed in the last 30 days
Ordering
Only a person with Signing authority may order controlled substances. Persons with signing authority include the owner/manager of the pharmacy or any other staff pharmacist
Any employee of the pharmacy can sign the manifest when controlled drugs are delivered to the pharmacy but the person with signing authority must sign for the drugs within 48 hours
Narcotic and Controlled Drug register
Narcotic and Controlled Drug Register: maintained in the pharmacy in either electronic format or manual format
the register consists of the Narcotic purchase record and the narcotic sales record. All controlled substance drugs must be recorded in the Narcotic Purchase Record
Reportable narcotics and controlled drugs need to be recorded in the narcotic sales record. This would include methadone sales
Sales Records are printed every 2 weeks and maintained on site for audit purposes
What is a Narcotic Drug
Any substance set out in the Schedule to the Narcotic Control Regulations, or anything that contains a substance listed in the schedule
Categories
narcotic drugs/ straight narcotics
Verbal prescription narcotic
OTC narcotic preparation
Filling Narcotic and Controlled Prescriptions
Narcotic and controlled prescription are filed by prescription number in a separate file from other prescriptions and are coded differently than regular prescriptions
If 2 medications are on the same prescription from, other original is stored with the narcotic while the copy is places with the regular prescriptions, cross referencing both prescription number
Narcotics and controlled drugs are to be kept in a locked cupboard or safe
Returning-Destroying Narcotics-Controlled Drugs
Expired drugs are based on manufacturer policy and with prior permission
part bottles can be destroyed and the destruction must be witnessed by a second person
Inventory is signed and dated by both the person destroying and the person witnessing the destruction with a copy placed in files for storage
OTC Narcotics= exempted Narcotics
OTC Narcotics will contain less than 8 mg of codeine if solid and 20mg/ 30ml if liquid and are to be stored in the non-patient access area of the pharmacy where the pharmacist can be involved in the sale of the product and the sale can be documented
Types of Narcotics and Controlled Drugs
Reportable Narcotics= straight narcotics= must be entered in Narcotic sales record
contains at least one Schedule I drug (N) + 1 other non-narcotic ingredient
injectable
from opium- containing heroin, hydrocodone, methadone, oxycodone
All products with pentazocine or dextropropoxyphene
verbal orderrefillspart-fills are allowed if quantity and interval are indicated
Transfers not permitted
NCR: Definition of Prescription
Prescription means, in respect of a narcotic, an authorization given by a practitioner that a stated amount of the narcotic be dispensed for the person named on the prescription
The quantity to dispense MUST be directly stated or it must be written in a way that an exact amount can be calculated
Possession
A person is permitted to possess a narcotic if
it for a Business or profession
receive pursuant to a prescription
if they are a hospital employee
employed as law enforcement- inspector, member of the Royal Canadian Mounted Police, police constable, peace officer or a part of the Government of Canada in purpose and connection with such employment
Narcotic Control Regulations
What is a “STRAIGHT” Narcotic
not defined in legislation
it is defined by what it is not by applying definition for verbal “backwards” and excluding otc narcotics
CONTAINS a single narcotic ingredient only, OR contain a narcotic and only ONE medicinal; ingredient other than a narcotic in a recognized therapeutic dose,
BE INTENDED for parenteral administration, OR
(CONTAIN hydrocodone, methadone, oxycodone or pentazocine
Verbal Narcotic Preparations= verbal prescription narcotics= non-reportable
contains 1 narcotic + 2 non-narcotic drugs
non-injectable
does not contain heroin, methadone, hydrocodone, oxycodone and pentazocine
no refills
part-fills allowed
no transfers
OTC Narcotics= exempted narcotic compounds
Codeine is only narcotic ingredient
less than 8 mg per solid dosses or 20 mg/30 ml in liquid
+2 other non-N ingredients
no Rx required
non-patient access area
sales may be documented
OTC Codeine Preparation (s.36)
(1)Subject to subsection (2), a pharmacist may, without a prescription, sell or provide a preparation containing not more than 8 mg or its equivalent of codeine phosphate per tablet or per unit in other solid form or not more than 20 mg or its equivalent of codeine phosphate per 30 mL in a liquid preparation if
(a) the preparation contains
two additional medicinal ingredients other than a narcotic in a quantity of not less than the regular minimum single dose for one such ingredient or one-half the regular minimum single dose for each such ingredient, or
three additional medicinal ingredients other than a narcotic in a quantity of not less than the regular minimum single dose for one such ingredient or one-third the regular minimum single dose for each such ingredient and
(b) there is legibly and conspicuously printed on the Inner label and the outer label, as those terms are defined in section A.01.010 of the Food and Drug Regulations, a caution to the following effect.
"This preparation contains codeine and should not be administered to children except on the advice of a physician, dentist or nurse practitioner
(2) No pharmacist shall sell or provide a preparation referred to in subsection (1) if the pharmacist has reasonable grounds to believe that the preparation is to be used for purposes other than recognized medical or dental purposes
NCR: Definition of Advertisement
Advertisement: any representation by any means hat ever for the purpose of promoting directly or indirectly the sale or disposal of a narcotic
Advertising of a narcotic to the general public is prohibited
NCR: Licensed Dealers
This section contains regulations pertaining to Licensed Dealers
No person except a licensed dealer shall produce, make, assemble, import, export, sell, provide, send or deliver a narcotic
License Dealer (wholesale Manufacturer) may sell/provide (not methadone) to:
another licensed dealer
pharmacist
practitioner
Hospital Employee
person with s.56 exemptions
*Methadone may be sold to all the above except the practitioner unless stipulated in s.56
Regulations in this section outline the requirement that a licensed dealer must meet in order to obtain a license, and outline the requirements they must meet in order to sell '
Regulations in this section pertain to but are not limited to
methods for ordering
information required to place an order
receipts: the licensed dealer must obtain a signed receipt from the purchaser within 5 working days
Purchaser requirements: the licensed dealer is only permitted to sell to persons registered with the Pharmacy Regulatory Authority
NCR: Pharmacist
This section contains regulations specific to Pharmacists
Regulations in this section pertain but are not limited to
receipt of narcotics
sale of narcotics
records of sale
refills of narcotic prescriptions
transcribing verbal orders
loss and theft of narcotics
Protection of narcotics
emergency supply
Destruction of Narcotics
OTC codeine preparations
Loss and Theft (s.42):
"A pharmacist shall report to the Minister any loss or theft of a narcotic within 10 days of his discovery thereof
Emergency Supply (s. 45)
A pharmacist may, on receiving a written order for a narcotic: > (b)sell or provide to another pharmacist the quantity of the narcotic that is specified in the order as being required for emergency purposes, if the order is signed and dated by the other pharmacist
(2) A pharmacist shall, immediately after returning, selling or providing a narcotic under subsection (1) or after receiving a narcotic under paragraph (1)(b) or subsection 65(4), enter the details of the transaction in a book, register or other record maintained for the purpose of recording such transactions...
Receipt of Narcotics
Process of Receipt of Narcotics (s.30)
A Pharmacist who receives a narcotic from a licensed dealer , shall immediately enter in a book, register or other record maintained for such purposes, the following:
Name of quantity of narc received
was it was received
name and address of person it was received from
Sale of a Straight Narcotic (S.31)
A pharmacist may sell or provide a narcotic other than methadone or dried marihuana to a person
if a person is exempted under section 56 of the act with respect to the possession of that narcotic or
If the pharmacist has first received a written order or prescription therefor signed and dated by a practitioner and the signature of the practitioner, where not known to the pharmacist, has been verified by him
Refills (s.37)
A pharmacist shall not use an order or prescription, written or verbal, to dispense a narcotic after the quantity of the narcotic specified in the order of prescription has been dispensed
Record of Sale (s.38)
Where, pursuant to a written order or prescription, a pharmacist dispenses a narcotic, other than dextropropoxyphene or a verbal prescription narcotic, the pharmacist shall forthwith enter in a book, register or other record maintained for such purposes
the name and address of the person named in the order or prescription:
the name, quantity and form of the narcotic;
the name, initials and address of the practitioner who issued the order or prescription;
the name or initials of the pharmacist who sold or provided the narcotic
the date on which the narcotic was sold or provided, and the number assigned to the order or prescription
Prescription Filling (S.40)
"A pharmacist shall maintain a special narcotic prescription file in which shall be filed in sequence as to date and number all written orders or prescriptions for narcotics dispensed and the written record of all verbal prescription narcotics dispensed pursuant to a verbal order or prescription..."
"A pharmacist shall retain in his possession for a period of at least two years any records which he is required to keep by these Regulations"
Narcotic Sales Registry and Filling
Record the amount dispensed on that day only and original Rx #
Typically done with end of day report in your pharmacies computer
All narcotic prescription must be filed separately from regular prescription
if both a narcotic and regular med on 1 Rx, file original with narcotics and a reference in the regular prescription
Receiving Narcotic Orders
shipped separately
invoiced separately
must order using pharmacist narcotic order #
Invoice must be signed and returned by pharmacist
all narcotics must be stored in locked area
…
Request for Destruction of Narcotics
Destruction of Narcotics and Controlled Drugs
Narcotic and Controlled drugs to be destroyed shall receive prior authorization from health Canada and, at the time of destruction, shall be witnessed and documented by two health care professionals
Destruction
Loss reported within 10 days
TLDR excess of a narcotic that was already given to a patient doesn’t need to be witness as long as it is documented
the remainder of an open ampoule, the partial content of which has been administered to a patient, may be destroyed by a licensed health professional without a witness. Such a destruction needs to be documented. As part of the security measures in place and in order to prevent diversions, a hospital may choose to increase this regulatory requirement.
Narcotic and Controlled medication to be destroyed locally, since 2016, do not require prior authorization from Health Canada but at the time of destruction, shall be witnessed and documented by two health care professionals (one must be pharmacist)
Records maintained for 2 years
Reportable Controlled Drugs= Straight Controlled Drugs= Reportable Sales Record
Drugs that are CNS stimulants such as Ritalin or Dexadrine or amphetamines
Repeats allowed on written if indicated # of repeats and time interval
no repeats allowed on verbal prescriptions
no transfers allowed
combinations containing more than one controlled drug
Controlled Drug Regulation
Found under Food and Drug Regulation Part G
Drug labels must have the Rx symbol
Schedule to Part G of FDR has 3 sections
Part I: amphetamines, methylphenidate plus secobarbital and pentobarbital
Part II: barbiturates and their salts and derivative excluding secobarbital and phenobarbital
Part III: anabolic steroids and derivatives
Controlled Drug Preparations= one Controlled Drug + 1 or more medicinal ingredients
not reportable in sales record
repeats on written if authorized in writing the # of repeats and time interval
No repeats on verbal
transfers not permitted
Controlled Drugs: Schedule IV
barbiturates (except secobarbital and pentobarbital) and other controlled including butorphanol
Anabolic Steroids
Repeats on verbal and written allowed if # of repeats & time interval
Transfers not permitted
Example: Phenobarbital, butorphanol
Benzodiazepines and other Targeted Substances
non reportable
filled with regular prescription
repeats allowed
can only be transferred once
Schedule F drugs= Regular Prescription Drugs
refills allowed
non-reportable
verbal and written Rx
Benzodiazepines and Other targeted Substances Regulations
Benzodiazepines and Other targeted Substances Regulations were implemented in September 2000
Symbol on stock bottle
You can still file Rx records with either N/CD or regular
Regulations in this section pertain to, but are not limited to
refills
sales
prescription transfers
Sale to Another Pharmacy
A quantity may be sold to another pharmacist if the other pharmacist states that the targeted substance is required because of a delay or shortfall in an order for the targeted substance (s. 55 (b) )
Refills: are permitted if number of refills is specific, a record is kept of each refill, less than one year has elapsed since the day on which the prescriber was issued by the practitioner (s.52)
Must abide by any intervals notes by the prescriber
Prescription transfer: A pharmacist may transfer a prescription for a targeted substance to another pharmacist, except a prescription that has already been transferred (S.54)
Destruction (s. 2(2).
There is no need to contact the Compliance, Monitoring, and Liaison Division to request destruction of T/C
Quantities to be destroyed must be recorded
Destruction must be witnessed
Pharmacist, practitioner or individual in charge of a hospital may destroy
Exception: remainder of an open ampoule if the partial contents were administered to a patient in hospital
A pharmacist, a practitioner or the individual in charge of a hospital may destroy a targeted substance if
(a) before the destruction, the pharmacist, practitioner or individual records information with respect to the destruction, including the name, strength per unit and quantity of the targeted substance to be destroyed;
(b) the targeted substance is destroyed using a method of destruction that conforms with all applicable federal, provincial and municipal environmental legislation;
(c) the person records the date of destruction;
(d) subject to subsection (3), the destruction is witnessed by a pharmacist or a practitioner; and
(e) immediately following the destruction, the person who destroyed the targeted substance and the witness referred to in paragraph (d) sign and print their names on a joint statement, indicating that they witnessed the destruction and that the targeted substance destroyed has been altered or denatured to such an extent that its consumption has been rendered impossible or improbable.
NAPRA Guidelines
Perpetual inventory
Manual inventory every 3 months or when changing managers
triplicate prescription program
should discrepancies be identified during inventory counts, the manager shall record the incident on an "incident report" and keep a record at the pharmacy. The manager shall initiate the necessary steps to identify the cause of the shortage, the responsible staff person and the initiate corrective actions. Significant shortages or diversion incidents must be reported to the M.Ph.A. and Health Canada.
Where a patient reports a shortage in their prescription, the inventory control system would verify or refute the shortage. If the prescription is re-dispensed, documentation of the date, time and reason for re-dispensing shall be noted on the prescription and cosigned by the manager and, except in sole practice situations, one other pharmacist.
When a breakage occurs, a report shall be filed on the pharmacy records of perpetual inventory, as a negative quantity. Documentation of the date, time and place of breakage could be co-signed by the manager and, except in sole practice situations, one other pharmacist.
NB Narcotic and Controlled Drug Storage Guidelines
If significant quantities of narcotic or controlled drug products are kept on hand, the bulk of these products should be kept in a safe or locked cabinet.
Narcotic or controlled drug products that are stored in open shelf areas should be dispersed with regular prescription inventory, rather than in one localized shelf area.
The intent of this directive is to prevent or minimize the loss of a significant quantity of product and increase the time necessary to collect the product in the event of a robbery, while not endangering staff faced with such a situation.
This directive does not prevent a pharmacy from choosing to store all narcotic and controlled drug products in a safe or locked cabinet.
CDSA Controlled Drugs and Substances
the controlled drug and substance act is a federal law
applies to the handling of controlled substances in Canada
Loss or theft: reports of any loss or theft of controlled substance or precursors must be submitted to health Canada Office of Controlled Substances (OCS)
Reports of any loss or theft of controlled substances or precursors must be submitted to Health Canada's Office of Controlled Substances (OCS).
Post-Consumer Returns
Post-consumer returns must be received by a pharmacist, pharmacy intern, or pharmacy technician.
Post-consumer returns must be stored in a one way entry container that has a unique identifier. It is recommended that the container is also opaque, inconspicuous and tamper evident.
Containers must be kept in the pharmacy dispensary when in active use and access should be limited to pharmacy staff. Should there be limited space inside the dispensary, the containers may be placed outside of the dispensary as long as they are in plain sight of the pharmacy staff and secured to the floor.
Pharmacists are also encouraged to use other means to enhance security in and around the dispensary area, such as the installation of security cameras.
Post-consumer returns must be received by a pharmacist, pharmacy intern,
or pharmacy technician.Pharmacists are not required to send destruction requests to Health Canada in order to proceed with local destruction.
Pharmacists performing local destruction must follow all applicable municipal, provincial and federal environmental laws and the destruction must render the controlled substances unusable.
Pharmacists should be aware that the destruction process may vary from substance to substance depending on the chemical or physical properties of the substance in question, however a change of state is recommended (i.e., from solid to liquid).
Pharmacists are encouraged to consult Workplace Hazardous Materials Information System (WHMIS) sheets or their respective provincial regulatory colleges for instructions on the appropriate method of destruction of controlled substances.
Once subjected to local destruction, post-consumer returns may be placed in an appropriate container and disposed of in a manner that is safe, environmentally responsible, secure and compliant with legal and professional requirements to protect confidential patient information. Already denatured products need not be sent to licensed dealers for disposal and can be placed in the regular pharmaceutical waste.
All local destructions must be witnessed by a practitioner, pharmacist, a pharmacy intern, or a pharmacy technician.
Pharmacists carrying out local destruction of post-consumer returns must record the date the destruction took place, the unique identifier of the container and the number of containers destroyed.
Records for the local destruction of post-consumer returns should be kept separate from those for post-consumer returns being sent to a licensed dealer.
The generated record must be signed by the pharmacist who carried out the destruction
and the witness present. The destruction must be witnessed in duplicate by the individual
destroying the substances and any other practitioner, pharmacy intern, or pharmacy
technician. Both persons must sign and print their names on the generated record and
indicate that they witnessed the destruction and that the substance was altered or
denatured to such an extent that its consumption was rendered impossible or improbable.This information must be recorded in a register similar to that required to be kept for
orders involving narcotics, controlled drugs and targeted substances, and must be
retained for a period of at least two years, in a manner that permits an audit to be made
35 day Regulation
A pharmacist shall dispense no more than a thirty five-day supply of narcotics, controlled drugs or benzodiazepines to any client. This does not apply to drugs indicated for and being used for the prevention and/or treatment of seizure disorders. Where the signa on the prescription is not clearly defined with respect to days’ supply, the pharmacist shall dispense no more than thirty-five doses.
A pharmacist may dispense more than a thirty-five-day supply of medication provided that (a) in the member’s professional judgement it is safe to do so; and (b) the prescriber has specified the exact quantity to be dispensed in excess of the thirty-five-day limit and has stated a reason for ordering that quantity.
NBCP- Regulations: https://nbpharmacists.ca/wp-content/uploads/2023/02/2022-REGS-bilingual-Nov-2022-Formatted.pdf?x43718
Definitions
Act: means the NB Pharmacy Act
ACPE: means the Accreditation Council for Pharmacy Education
Apprentice: means a registrant in a conditional register or a student (pharmacist or technician) who has entered into training with a preceptor in order to become a pharmacist or pharmacy technician.
Biologicals: means medicinal preparations made from living organisms and their products, which include, but are not limited to serums, vaccines, antigens, antitoxins.
CCAPP: means the Canadian Council of Accreditation of pharmacy programs.
Child resistant container: means a container that meets the Canadian Standards Association standards for child resistant containers
Close supervision: means supervision requiring direct contact with the supervised individual (member, employee) in person for most of the work period at the workplace.
Collaborative practice: means a practice setting in which a member works closely and cooperatively with one or more health professionals.
Collaborative practice agreement: means a written agreement between a pharmacy tech or pharmacists, and one or more health professionals.
Device: means any article, instrument, apparatus or contrivance, including any component, part or accessory thereof, manufactured, sold or represented for use in
The diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals
Restoring, correcting or modifying a body function or the body structure of human beings or animals
The diagnosis of pregnancy in human beings or animals
The care of human beings or animals during pregnancy and at and after birth of the offspring, including care of the offspring
And includes a contraceptive device but does not include a drug
Dispensary: means the area of a pharmacy where
drugs listed in Schedule I and II are stored for sale and/or prepared for dispensing.DIS/PMP: means the provincial drug information/prescription monitoring program.
Drug preparation activities: means reconstituting, diluting or otherwise preparing a drug or combining, admixing or mixing together two or more substances, at least one of which is a drug, to create a final product for the purpose of the sale or provision to another person, other than pursuant to or in anticipation of a prescription
Drug preparation premises: means any place where drug preparation activities take place
under the supervision of a pharmacist which complies with a regulatory framework in that jurisdiction but does not include:(a) a pharmacy in respect of which a certificate of operation has been issued by the regulatory body for that jurisdiction;
(b) a premises in respect of which a valid establishment license has been issued under the Food and Drug Regulations to the Food and Drugs Act (Canada)
Electronic signature: means an electronic sound, symbol, or process attached to or logically associated with a record and executed or adopted by a person with the intent to sign the record. The signature may also be “stylus on screen”. Reproduced images (jpeg, etc.) of signature are not acceptable.
Electronic transmission: of a prescription means communication of an original prescription or refill authorization by electronic means, to include computer-to computer, computer-to-facsimile machine, facsimile machine to facsimile machine, facsimile machine to computer or e-mail transmission which contains the same information it contained when the authorized prescriber transmitted it, but does not include a telephoned order
General supervision: means supervision requiring direct contact with the supervised individual (e.g. member, employee) in person at least monthly with supervision available as needed by other methods.
Pharmacist: Direct Client Care” means a pharmacist in active practice that had direct contact with clients for at least 400 hours during the preceding two-year period
Non-Direct Client Care” means a pharmacist in active practice who does not meet the criteria of a Pharmacist –Direct Client Care (e.g. pharmacists in administrative, management or other nondirected client care positions)
Pharmacy Technician: Direct Client Care” means a pharmacy technician in active practice, under the supervision of a Pharmacist – Direct Client Care, for at least 400 hours during the preceding two-year period
Non-Direct Client Care” means a pharmacy technician in active practice who does not meet the criteria of a Pharmacy technician – Direct Client Care (e.g. pharmacy technicians in administrative, management or other non-direct care positions). Definitions continued
PRA: means a Pharmacy Regulatory Authority of a Canadian province or territory
Preceptor: means a member who
(a) is a member in good standing;
(b) is registered to practice pharmacy in a location approved by Council;
(c) has been registered for a minimum of one year with the College;
(d) has no restrictions on the right to practice; and
(e) meets the requirements of section 12.23
Record: means the records of a pharmacy, whether in written, photographic, magnetic, electronic or other form, and includes, without limitation
(a) the records of the proprietor of the pharmacy, the manager, the regulated members engaged by the proprietor or any other person associated with the pharmacy;
(b) any record required to be kept under the Act, the Controlled Drugs and Substances Act (Canada) or the Food and Drugs Act (Canada) or the regulations or standards under those acts
(c) a record of all prescriptions the pharmacy receives, including an identification of the prescriptions that the pharmacy transfers to another pharmacy or pharmacist;
(d) a record of all drugs dispensed from or through the pharmacy, including the prescription, the name of the drug, the amount dispensed, the name and contact information of the client and the name and contact information of the prescriber;
(e) a record of the pharmacy services provided, including the name of the person or persons who dispensed a drug, or provided a pharmacy service;
(f) a record of the names and contact information of the clients to whom pharmacy services are provided; and
(g) a record of the counselling services provided to a client
Registrant: means a person whose name is entered on any register
Routine supervision: means supervision requiring direct contact with the supervised individual (e.g. member, employee) in person at the work site at various times throughout the work period with indirect contact occurring by other methods, such as telephone or written communication.
Supervision: as defined in the Act, includes close supervision, routine supervision or general supervision, as the case may be
Part II Council
Council shall consist of:
Voting councilors, being:
(i) the President,
(ii) the immediate past-president, or a former president appointed by Council if the past-president is unable or unwilling to serve,
(iii) seven elected pharmacists,
(iv) two elected pharmacy technicians
(v) three lay representatives appointed by the Minister
non-voting councilors, as appointed by Council, who may participate in debate, but are not entitled to vote on any matter before Council, being:
(i) at least one representative of a school of pharmacy
(ii) “ex officio” representatives in the number determined by Council, who shall serve for terms set by Council and at the will of council
Disqualification
2.2 The following persons are disqualified from being councilors:
(a) a person who is less than 19 years of age
(b) a person who is of unsound mind and has been so found by a court in Canada or elsewhere;
(c) a person who is not an individual;
(d) a person who is on the staff of the College
(e) a person who has the status of bankrupt;
(f) a member on a conditional register;
(g) a person convicted of an offence under
(i) the Criminal Code of Canada,
(ii)the Narcotic Control Act (Canada),
(iii) the Food and Drugs Act (Canada),
(iv) the Controlled Drugs and Substances Act, or
(v)the criminal law of any jurisdiction outside of Canada
Members of Council
2.3(1) Pursuant to section 7 of the Act, the
membership shall elect to Council, for two year terms commencing at the conclusion of the annual general meeting
(a) seven pharmacists; and
(b) two pharmacy technicians. 2.3(2) Pursuant to section 8 of the Act, the
Minister shall appoint three lay representatives, for a three-year term commencing at the close of the annual general meeting following their appointment, and may be re appointed for one additional term. (2016)
2.3(3.1) Each elected councilor ceases to hold office at the close of the second annual general meeting following the councilor’s election. (2016)
2.3(3.2) Each lay representative ceases to hold office at the close of the third annual general meeting following the councilor’s appointment. (2016)
2.3(4) No pharmacist or pharmacy technician may be elected to more than five consecutive terms on Council
2.3(5) Presidents, Presidents-Elect or Past Presidents who complete five consecutive terms on Council shall remain on Council until each completes their term as Past-President, resigns or becomes otherwise disqualified. (2018)
Officer and Duties
3.3(2) The President-Elect shall assume the office of President commencing at the end of the preceding President’s term of office
3.3(7) The President-Elect shall:
(a) be vested with all the powers and perform all the duties of the President in the absence, disability or refusal to act of the President;
Removal from office
3.4(1) Any five councilors may seek the removal from office of the President or President-Elect by delivering to the Registrar a notice in writing stating the reason for the proposed removal.
3.4(2) The Registrar shall, upon receipt of such notice, deliver a copy of the notice to the President or President-Elect affected.
3.4(3) Council may, after being satisfied that reasonable notice has been given under subsection 3.4(2), and by the vote of two thirds of those councilors present and eligible to vote on the matter, remove the President or President-Elect from office
Meeting of Council
4.1 Council shall hold at least three meetings annually, one of which is held at the conclusion of the Annual General Meeting.
4.2(1) Meetings of Council may be called from time to time by the order of the President or at the written request of three or more councilors to be held at any convenient place
4.2(2) Notice of meetings of Council shall be delivered by e-mail, by facsimile, electronically or by any other generally accepted means by the Registrar to each member of Council not less than one week before the time appointed for such meeting.
4.2(3) Meetings of Council may be held from time to time without formal notice if all councilors are present, or those absent have signified their consent to such meeting being held in their absence
4.3 The accidental omission to give notice of a meeting to any councilor or the nonreceipt of the notice by any councilor does not invalidate anything done at the meeting.
4.4 A meeting of Council may be held in person, by conference call, video conferencing or other method that ensures that the councilors all have the opportunity to participate in the meeting
4.8 Council shall maintain a policy on the use of in camera for all, or parts, of a meeting
Council members only;observers have to leave
Part V Committees
5.1(1) Council may appoint standing and special committees in addition to those committees required by the Act.
5.1(2) Committees may select their respective Chair unless determined otherwise by legislation, or by Council.
5.1(3) Those serving on Committees need not be members of the College.
5.1(4) Council shall approve Terms of Reference for all committees
Finance Committee
5.2 Council shall appoint a Finance Committee responsible for advising Council on matters pertaining to finance, including budgets, internal controls, investments, staff compensation, and any other matter designated by Council
Continuous Professional Development Committee
5.3 Council shall appoint a Continuous Professional Development Committee to guide and ensure that members registered to practice pharmacy maintain and improve their skills and knowledge base on an on-going basis
Governance Committee
5.4 Council shall appoint a Governance Committee to monitor the functioning of
Council, develop governance policies and ensure policies are followed
Registration Committee
5.6 Council shall appoint a Registration Committee to assess applications for membership and establish requirements that applicants must meet to be entered on a register.
5.7(1) If the term of a Registration Committee member expires before the Committee
concludes a matter before it, the Committee member whose term has expired shall
continue to be a member of the Committee until the matter is concluded by the Committee
Inquiries
5.8 At the request of the Registrar, the Registration Committee shall inquire into
(a) an application for enrolment as a member;
(b) an application for reinstatement in the College by a former member; and
(c) an application for transfer by a member from one register to another
Refusal
5.16 The Registration Committee may direct the Registrar to refuse to issue a certificate and/or registration to, or enter on a register, any applicant who
(a) has been the subject of a decision of a Canadian court finding the applicant guilty of a criminal offence which, in the reasoned opinion of the Registration Committee, is related to the practice of the profession, unless the applicant has obtained a pardon;
(b) has been the subject of a decision of a foreign court finding the applicant guilty of an offence which, if committed in Canada, could have led to criminal proceedings and which, in the reasoned opinion of the Registration Committee, is related to the practice of the profession, unless the applicant has obtained a pardon;
(c) has been the subject of a disciplinary decision by a Complaints or Discipline and Fitness to Practice Committee of another regulatory body, imposing the revocation of a certificate and/or registration; or
(d) has been the subject of any other matter deemed to be significant by the Registration Committee
Restriction or Suspension
5.17 The Registration Committee may direct the Registrar to enter an applicant on a register, but restrict or suspend the applicant’s right to engage in professional activities, if that applicant
(a) is the subject of a disciplinary decision made by the Complaints Committee or the Discipline and Fitness to Practice Committee;
(b) does not meet all of the established criteria for suspension
Restriction or Suspension
(c) is the subject of a disciplinary decision made outside New Brunswick which, if made in New Brunswick, would have had the effect of a restriction or suspension of the right to engage in professional activities imposed by the Complaints Committee or Discipline and Fitness to Practice Committee;
(d) is or has been, as the case may be, the subject of a decision described in section 5.16; or
(e) requests restrictions on, or suspension of, the applicant’s registration
Part VI-Codes of Conduct
Governance
6.1(1) The Governance committee is responsible for developing, and monitoring compliance with, a Code of Conduct (including conflict of interest) and procedures for councilors and of Committees
6.1(2) All councilors, officers and committee members shall exercise the powers and discharge the duties of their office honestly, in good faith, and in the best interest of the College in accordance with the approved Code of Conduct, and in connection therewith shall exercise the degree of care, diligence and skill that a reasonably prudent person would exercise in comparable circumstances.
6.1(3) Each councilor, committee member and office staff shall conduct himself or herself with utmost integrity and professionalism and ethically in relations with the public and……
Conflict of Interest
6.2(1) Council shall ensure a Conflict of Interest policy (part of Code of Conduct) is in place.
6.2(2) Each councilor shall review the Conflict of Interest Policy at least once per year and shall affirm that they have reviewed the policy by completing and signing a conflict-of-interest policy agreement form designated by Council.
6.2(3) A councilor shall abstain from voting or attempting to influence the vote on any matter before Council that places him/her in a conflict of interest.
6.3 Members and managers shall avoid conflicts of interest in their practice
6.4 Subject to section 6.5, a manager or pharmacist is in a conflict of interest,
(a) where a reasonable person knowing the relevant facts would conclude or perceive that the action of the pharmacy in relation to the provision of services was adversely influenced or would likely have been adversely influenced by the financial interests of the pharmacy or of a related person or a related corporation
(b) where the pharmacy or a related person or a related corporation enters into an arrangement or agreement which a reasonable person knowing the relevant facts would conclude or perceive would likely have the effect of adversely influencing the exercise of a member’s professional judgment or influencing or impeding a member’s ability to engage in the practice of pharmacy in an ethical manner or in accordance with the standards of practice of the profession
c) where the pharmacy or a related person or a related corporation enters into an arrangement or agreement which a reasonable person knowing the relevant facts would perceive as directly or indirectly influencing or encouraging a prescriber to promote the use of the pharmacy by a client; or
(d) where the pharmacy or a related person or a related corporation
(i) accepts or receives a benefit by reason of the referral of a client to any other person,
(ii) offers or confers a benefit to a person by reason of the referral of a client to the pharmacy, or
(iii) offers or confers a benefit including but not limited to loyalty programs or redeemable incentives to a client in relation to the sale of a drug referred to in Schedule I or the provision of professional pharmacy services other than
(A) an adjustment in the fee or amount that would otherwise be charged by the pharmacy with regard to that client for that drug or that professional pharmacy service, or
(B) the provision to a client, at no charge, of an item of a nominal value, to be used in maintaining or promoting well-being or health.
Professional Misconduct
6.7 In addition to those activities enumerated in the Act, professional misconduct includes, but is not limited to, the following:
(a) contravening, while engaged in the practice of pharmacy, any federal or provincial law or regulation with respect to the distribution, sale or dispensing of any drug or mixture of drugs;
(b) breach of the Code of advertising;
(c) practicing without maintaining the required professional liability insurance;
(d) failing to pay the appropriate fees to practice pharmacy;
(e) engaging in a conflict of interest;
(f) failing to maintain the Standards of Practice of the profession;
(g) failing to respond to a communication from the Registrar (or designate), or the Administrator of Complaints;
(h) refusing to allow an appointed person to enter at a reasonable time the pharmacy in which the member is engaged in the practice of pharmacy for the purpose of an inspection;
(i) displaying a lack of knowledge, skill or judgment, or disregard for the welfare of the public of a nature or to an extent that demonstrates a member is unfit to carry out the member`s responsibilities; (2017)
(j) selling or dispensing an excessive or unreasonable or improper amount of a drug;
(k) abusing a client, verbally, emotionally, or physically;
(l) discontinuing professional services that are needed, without reasonable cause, unless
(i) the client requests the discontinuation,
(ii) alternative services are arranged, or
(iii) the client is given a reasonable opportunity to arrange alternative services
(m) breaching an agreement with a client relating to professional services for the client, or fees for such services;
(n) falsifying a record in respect of a prescription or the sale of a drug;
(o) sharing fees with a person who has referred a person to a member or to a pharmacy or receiving fees from a person to whom a member has referred a person
(p) participating in a lease of premises for a pharmacy that permits a person other than a member or the owner of the pharmacy to participate in the revenue of the pharmacy except by way of a rent normal for the area in which the premises are located;
q) knowingly submitting a false or misleading account or false or misleading charge for a drug, the compounding of a drug product or dispensing of a prescription;
(r) signing or issuing a certificate or similar document that contains a statement the signing or issuing member knows or ought to know is misleading;
(s) announcing or holding out by a member that the member has special qualifications that are not in fact possessed by the member;
(t) except as specifically permitted in these Regulations, returning to stock or again selling or dispensing a drug previously sold or dispensed and delivered, or a medication sample, or outdated pharmaceutical products
(u) using improperly the authority to sell or dispense a drug or mixture of drugs;
(v) acting as a member while the ability to perform an action as a member is impaired by any substance;
(w) knowingly permitting the premises in which the pharmacy is located to be used for unlawful purposes;
(x) permitting, consenting to or approving either expressly or by implication the commission of an offence under the Act or these Regulations by another person associated with the pharmacy in which the pharmacist practices;
(y) falsifying a record, or failing to maintain the records that are required to be kept respecting clients
z) purchasing a drug other than from a legally authorized source;
(aa) disclosing of information relating to selling or dispensing of drugs to a person other than the person to whom the drugs are sold or dispensed, other than as required by law or these Regulations or with the consent of the person to whom the drugs are sold or dispensed;
(bb) providing a prescriber with prescription blanks which are imprinted with the name of a pharmacy; and
(cc) engaging in conduct, or performing an act, relevant to the practice of pharmacy that, having regard to all the circumstances, would reasonably be regarded by members as disgraceful, dishonorable or unprofessional
Fees
7.1 Council shall establish a dues and fees schedule which shall have force only after the same has been approved, with or without amendment, by majority vote at an annual or special general meeting of the College. (2016)
7.2(1) Every member shall pay the membership fees for the category of membership of the member on or before November 30 in each year, unless otherwise specifically provided
7.2(2) Every member who fails to pay the required fees by November 30 shall also pay to the College an additional late payment fee as specified in the fee schedule, by December 31 of the same year. (2016)
7.2(3) A member who has not paid the applicable fees in any year is suspended from practice on January 1st of the following year, and may be removed from the register
7.3 The manager is responsible for ensuring the annual renewal fee for the certificate of operation is paid by November 30 in each year. Every pharmacy who fails to pay the required fees by November 30 shall also pay to the College an additional late payment fee as specified in the fee schedule, by December 31 of the same year. (2016)
7.4 If any of the fees and dues owed by a pharmacy are not paid on or before December 31 of any year in which they are due,
(a) the pharmacy and the manager may be removed from the applicable register; and
(b) the certificate of operation shall be considered lapsed and the pharmacy shall cease to conduct business immediately
Part IX Registers
Active Pharmacist Direct Client Care
Active Pharmacist Non-Direct Client Care
Non-active Pharmacist
Retired Pharmacist
Active Pharmacy Technician Direct Client Care
Active Pharmacy Technician Non-Direct Client Care
Conditional Register
Non-active Pharmacy Technician
Retired Pharmacy Technician
Pharmacist Student
Pharmacy Technician Student
Retired Certified Dispenser
Life member
Emergency
Register Information
11.4 In addition to information required by the Act, all registers must contain the following information with respect to the member:
(a) the member’s name as it is given on the person’s birth certificate, subject to any change in this name supported by documentation under the Change of Name Act or through the amendment process of the Vital Statistics Act, or equivalent in the Province of New Brunswick or equivalent in another Canadian jurisdiction; (2015)
(b) the address at which the registrant ordinarily resides;
(c) date of birth;
(d) gender
(e) telephone number;
(f) email address;
(g) place of employment;
(h) a notation and date of the retirement from practice or death of a member
(i) registration number;
(j) expiry date of the annual license;
(k) the type of registration issued to the member;
(l) a notation of every voluntary surrender or cancellation of a registration, and the date of surrender or cancellation; and
(m) a notation of every reinstatement and the date of reinstatement.
Duty to Notify the Registrar of Changes to information
11.5 A registrant shall notify the Registrar of any change to information required to be on the register.
11.6 In addition to any information required by the Act, the member must also provide the following information:
(a) all verdicts and recommendations of a coroner’s inquest involving the member;
(b) denials of registration by professional regulatory colleges and denials of membership by professional associations that have regulatory responsibility
Information made available to the public
11.7 The following information contained in a register is considered to be public knowledge
(a) registration number;
(b) person’s name; (2015)
(c) the register in which the person is listed;
(d) whether the person is authorized to administer injections, assess minor ailments or provide other specialized services; (2015)
(e) whether the person is engaged in a collaborative practice agreement; (2015)
(f) results of proceedings from any Complaints Committee or a Discipline and Fitness to Practice Committee hearing where a person has been found to be at fault, for a period of two years;
(g) a notation indicating that a person’s registration has been suspended or revoked; notation remains on the register for five years; and
(h) a notation indicating that a person’s registration has been suspended or revoked for sexual misconduct; notation remains on the member’s file indefinitely, without limitation
Part XII Registration
12.1 All applicants for registration must:
(a) be of good character;
(b) complete an application in the form established by Council;
(c) pay to the College the fees provided for in the fee schedule;
(d) provide evidence that he or she:
(i) is a Canadian citizen, landed immigrant or holds a valid employment visa or valid Canadian work permit;
(ii)is a graduate of a CCAPP or ACPE accredited program, in Canada or the United States, or is authorized to practice pharmacy in another Canadian jurisdiction;
(iii) has passed any examinations or assessments that Council may require
(iv) has served a period of internship as determined by the Registration Committee;
(v) has successfully completed a structured practical training program approved by Council;
(vi) has insurance, as required by Part XXV of these Regulations;
(vii) is proficient in one of the official languages of New Brunswick;
(viii) has knowledge, to the satisfaction of the College, of the Act, Regulations, the Code of Ethics and Standards of Practice and practice directives applicable to the practice of pharmacy in New Brunswick, relevant to the members registration, and provide an undertaking that he will conform to these in practice
(ix) is currently practicing in a direct client care setting if the applicant is requesting admission to a Direct Client Care register; and
(x)meets any other requirement specified for registration in the
applied to register;
(e) disclose by declaration whether he or she
(i) is currently suspended as a result of professional misconduct, or as the result of an allegation of professional misconduct, by a PRA in Canada or elsewhere, or, if the applicant has been so convicted, provide evidence satisfactory to the Registration Committee showing effective rehabilitation
(ii)has been convicted of an offence or been subject to professional discipline which could make the applicant unsuitable for registration as a member;
(iii) is, or has been, the subject of a judicial or disciplinary decision referred to in sections 5.16 or 5.17
(iv) has dependence to alcohol, drugs or other substances;
(v) has an ongoing medical condition (including substance abuse or dependence) of which he or she is aware and knows, or ought reasonably to know, adversely affects the ability to competently and safely practice pharmacy, or which could make the applicant unsuitable for registration;
(vi) has any pending complaint or disciplinary action; or
(vii) complies with the recency of practice requirements in section 12.30; and
(f) supply:
(i) an identification photograph or electronic image issued by a government of a Canadian jurisdiction; and
(ii) a criminal record check (Canadian federal and provincial) effected within the previous six months
(iii) evidence of current First Aid and CPR certification for registration and licensure on an Active: Direct Client Care register.(2021)
Conditional Registers
12.5(1) The following registrants may be entered on a conditional register
(a) Current members with conditions imposed by the College;
(b) International pharmacy graduates (pharmacists and pharmacy technicians);
(c) Registrants pursuing postgraduate training in a formal educational program;
(d) Registrants pursuing a training program not associated with an educational institution;
(e) Members who have conditions resulting from Complaints or Discipline and Fitness to Practice proceedings. (2022
Rights of Conditional Registration
12.7 Where a person is entered on the conditional register, he or she may:
(a) conduct the practice of pharmacy only in accordance with any conditions imposed; and
b) except as set out in section 12.8, exercise all the other rights and privileges of a member
Pharmacy Technician Students
12.19(1) A pharmacy technician student shall register with the New Brunswick College of Pharmacists as a "registered pharmacy technician student" prior to the commencement of any employment and shall not hold themselves out to be other than a registered pharmacy technician student. Pharmacy technician students shall not hold themselves out to be pharmacy technicians/assistants. (2015)
12.19(2) Pharmacy technician students may only provide pharmacy services while under the supervision of an authorized preceptor
12.19(3) Pharmacy technician students must complete a minimum of 14 weeks of practical training, under the supervision of a preceptor, consisting of:
(a) a minimum of eight weeks in a structured practice experience program similar to that for pharmacists as defined in “A Framework for Assessing Canadian Pharmacists’ Competencies at Entry-to Practice through Structured Practical Training Programs” as published by NAPRA, in a direct client care setting in a community pharmacy or hospital pharmacy, or other location approved by Council
(b) a minimum of 6 weeks, which shall be completed in New Brunswick after graduation; and
(c) successful completion of a Structured Practical Evaluation (SPE) as part of the 6 week post-graduate training period, one component of which requires the pharmacy technician student to accurately apply an independent double check to 500 prescription/ orders/ products for final release with 100% accuracy, an activity which allows for a maximum of 50 items per day. (2016)
12.19(4) During a period of internship, a Pharmacy Technician Student must be assigned to a preceptor, who, as the Pharmacy Technician Student’s preceptor, shall ensure that the Pharmacy Technician Student is exposed to areas of the practice of pharmacy relevant to the internship, including:
(a) maintenance of the client medication profile, evaluation of therapy (for example: duplication, adherence), evaluation of new prescriptions, and resolution of potential and existing problems
(b) accurate dispensing of medication according to the prescription;
(c) assistance to the client on the use of medical devices;
(d) communication with clients and/or health professionals regarding drug and health information;
(e) compliance with all legal requirements associated with the distribution of drugs and the operation of a pharmacy;
(f) provision of information and/or referral services in emergencies, and upon request
(g) development and exercise of appropriate professional judgment;
(h) knowledge of, and compliance with, ethical and professional Standards of Practice;
(i) any other areas established by Council. (2015)
Pharmacy technician students becoming pharmacy technicians
12.20 A pharmacy technician student may apply to be a registered pharmacy technician provided all the requirements in section 12.1 and the requirements provided in section 12.19 are met. An educational program having provisional CCAPP or ACPE accreditation in Canada or the United States will be considered to be accredited for the purposes of this section. Pharmacy Technician Students qualifying under Section 12.3 may apply meeting the requirements of Section 12.1 with the exception of subparagraph 12.1(d)(ii), and meeting all requirements of Sections 12.19 and 12.3. (2015) (2019)
Time Limits
12.21 A person applying for registration and licensure who has graduated from an accredited pharmacy program must be registered and licensed with the College within three years of completing the program and within three years of successfully completing PEBC examinations. (2020)
Apprenticeship Agreement
12.22(1) Every person before commencing training with a preceptor shall:
(a) be registered with the College either as a conditional registrant or a student;
(b) enter into an apprenticeship agreement in the form established by Council; and
(c) forward the signed agreement to the College and receive confirmation from the College that the preceptor meets all requirements provided in subsection 12.23(1). (2021)
Preceptor Qualifications
12.23(1) A member, in order to serve as a preceptor, must meet the following requirements:
(a) be a member who practices in New Brunswick for at least 18 hours a week; (average a year)
(b) have been licensed and practicing in New Brunswick for at least one year;
(c) meet the training requirements of the College by either completing a preceptor training program approved by the College, or meeting the requirements to be a preceptor for the structured practical experiential program (SPEP) in the curriculum of an accredited pharmacy education program;
(d) practice in a pharmacy that meets the SPEP Practice Site Criteria established by the educational institution, or at a location approved by Council;
(e) confirm that the apprentice is properly registered with the College
(f) ensure that any apprentice engaged in practice experience has the level of personal supervision or direction that, in the professional judgment of the preceptor, is required to ensure safe and effective client care given the knowledge, skills and experience of the apprentice; and
(g) not have or be perceived by the College to have a conflict of interest or bias with respect to the apprentice they are supervising. (2021)
A preceptor may not:
(a) have any terms, conditions or limitations on his/her certificate of registration and license other than those applicable to all members of that register unless otherwise authorized by the Registration Committee;
(b) have been found to have committed an act of professional misconduct or to be incompetent by the Discipline and Fitness to Practice Committee within the last six years;
(c) have been found to be incapacitated by the Complaints Committee within the last six years
(d) have been the subject of allegations of professional misconduct or incompetence that have been referred to, but not yet decided upon by, the Complaints Committee, or the Discipline and Fitness to Practice Committee
Duration of Registration of Students
12.24(1) The registration of a student (pharmacist and pharmacy technician) shall be revoked by the Registrar if:
(a) the student is registered on another register;
(b) prior to graduation the student ceases to be enrolled in their pharmacy education program; (2015)
(c) the registration is cancelled under Part X of the Act;
(d) the student has otherwise failed to comply with the provisions of the Act or the Regulations
12.24(2) Where a student’s registration is revoked, the student must obtain the permission of Council before reapplying for registration. Council, on application to it by the student, may at its discretion order that the registration of the student be re-instated.
12.24(3) The registration of a student (pharmacist and pharmacy technician) who does not become a member expires one year from the date of graduation, unless an extension is granted by the Registration Committee. (2016; 2017)
Application not Approved
12.29 If an application for registration or conditional registration is not approved, or approved subject to conditions, the applicant must be notified in writing, with reasons for the decision, and advised of the right to appeal the decision to Council.
Change of Workplace or Practice
12.31 A member who changes place of employment for more than 30 consecutive days shall notify the College by updating their member profile within seven days of the change
Pharmacies
Pharmacies are required to register as either community or institutional.
In the registration the pharmacy needs to include:
Name of the pharmacy,
Name(s) of the person(s) who conduct business,
Name of the manager who holds the certificate of operation
Address, telephone number and fax number of the pharmacy
Email addresses of manager and the pharmacy
Certificate of operation number
Initial date and end date of registration and operation
Pharmacy related website address(s)
Owner’s name, phone number and email address
Certificate of Operation
Before a pharmacy can operate it must apply for a certificate of operation at least 30 days prior to operation.
In order to receive a certificate of operation, the pharmacy must provide to the registrar
A completed application form
Demonstrate that the pharmacy will be staffed and managed by members capable of operating a pharmacy
Operate a sufficient number of hours per week to meet the needs of the community
Have internet access for email and research purposes
Be connected to and share information with DIS/PMP
Have a quality management process in place
Meet all requirements related to the practice of pharmacy as described in the application, established by Council in policy or practice directive
Restriction on Operation
N.B.: Council has yet to declare into force section 13.6
13.6(1) A pharmacy may be granted a certificate of operation as offering a specialized type of service.
13.6(2) The pharmacy’s practice is then restricted to the type(s) of service stated on the certificate.
13.6(3) Nothing prevents a pharmacist in a specialized pharmacy from providing care where there is an urgent situation and it is required to meet the needs of clients
Certificates of Operation
N.B.: Council has yet to declare into force section 13.7
13.7 The following categories of certificates of operation are established:
General
Central fill
Mail order
Clinical practice
Satellite pharmacy
Methadone
Specialty compounding
Pharmacy education facility
Correctional service
Nursing home
Hospital
Natural Health/Alternative Care and
Limited service, other
Pharmacy Standards of Operation
Pharmacies that provide direct client care service to the public
are required to:Be accessible to the public in person and by telephone,
Designed to discourage entrance to the dispensary area by unauthorized persons but still encourage and facilitate discussion between client and pharmacist
equipped with a private consultation area where clients may be counselled and their treatment discussed without being overheard by the public, or other staff. (2022)
Quality Management
14.2 The manager must ensure and document ongoing quality management including, but not limited to: evaluating staff performance, equipment and facilities and adherence to Standards of Practice including the following
(a) as of January 1, 2019, anonymous medication error reporting to an external Canadian database for errors that reach patients;
(b) response to individual errors and trends
(c) maintenance of a culture of safety within the practice
(d) provisions to protect the confidentiality of information relating
to clients. (2018) Quality Management
Information to be posted in Pharmacy
The following items are to be displayed in or near the dispensary where clients can view:
Certificate of Operation
Certificate of Registration and annual license of pharmacists, pharmacy technician and any students
Hours of operation
A condensed version of the Code of Ethics; (2022)
Any other information required by Council to be made available for the purpose of informing the public about the practice of pharmacy
Presence of Pharmacist
14.16(1) When the dispensary and the professional service area are open and accessible to the public and Schedule III drugs are displayed, a pharmacist shall be present in the pharmacy. (2022)
After hours, staff may be present in the dispensary to perform limited tasks such as inventory control, generating prescription labels, replenishing drug stock, 3rd party billing etc. No activities that require the presence of a pharmacist may be performed
Security
Every member while on duty is responsible for the security of the pharmacy. The member should protect against unauthorized entry, theft or diversion of medication.
After hours, the pharmacy should be secured with suitable security measures such as locks, alarms, cameras to prevent and detect unauthorized entry
Prescription Dispensing and Records
A prescription may be filled or refilled up to one year from the date issued unless cancelled by the prescriber.
No person except a member within their scope of practice, shall:
Sell a scheduled drug
Prepare written copies of a prescription
Provide or receive verbal copies of a prescription
Assess and approve a prescription for filling or refilling
Receive and record a verbal prescription from a prescriber
Educate a client about a drug and their drug therapy
Adjusting Quantity
A member may in consultation with a client adjust the quantity of the drug to be dispensed when:
The client request a different quantity and its appropriate to do so,
The manufacturers standard package size does not match the prescribed quantity, (boxes do not have to be opened)
The quantity exceeds the amount covered by the client’s drug plan,
A trial quantity is authorized by the client,
The member consults with the prescriber and documents the consultation,
Poor compliance history,
Drug misuse suspected,
The safety of the client is in question due to potential for drug overdose
35 Day Supply Regulation
17.5(2) Subject to subsection 17.5(4), a pharmacist shall dispense no more than a thirty-five day supply of narcotics, controlled drugs or benzodiazepines to any client. (2022)
Subsection 17.5(2)(a) does not apply to drugs indicated for and being used for the prevention and/or treatment of seizure disorders. (2015)
17.5(4) A pharmacist may dispense more than a thirty-five-day supply
of medication provided that:17.5(4) (a) in the member’s professional judgement it is safe to do so; and
(b) the prescriber has specified the exact quantity to be dispensed in excess of the thirty-five-day limit and has stated a reason for ordering that
quantity. (2022)
35 Doses: Where the signa on a prescription does not clearly define the days supply, the pharmacist or certified dispenser shall dispense no more than thirty-five doses
Substitution
When a prescription either written or verbal contains a direction by the prescriber that the prescribed brand of drug is not to be substituted the person dispensing the drug shall not make a substitution unless requested by the client.
Any substitutions must be recorded and forms part of the prescription record
Child Resistant Containers
Any one who fills a prescription in an oral dosage form is required to dispense the drug in a child resistant container.
A child resistant container does not have to be used when:
A client, their prescriber or a responsible agent directs otherwise,
Medications are dispensed in the manufacturers original packaging,
Medications are dispensed in devices or aids to improve compliance,
Medications are being delivered to clients in hospital or nursing home.
If a child resistant container is not being used at the time of filling then a note should be made on the client’s record indicating this.
**Light resistant
Obligations Before Dispensing
17.10 Members must: (a) ensure that a prescription is authentic; (b) refuse to dispense the drug if the member doubts the authenticity of a prescription; (c) review prescriptions for completeness and appropriateness with respect to the drug, dosage, route and frequency of administration; (d) review client personal health for potential drug interactions, allergies, therapeutic duplications and any other drug related issues; (e) consult with clients concerning the client’s drug history and other personal health information (f) consult with the client’s prescriber with respect to the client’s drug therapy where warranted; and (g) follow-up on suspected adverse drug reactions, or other drug related issues
IF the doctors name is illegible write their family doctor and make note
Medication Labels
The label must include:
The drug name and strength,
The name, address and telephone number of the pharmacy,
The prescription number, dispensing date and name of prescriber,
The full name of the client,
The prescriber’s direction for use,
The quantity dispensed,
The DIN, Natural Product Number or Homeopathic Medicine Number as
well as manufacturer’s name or abbreviation,Any other information required to ensure the client takes/uses the
medication appropriately
if the prescription is for a single-entity product, the label must include:
(a) the generic name, strength and the manufacturer’s name,
together on one line(b) if any other drug name, e.g. brand name, is also used, it must be
on a separate line on the label.
17.14(3) In reference to subsection 17.14(1), if the prescription is for a multiple-entity product, the label must include:
(a) the brand name; or
(b) all active ingredients and quantity/strength, and at least one of:
(i) the manufacturer’s name, or
(ii)the drug identification number
If the prescription is for a compounded preparation, the label must include the strength and name of each active ingredient.
Medications dispensed in Compliance aids
Medications dispensed to clients to improve compliance shall conform to the guidance approved by Council with regard to packaging, labelling and storage requirements
Obligations Following Dispensing
Prior to delivering a prescription to the client, the pharmacist has an obligation to ensure the client is counselled in accordance with Standards of Practice and the counselling is
documented in the client’s profile
Client Profile
Minimum information Required
Client’s name
Address
Phone number
Gender
Date of Birth
Any client identification number required for DIS/PMP
Medical conditions and physical limitations
Allergies and drug reactions
Reference to the prescription number for each prescription filled
Documentation on any info collected by the pharmacist relating to med history or info
If the client requests not to use client resistant containers
A client profile is considered property of the pharmacy in which it is prepare
Prescription Verification
The prescription record is to include:
The signature or initials of the person authorizing the prescription to be filled,
The signature or initials of the person preparing the drug for dispensing,
The signature or initials of the person doing the final check,
The signature or initials of the person counselling the client
Prescription Records
The prescription record includes all information recorded in written and electronic format that is pertinent to the prescription being dispensed.
In addition to prescription information, information on a client’s use of Schedule II and Schedule III drugs may also be recorded if its relevant to managing a client’s medication use
Retention of Records
A pharmacy is retain records for a period of two years in written format and electronically for not less than 15 years.
Storage in electronic format means the full original prescription, front and back if applicable and viewable.
The records do not need to be stored in the pharmacy as long as the records are securely stored at a physical location within Canada and are retrievable within a reasonable time.
Records stored electronically need to be encrypted or encoded and access restricted to only authorized personnel
Release of Information
No information contained on a prescription or Client profile should be released to any person without consent of the client.
Information can be released to
Government or agency providing benefits to the client,
Another health care professional,
A police officer on presentation of a search warrant,
Authorized inspectors of Health Canada or NBCP,
A police officer when a forgery, fraud, polypharmacy or double doctoring is suspected or known
Pursuant to the Prescription Monitoring Act
Transfers
A prescription can be transferred in or out of a pharmacy if:
The drug doesn’t contain a controlled drug or narcotic except as
authorized under the CDSAPharmacies providing or receiving the transfer are registered in any
province or territory of Canada.
A prescription can be transferred either verbally or electronically.
When a transfer is made the following info is recorded:
Date of the transfer and name of pharmacist authorizing transfer,
The name of the pharmacist and pharmacy requesting the transfer,
After transfer all remaining refills are cancelled.
The pharmacist, or pharmacy technician who receives the transfer must ensure the authenticity of the person transferring the prescription verbally or electronically and must enter on the transferred prescription record the name of the client, the original prescription date, the date the prescription was last filled by the transferring pharmacy, the initials of the pharmacist who authorized the transfer.
Return to Stock
Any drug or preparation previously delivered to a client cannot be accepted for return to stock.
A drug can be returned for a dosage adjustment or reuse by the same client; or for destruction
Expired Drugs
Expired drugs can not be sold in a pharmacy.
Drugs are considered expired when:
the expiration date has passed,
Its unlikely the drug would be fully consumed before the expiration date
Code of Advertising
Advertising for Pharmacy
Must not be false or misleading
Encourage the misuse or inappropriate use of drugs,
Undermine the integrity of the profession,
Doesn’t make comparisons between pharmacies or pharmacists
Must be verifiable,
Contains no testimonials
Cannot contain information on fee, markup or price
contains no reference to a member’s specialty unless the member is a specialist in a specialty recognized by the College;
contains no information in respect to a fee, markup or price other than descriptive information in respect to a pharmacy’s full retail price for a prescribed medication, which descriptive information must include generic or trade name, manufacturer, strength and quantity.
does not offer any incentive in relation to a prescription drug product or pharmacy services;
does not encourage the transfer of prescriptions by offering the receipt of an incentive associated with filling prescriptions or receiving pharmacy services
Prescribing by Pharmacists
Only pharmacists who have completed the requirements by Council can prescribe.
Types of prescribing
Adapting a prescription,
Altering dose, formulation or regimen,
Renewing a prescription for continuity of care,
Continuing therapy without a prescription for a previously diagnosed condition,
Therapeutic substitution,
Prescribing non-prescription drugs, treatments and devices,
Prescribing in an emergency,
Collaborative practice,
Prescribing for minor ailments
A pharmacist may only prescribe a drug, treatment or device if:
the indication and treatment is within the pharmacist’s scope of practice, knowledge, skills, competencies and experience;
the pharmacist has:
performed an assessment in an environment that is appropriate,
determined treatment is indicated,
discussed treatment options with the client, and
prescribed the most appropriate treatment based on the assessment; and
the drug is appropriate to treat the client’s condition.
a pharmacist shall not prescribe a drug unless the pharmacist has obtained sufficient information by reviewing the client’s medication history and discussing treatment options with the client or, if necessary, and with the client’s consent, obtains pertinent information about the client’s care and treatment from family, friends, or caregivers.
there is an established pharmacist-client relationship
prescription decision of the pharmacist has been consented to by the client, or by the client’s parent or legal guardian,
the pharmacist has successfully completed any training requirements determined by Council, and has available any required reference resources
shall assess the client in person at the time of prescribing.
the pharmacist has seen the client personally in the past and has an established professional relationship with the client;
the pharmacist has sufficient knowledge of the client’s condition and current clinical status relevant to the prescribing decision; and
the pharmacist communicates with the client or their agent at the time of prescribing
the pharmacist has assessed the client in compliance with the Code of Ethics and Standards of Practice and any applicable practice directives;
the drug is prescribed in a circumstance which is within the pharmacist’s area of practice, knowledge and skills, or specialty;
the pharmacist has determined that a prescription is reasonably necessary to treat the client; and
the pharmacist has discussed with the client, or their agent, reasonable and available therapeutic options.
If the pharmacist identifies that the condition being assessed is outside his or her scope of practice, the pharmacist shall refer the client to an appropriate health care practitioner, and shall record the assessment and the referral in the client’s profile
a follow-up plan that is sufficiently detailed to monitor the client’s progress and ensure continuity of care by the pharmacist,
or other regulated health professionals or caregivers, if applicable; and
any other advice or treatment recommended to the client.
The pharmacist, when prescribing a drug, treatment or device, will notify the client’s primary care provider (when such exists) when the order the pharmacist is prescribing is clinically significant.
Prescribing for Minor Ailments
A pharmacist is authorized to prescribe a drug, treatment or device that is in Schedule I, Schedule II or Schedule III or is an unscheduled drug for the treatment of a condition, if the drug, treatment or device is indicated for treatment of a minor ailment
Appendix 2: List of Minor Ailments
Allergic Rhinitis
Calluses and Corns
Contact Allergic Dermatitis
Dandruff
Dysmenorrhea
Dyspepsia
Emergency Contraception
Fungal Infections of the Skin
Gastro-esophageal
Reflux Disease
Hemorrhoids
Herpes Simplex
Impetigo
Mild Acne
Mild Headache
Mild to Moderate Eczema
Mild Urticaria (including bites and stings)
Minor Joint Pain
Minor Muscle Pain
Minor Sleep Disorders
Nasal Congestion
Nausea
Nicotine dependence
Non-infectious Diarrhea
Oral Fungal Infection (thrush)
Oral Ulcer
Threadworms and Pinworms
Upper respiratory tract conditions (cough, nasal congestion and
discharge, sore throat, fever, headache, malaise)Urinary Tract Infection (uncomplicated)
Vaginal Candidiasis
Warts (excluding facial and genital)
Xerophthalmia (dry eyes)
Contraception Management
Paxlovid
Herpes Zoster (Shingles)
Prescribing for Preventable
Diseases
Subject to Sections 2 & 3, pharmacists may prescribe and administer Schedule
I, Schedule II, Schedule III and Unscheduled vaccines (individual or combination
products) and/or drug products for the prevention of the following diseases:Cholera (pharmacist may prescribe only the oral, inactivated vaccine)
Diphtheria
Haemophiles influenzae type B
Hepatitis A
Hepatitis B
Herpes zoster (shingles)
Human Papillomavirus (HPV)
Malaria
Measles
Meningococcal disease
Mumps
Pertussis
Pneumococcal Disease
Polio
Rubella
Seasonal Influenza
Tetanus
Traveler’s Diarrhea (pharmacist may also prescribe pre-emptive treatment)
Varicella zoster (chickenpox)
Pharmacists may ADMINISTER injectable vaccines for the following diseases but they may NOT PRESCRIBE injectable vaccines for the following diseases unless they have successfully completed a training program in travel medicine approved by Council. (These are usually required for international travel.)
Cholera (other than the oral, inactivated vaccine)
European tick-borne encephalitis
Japanese encephalitis
Rabies
Typhoid
Yellow fever
Criteria for Prescribing
the pharmacist has made an assessment to determine whether the drug will be safe and effective in the circumstances of the client, including, but not limited to the following:
the client’s symptoms,
co-existent disease states and chronic conditions,
the client’s allergies and other contraindications and precautions,
other medications the client may be taking,
the client’s gender, age, weight and height (where applicable),
pregnancy and lactation status, if applicable, and
any other inquiries reasonably necessary in the circumstances
Prescribing Restrictions
A pharmacist may not prescribe
for themselves;
for any person with whom there is a close personal or emotional relationship; or (friends/family)
in contravention of federal legislation, including the Narcotic Control Act and its Regulations, the Controlled Drugs and Substances Act and its Regulations or any successor act or regulation
Recording of Prescribing
must make and retain a record of all information necessary for prescriptions PLUS:
the circumstances under which the drug was prescribed;
the rationale for prescribing – diagnosis, treatment plan, clinical indication, or expected outcome;
a summary of the pharmacist’s assessment of the client;
the name, address, and telephone number of the pharmacist issuing the prescription;
pharmacist’s signature and registration number
Part XXII- Administration of Drugs
have successfully completed an educational training program approved by Council;
have policies and procedures in place for administering drugs and dealing with emergencies;
ensure that the environment in which the drug is to be administered is appropriate;
have proper regard for the interests of the client and take all steps necessary to ensure that the drug is administered safely; and
have successfully completed any other requirements specified by Council.
Administration of Drugs
Routes of Administration are:
Orally including sublingual and buccal,
Topically including ophthalmic, Otic and intranasal,
Via inhalation.
A pharmacist who meets requirements of the Administration of Injections
Policy may administer a drug, biological or blood product:Through intra-dermal injection,
Through subcutaneous injection,
Through intramuscular injection or
Intravenously through an established central or peripheral venous access device
Pharmacists may only administer an injectable vaccine to a client who is 5 years of age or older, and only after having successfully completed an injection administration training program approved by Council. (2016)
Record of Drug Administration
must make and retain a record in the pharmacy of:
the name and address of the client;
the name of the drug and total dose administered;
the route, and site, of administration;
the lot number and expiry date of the product administered;
the name of the pharmacist administering the drug;
the date and the time of the administration;
any client counselling provided; and
any adverse events and their management
Part XXIII- Tests
A pharmacist may interpret the results of any clinical test performed by the client, and may give advice to the client regarding the results and implications of those tests.
A pharmacist may administer the clinical tests approved by Council, interpret their results and give advice to the client regarding the results and implications of those tests
Test Interpretation Record
A pharmacist who interprets and makes a recommendation to a client regarding a clinical test must make and retain a record in the pharmacy of:
the name and address of the client;
the nature of the test interpreted;
the date of the test;
the results of the test; the nature of the advice given to the client; and
the pharmacist’s name
Ordering Tests
A pharmacist may administer a test, or order, and receive the results of, a
laboratory screening or diagnostic test when deemed appropriate and
necessary for the care of the client.If test results reveals medical issues requiring attention; or that, the pharmacist is not able to interpret, must
promptly forward the results to any other health professional responsible for the client’s care for the interpretation of the results;
discuss the interpretation and course of action to be followed with the health professional when required;
recommend a course of treatment, if appropriate.
The pharmacist and the other health professional will determine which will advise the client of the test results
Test Ordering and Results Record
A pharmacist who administers a test, or orders and receives the results of a screening or diagnostic test must make and retain a record in the pharmacy of:
the name and address of the client;
the nature of the test administered or ordered;
the name of any health professional to whom the results were forwarded, or a recommendation was made;
the name of the pharmacist requesting the test;
the date the test was ordered;
the date the results were received; the date the results were communicated by the pharmacist to the client, if the pharmacist is able to interpret the results, and other health professionals responsible for the client’s care
Professional Development
Members are to maintain a portfolio documenting ongoing learning activities, as a condition of maintaining membership with the college.
Members may be requested to submit or present in person their portfolio to the college upon request for audit, review and discussion
Insurance
Pharmacy technicians need liability insurance that provides a minimum of $1,000,000 per claim or occurrence and a minimum of $2,000,000 annual aggregate.
Proof of personal professional liability insurance shall be provided to the Registrar upon registration and annually at the time of license renewal, or when requested
NBCP-Pharmacy Act https://nbppharmacists.ca/wp-content/uploads/2020/12/New-Act-with-Table-of-Contents.pdf?x43718
Definitions
administer = the direct application of a drug, or treatment, to the body of a client by ingestion, application, inhalation, injection, or any other =. (administrer)
Administrator= the Administrator of Complaints appointed by Council to carry out the responsibilities set out in Part X. (administrateur)
applicant= a person applying for admission to membership in the College or reinstatement in the College. (postulant)
certificate of operation= a certificate of any category authorizing the operation of a pharmacy, and issued to a manager. (certificate d’exploitation)
Certified dispenser: a person whose name is entered on a register of Certified dispensers. (dispensateur agréé)
Code of Ethics= the Code of Ethics adopted by the College, as amended from time to time. (Code de déontologie)
compound: to prepare components into a drug product, including the preparing of drugs or devices in anticipation of receiving prescriptions based on routine, regularly observed prescribing patterns. (composition)
conduct includes an act or omission. (conduite)
Council= the Council of the College. (Conseil)
Court = the Court of Queen's Bench of New Brunswick. (Cour)
day= a calendar day. (jour)
dispensing = the interpretation and clarification of a prescribers order and the assembly and preparation of the order for delivery to the client. (exécuter une ordonnance ou dispenser)
document includes:
(a) any record containing information whether in legible, visible or audible form, or stored electronically,
(b) files, papers, books, accounting records, banking records, prescriptions, photographs, plans, charts, prints, drawings, films, tapes, video cassettes, diskettes, word processing software and other machine readable records regardless of physical form or characteristics, and
(c) any part of a document. (document)
“Drug”: includes any substance or mixture of substances manufactured, compounded, sold or represented for use in:
(a) the diagnosis, treatment, mitigation or prevention of a disease, disorder or abnormal physical state, or its symptoms, in human beings or animals, or
(b) restoring, correcting or modifying organic functions in human beings or animals. (médicament)
employee: a person directly or indirectly providing services to an employer, whether as an independent contractor or employee, and regardless of whether such services are provided on a full-time, part-time or casual basis. (employé)
health professional = a person who provides a service related to:
(a) the preservation or improvement of the health of individuals, or
(b) the diagnosis, treatment or care of
individuals who are injured, sick, disabled or infirm,
and who is regulated under a private Act of a Canadian legislature, or Parliament, with respect to the provision of the service, and includes a social worker registered under the New Brunswick Association of Social Workers Act, 1988. (professionnel de la santé)
inspector = a person appointed by Council or the Registrar, or the Registrar himself or herself, to investigate, audit or inspect matters related to the practice of pharmacy. (inspecteur)
intern = a person whose name is entered in the register of interns. (stagiaire)
internship = a period of practical training under the supervision of a preceptor approved by Council. (stage)
lay representative: a person who is appointed as a public representative under this Act. (représentant du public)
limited access drug = a drug which shall not be sold:
(a) without a prescription, or
(b) without the supervision or intervention
of a member in accordance with this Act and the Schedules established pursuant to section 27. (médicament à accès limité)
manager = the member designated to have authority over and be responsible for the operation of the pharmacy. (gérant)
member = a member of the College as defined in Part VIII. (membre)
Minister = the Minister of Health for New Brunswick, or his or her successor. (ministre)
"person" includes an individual, a partnership, a corporation and any other organization or entity. (personne)
pharmaceutical alternative: is a drug product that contains the same therapeutic moiety, but different salts, esters, or complexes of that moiety, or is a different dosage form or strength. (substitut pharmaceutique)
pharmaceutically equivalent: a drug product that, in comparison with another
drug, contains identical amounts of the identical medicinal ingredients, in comparable dosage forms, but that does not necessarily contain the same non-medicinal ingredients. (équivalent pharmaceutique)pharmacist= a person whose name is entered on a register of pharmacists. (pharmacien)
pharmacy:
(a) the location where distributive, cognitive or consultative services are provided to the general public relating to drugs, medicines, compounding, dispensing prescriptions and/or health, and
(b) other locations as defined in the regulations. (pharmacie)
pharmacy residency is an organized, directed, accredited program that builds upon knowledge, skills, attitudes, and abilities gained from an accredited professional pharmacy degree program, with the purpose of enhancing general competencies in managing medication- use systems and supporting optimal medication therapy outcomes for clients with a broad range of disease states. (résidence en pharmacie )
pharmacy technician: a person whose name is entered on a register of technicians. (technicien en pharmacie)
pharmacy technician student= a person whose name is entered on a register of pharmacy technician students. (étudiant en technique pharmaceutique)
“PEBC” = the Pharmacy Examining Board of Canada. (BEPC)
“Pharmacist – Direct Client Care” = a pharmacist in active practice that had direct contact with clients for at least 400 hours during the preceding two-year period. (pharmacien – ASSISTANCE DIRECTE AUX CLIENTS)
“Pharmacy technician – Direct Client Care” = a pharmacy technician in active practice, under the supervision of a Pharmacist – Direct Client Care, for at least 400 hours during the preceding two-year period. (technicien en pharmacie – ASSISTANCE DIRECTE AUX CLIENTS)
“Pharmacy technician – Non-Direct Client Care” = a pharmacy technician in active practice who does not meet the criteria of a Pharmacy technician – Direct Client Care (e.g. pharmacy technicians in administrative, management or other non-direct care positions). (technicien en pharmacie – SANS ASSISTANCE DIRECTE AUX CLIENTS)
practice directive = a written statement made by Council for the purpose of giving practice direction to the members. (directive professionnelle)
preceptor = a person who meets the qualifications prescribed in the regulations (précepteur)
prescriber = a legally qualified health professional or a veterinarian, authorized to prescribe drugs or devices in any Canadian jurisdiction, and who gives a prescription. (prescripteur)
prescription = a direction given by a prescriber directing that a drug, device, or treatment specified in the direction be dispensed for the person named, or animal described, in the direction. (ordonnance ou prescription)
record includes documents as well as information described in the regulations, but does not include electronic software or any mechanism that produces records. (dossier)
regional health authority or RHA = a regional health authority established under the Regional Health Authorities Act, or as defined by the Minister. (régie régionale de la santé)
register = a register established under Part IX. (registre)
Registrar= the Registrar of the College appointed under section 13. (registraire)
record = the records of a pharmacy, whether in written, photographic, magnetic, electronic or other form, and includes, without limitation,
(a) the records of the proprietor of the pharmacy, the manager, the regulated members engaged by the proprietor or any other person associated with the pharmacy;
(b) any record required to be kept under the Act, the Controlled Drugs and Substances Act (Canada) or the Food and Drugs Act (Canada) or the regulations or standards under those acts;
(c) a record of all prescriptions the pharmacy receives, including an identification of the prescriptions that the pharmacy transfers to another pharmacy or pharmacist
d) a record of all drugs dispensed from or through the pharmacy, including the prescription, the name of the drug, the amount dispensed, the name and contact information of the client and the name and contact information of the prescriber;
(e) a record of the pharmacy services provided, including the name of the person or persons who dispensed a drug, or provided a pharmacy service;
(f) a record of the names and contact information of the clients to whom pharmacy services are provided; and
(g) a record of the counselling services provided to a client. (dossier)
regulations= the regulations of the College made under Part VI, and includes
the Code of Ethics. (règlement)restriction= a limitation placed on privileges to practice. (restriction)
retailer= a person who sells consumer goods to the public within the Province of New Brunswick and does not operate a pharmacy under the authority of a certificate of operation issued under this Act. (détaillant)
sell= to sell, advertise for sale, offer for sale, offer to arrange for another person to sell, expose for sale, have in possession for sale, or distribute, whether or not the distribution is made for consideration. (vendre)
standards of practice = the standards regarding the practice of members and the operation of pharmacies established in the regulations. (norme d’exercice)
supervision is a process in which two or more persons (one of whom is the person being supervised) participate in a joint effort to promote, establish, maintain and evaluate a level of performance, at levels defined in the regulations. (encadrement)
suspension = loss of privileges for a specified period of time. (suspension)
therapeutic equivalent: a drug product that can be expected to have the same clinical effect and safety profile as another drug. (équivalent thérapeutique)
wholesaler = a person who sells or distributes drugs and devices mainly for resale or business use, but excludes a manufacturer. (grossiste)
Part III: Objects and Duties of the College
(a) promote and protect the health and well-being of the public, in collaboration with other health disciplines, through regulation and development of the pharmacy profession;
(b) require that for the safety of the public, all persons engaged in the practice of pharmacy within the Province are acquainted with the processes of the profession and possess a competent practical knowledge of pharmacy;
(c) require that the profession of pharmacy is practised by its members in accordance with standards set by the College;
(d) regulate the practice of pharmacy and govern its members;
(e) maintain and develop standards of practice for members;
(f) establish, maintain and develop standards of professional ethics for its members;
(g) administer this Act and perform such other duties and exercise such other powers as are imposed or conferred on the College by or under any Act;
(h) uphold and protect the public interest in the practice of pharmacy;
(i) hold forth the independence, integrity and honour of the profession;
(j) establish and maintain standards for the education, knowledge, qualifications,
professional responsibility and competence of its members and applicants; and(k) ensure the safe, rational and effective use of drugs and devices, and support members in the continued improvement of pharmacy services to the public.
Part IV: Council
6(1) The College shall be governed by a Council consisting of Councilors who shall be:
(a) members of the College elected pursuant to section 7, being not fewer than six and not more than twenty-four;
(b) lay representatives appointed pursuant to section 8; and
(c) other persons, in the number and manner provided for in the regulations.
6(2) Council shall exercise all the powers and functions of the College
Part V: Powers of Council
Committees
(12) Council shall establish and appoint as here provided the following
committees:(a) the Complaints Committee,
(b) the Discipline and Fitness to Practice Committee,
(c) other committees deemed necessary by Council.
Regulations respecting pharmacy technician
16(1) As regards to pharmacy technicians, Council shall make regulations that establish
(a) criteria and conditions under which pharmacy technicians are permitted to practice pharmacy, subject to subsection 49(3);
16(2) Council shall make regulations imposing on persons desiring to become pharmacy technicians:
(a) the educational requirements to be met;
(b) a period of internship for a set time period; and
(c) other conditions to be met.
Part VI: Regulations of the College
Regulations respecting pharmacy technicians
16(1) As regards to pharmacy technicians, Council shall make regulations that establish
(a) criteria and conditions under which pharmacy technicians are permitted to practise pharmacy, subject to subsection 49(3);
16(2) Council shall make regulations imposing on persons desiring to become pharmacy
technicians:(a) the educational requirements to be met;
(b) a period of internship for a set time period; and
(c) other conditions to be met.
Coming into effect of regulations
22(1) A new regulation, or the amendment or repeal of a regulation, is not effective unless
(a) a majority of Councilors then in office vote in favour of it; and
(b) it has been approved, with or without amendment, by majority vote at an annual or special meeting of the College, and subject to subsection (2), it comes into force upon approval by the members or at such later date as provided in the regulation.
…the member obtained pursuant to the regulations, and the Minister obtained pursuant to subsection (3), Council may make, amend or repeal regulations relating to matters respecting
(a) Composition of Council and eligibility for Council membership;
(b) admission of members;
(c) setting or expanding the scope of practice for members;
(d) the adoption or deletion, in whole or in part, of any nationally accepted schedule or formulary adopted by reference as a Drug Schedule;
(e) the prescribing or
(f) members' authority to delegate duties;
(g) criteria for the eligibility to be entered in any of the practice registers, including recognition of educational credentials; and
(h) ordering of diagnostic tests
22(3) Upon receiving a written request from the College to make, amend or repeal a
regulation pursuant to subsection (2), the Minister shall, within thirty days, in writing,
either:(a) approve the request;
(b) reject the request with reason; or
(c) extend the time for his or her decision for a period not to exceed a further sixty days.
22(4) If no written response is received from the Minister at the end of the original or extended period provided for in subsection (3), the Minister shall be deemed to have accepted the proposed
Part VII: Meetings
28 An annual general meeting of the members of the College shall be held each year at a time and place designated by Council, convened in accordance with the regulations.
Special General Meeting
31 Council may at any time. convene a special general meeting of the College as provided in…
Part IX: Right to Practice
Interim suspension by registrar
42(1) If the Registrar believes that a matter exists relating to a member's practice that presents or is likely to present a serious risk to the public, the Registrar may:
(a) direct the member to rectify the matter;
(b) suspend the member's licence, pending a review of the matter by the Complaints Committee or the Discipline and Fitness to Practise Committee.
42(2) Failure to rectify the matter contrary to paragraph (1)(a) may constitute professional misconduct.
Referral of Complaints
42(3) Upon suspending a license under paragraph (l)(b), the Registrar shall refer the matter to the Complaints Committee or to the Discipline and Fitness to Practise Committee.
42(4) A panel of the committee shall hold a hearing into the interim suspension within ten days.
Practice of Pharmacy
49(1) The practice of pharmacy promotes health, the prevention and treatment of diseases, dysfunction and disorders through proper drug therapy and non-drug therapy
49(3) The practice of pharmacy by pharmacy technicians is limited to:
(a) the distributive component of the dispensing process (drug and product
distribution);(b) compounding and preparing drug products for dispensing;
(c) ensuring accuracy and quality of the final drug product;
(d) supervising and managing drug distribution systems to optimize the safety and efficiency of operations
(e) accepting activities delegated by another health care professional;
(j) directing clients to consult with other health care providers when appropriate; and
(g) other activities defined in the regulations.
49(6) Honorary members and members on retired or non-active registers are not authorized to practise pharmacy.
49(8) Nothing in this Act or the regulations prevents a pharmacy technician on an active or conditional register, who is employed in the public sector, from delegating
functions to a non-technician who is under the pharmacy technician's supervision.57 No person except a pharmacy technician shall use the title pharmacy technician or a variation of such title or an equivalent in another language
. 58 No person shall 'Use the initials "R.Ph.T." or "RPhT“ or initials which would imply that the person is a pharmacy technician, unless the person is a pharmacy technician
60 No person except a pharmacy technician student shall use the title
pharmacy technician student or student pharmacist technician or a variation of such title or an equivalent in another language
Part X: Discipline and Competency
Interpretation
69(1) The following definitions apply in this Part.
"caution" is intended to express the dissatisfaction of the committee and to forewarn the respondent that if conduct recurs, more serious disciplinary action may be Considered. (avertissement)
"censure" is the expression of strong disapproval or harsh criticism. (remontrance) "conduct deserving censure" includes:
(a) professional misconduct;
(b) conduct unbecoming a member of the College;
(c) acting in breach of this Act, the regulations, the Code of Ethics or practice directives;
(d:) incompetence in the practice of pharmacy; and
(e) any other matter that, in the opinion of the Complaints Committee or the Discipline and Fitness to Practise Committee, does not meet the prevailing standards of practice or conduct expected of a member in the practice of pharmacy. (conduit meritant remontrance)
"counsel" is advice as to how to improve the respondent's practice. (conseils)
"Court of Appeal" means The New Brunswick Court of Appeal. (Cour d'appef)
"incapacitated" means, in relation to a member, that the member has a physical or mental condition or disorder, or substance abuse problem that makes it desirable in the interest of the public that the member no longer be permitted to practise or that the member's practice be restricted, and
"incapacity" has a corresponding meaning. (incapacite)
"incompetence" means, in relation to a member, that the member's professional care of a client displays lack of knowledge, skill or judgement, or disregard for the welfare of the client of a nature, or to an extent, that demonstrates that the member is unfit to continue to practise, or that the member's practice should be restricted. (incompetence)
“Professional Misconduct” means the member has:
(a) pleaded guilty to or been found guilty of an offence that, in the opinion of either the Complaints Committee or the Discipline and Fitness to Practise Committee, is relevant to the member's suitability to practise or carry out professional responsibilities;
(b) been adjudged guilty of an act of professional misconduct by the governing body of a health profession in a jurisdiction other than New Brunswick that would, in the opinion of either the Complaints Committee or the Discipline and Fitness to Practise Committee, constitute professional misconduct under this act
(c) digressed from established or recognized professional standards or ethics of the profession;
(d) committed an act of professional misconduct as defined in the regulations;
(e) violated or failed to comply with this Act or the regulations;
f) violated or failed to comply with a condition or limitation imposed on the member's licence;
(g) failed to submit to an examination ordered by the Committee under subsection 86(1);
(h) sexually abused a client;
(i) failed to file a report pursuant to sections 70, 71 or 72 or paragraphs 18 if) or l4(2)(c); or
(j) continued to practise while knowing himself or herself to be incapacitated. (faux professionnelle) "respondent" means a member, former member, applicant or any
person whose conduct is being inquired into under this Act. (intime)
Mandatory reporting of sexual abuse
70(1) A member who, in the course of practising the profession, has reasonable grounds to believe that another health professional has sexually abused a client; and who fails to file a report in writing in accordance with subsection (4) with the governing body of the health professional within twenty- one days after the circumstances occur that give rise to the reasonable grounds for the belief, commits an act of professional misconduct.
70(2) A member is not required to file a report pursuant to subsection (1) if the member does not know the name of the health professional who would be the subject of the report.
70(3) If the reasonable grounds for filing a report pursuant to subsection (1) have been obtained from one of the member's clients, the member shall use his or her best efforts to advise the client that the member is filing the report before doing so.
70(4) A report filed pursuant to subsection (1) shall contain the following information:
(a) the name of the member filing the report;
(b) the name of the health professional who is the subject of the report;
(c) the information the member has of the alleged sexual abuse; and
(d) subject to subsection (5), if the grounds of the person filing the report are related to a particular client of the health professional who is the subject of the report, the name of the client.
70(5) The name of the client who may have been sexually abused shall not be included in a report unless the client, or if the client is incapable, the client's representative, consents in writing to the inclusion of the client's name.
70(6) No action or other proceeding shall be instituted against a member for filing a
report in good faith pursuant to subsection (1).
Other Mandatory Reports
71(1) A person who terminates or suspends the employment of a member or who imposes restrictions on the practice of a member for reasons of professional misconduct, incompetence or incapacity shall file with the Registrar within thirty days after the termination, suspension r imposition a written report setting out the reasons.
71(2)…employment of a member or to impose restrictions on the practice of a member for reasons of professional misconduct, incompetence or incapacity but did not do so because the member resigned, the person shall file with the Registrar within thirty days after the resignation a written report setting out the reasons upon which the person had intended to act.
71(3) This section applies to every person who employs a member.
72(1) A person who dissolves a partnership or association with another member for reasons of professional misconduct, incompetence or incapacity and who fails to file a written report with the Registrar within thirty days after the dissolution setting out the…
72(2) A member who believes that another member is suffering from a physical or mental condition or disorder of a nature or to an extent that the other member is unfit to continue to practise or that his or her practice or pharmacy operation should be restricted, shall inform the Registrar of that belief and the reasons for it.
72(3) Following any action against a member by any other licensing authority, by any health care institution, by any professional association, by any governmental agency, by any law enforcement agency, or by any court, for any act or conduct which could constitute professional misconduct under this Act, or for any conduct which could lead to a finding under this Act that a member is incapacitated or unfit to practise, the member shall report such information to the Registrar without delay.
73 No action or other proceeding shall be instituted against a person for filing a report in good faith under sections 71 or 72
Complains
76(1) A complaint against a respondent shall be:
(a) in writing; and
(b) delivered to the Administrator.
76(2) A complaint against a pharmacy is a complaint against the manager.
77 Any person may file a complaint, including the Administrator when acting pursuant to section 75, or the Registrar in circumstances where no complaint has been received from any other person, and it is in the public interest that action be taken immediately
78(1) Upon receipt of a complaint, or when acting under sections 75 and 80, the Administrator shall:
(a) if necessary, obtain additional information from the complainant and carry out an investigation; and
(b) provide the respondent with
(i) a copy of the complaint, and
(ii) the date by which a reply must be filed with the Administrator, which date shall not be later than twenty-one days after the date when the Administrator mails or delivers the complaint.
78(2) Upon receipt of the respondent's reply the Administrator may:
(a) investigate the complaint further should circumstances require;
(b) settle the complaint to the satisfaction of the complainant if the complaint alleges conduct deserving sanction that appears to the Administrator not to warrant action by the Complaints Committee or Discipline and Fitness to Practise Committee;
(c) refer the complaint to the Complaints Committee;
(d) refer the complaint to the Discipline and Fitness to Practise Committee if the subject matter is, in the opinion of the Administrator, sufficiently serious to warrant such referral; or
(e) dismiss the complaint if, in the opinion of the Administrator, it is without merit
78(3) A complainant who is dissatisfied with the decision of the Administrator in disposing of the complaint may request in writing a review by the Complaints Committee.
78(4) The Administrator or the Complaints Committee shall advise the complainant and the respondent in writing of the disposition of a complaint under subsections (2) or (3), as the case may be, and shall give reasons.
78(5) When a complaint is referred to the Complaints Committee, the Administrator shall provide the Committee with a full report of the results of any investigation, the complaint, the respondent's reply and any documentation and information relevant to the complaint.
78(6) When a complaint is referred to the Discipline and Fitness to Practise Committee, the Administrator shall comply with sections 93 and 95.
78(7) The Administrator shall report his or her actions on all complaints to Council, without disclosing the names of the parties.
79(1) An apology made by or on behalf of a person in connection with any matter that is or may become the subject of a complaint:
(a) does not constitute an express or implied admission of fault by the person in connection with that matter;
(b) does not, despite any wording to the contrary in any contract of insurance or indemnity and despite any other Act or law, void, impair or otherwise affect any insurance or indemnity coverage for any person in connection with that matter; and
(c) shall not be taken into account in any investigation or…
TLDR An Apology is not proof of wrongdoing
79(2) Despite any other Act or law, evidence of an apology made by or on behalf
of a person in connection with any matter that is or may become the subject of a
complaint, including the factual admissions made in the document containing the
apology, is not admissible in any civil or administrative proceeding, in a criminal prosecution or in an arbitration as evidence of the fault, liability or culpability of any person in connection with that matter.
TLDR Doesn’t count if it is during a court case
79(3) Notwithstanding subsection (2), if a person makes an apology while testifying at a civil proceeding, including while testifying at an out of court examination in the context of the civil proceeding, at an administrative proceeding, in a criminal trial or at an arbitration, this section does not apply to the apology for the purposes of that proceeding or arbitration.
Investigation Complaints
80 The Administrator shall investigate all matters that may constitute conduct deserving sanction, notwithstanding that no complaint has been received under section 78, or the complaint has been withdrawn, and may carry out investigations on the request of any person or of Council.
81 If an investigation under section 80 discloses that a respondent may deserve sanction, the Administrator shall cause a complaint to be filed with the Complaints Committee or refer the complaint directly to the Discipline and Fitness to Practise Committee, as per subsection 78(2).
Product Selection and Privacy
128(1) - A pharmacist may dispense a pharmaceutically equivalent, a pharmaceutical alternative or a therapeutic equivalent, all as defined in this Act or in the regulations, unless otherwise directed by the prescriber, or requested by the client.
No liability for dispensing pharmaceutically equivalent products
129 - No action or other proceeding lies or shall be instituted against a prescriber, pharmacist or any member under the supervision of a pharmacist, on the grounds that a pharmaceutically equivalent or a pharma ceutical alternative other than the one prescribed was dispensed in accordance with this part
What is personal information?
Be careful what we share and use for information
Under PIPEDA, personal information includes any factual or subjective information, recorded or not, about an identifiable individual. This includes information in any form, such as:
age, name, ID numbers, income, ethnic origin, or blood type;
opinions, evaluations, comments, social status, or disciplinary actions; and
employee files, credit records, loan records, medical records, existence of a dispute between a consumer and a merchant, intentions (for example, to acquire goods or services, or change
jobs).The principles are:
1.Accountability
2.Identifying Purposes
3.Consent
4.Limiting Collection
5.Limiting Use, Disclosure, and Retention
6.Accuracy
7.Safeguards
8.Openness
9.Individual Access
10.Challenging Compliance
Accountability
Your responsibilities
Comply with all 10 fair information principles.
Appoint someone to be responsible for your organization’s PIPEDA compliance.
Protect all personal information held by your organization, including any personal information you transfer to a third party for processing.
Develop and implement personal information policies and practices.
Identifying Purposes
Identify and document your purposes for collecting personal information. This will help you determine which specific personal information to collect to fulfill those purposes.
Tell your customers why your organization needs their personal information before or at the time of collection. Depending on how the information is collected, this can be done orally or in writing.
Obtain their consent again should you identify a new purpose.
Consent
Meaningful consent is an essential element of PIPEDA. Organizations are generally required to obtain meaningful consent for the collection, use and disclosure of personal information.
To make consent meaningful, people must understand what they are consenting to. It is only considered valid if it is reasonable to expect that your customers will understand the nature, purpose and consequences of the collection, use or disclosure of their personal information.
Consent can only be required for collections, uses or disclosures that are necessary to fulfil an explicitly specified and legitimate purpose. For non-integral collections, uses and disclosures, individuals must be given a choice.
The form of consent must take into account the sensitivity of the personal information. The way you seek consent will depend on the circumstances and type of information you are collecting. Individuals can withdraw consent at any time, subject to legal or contractual restrictions and reasonable notice, and you must inform individuals of the implications of withdrawal.
Limiting Collection
Collect only the personal information your organization needs to fulfill a legitimate identified purpose.
Be honest about the reasons you are collecting personal information.
Collect personal information by fair and lawful means. This requirement is intended to prevent organizations from collecting information by misleading or deceiving about the purpose
Limiting Use, Disclosure, and Retention
Unless someone consents otherwise—or unless doing so is required by law—your organization may use or disclose personal information only for the identified purposes for which it was collected.
Keep personal information only as long as it is needed to serve those purposes. Know what personal information you have, where it is, and what you are doing with it.
Obtain fresh consent if you intend to use or disclose personal information for a new purpose.
Collect, use or disclose personal information only for purposes that a reasonable person would consider appropriate in the circumstances.
Put guidelines and procedures in place for retaining and destroying personal information.
Accuracy: Minimize the possibility of using incorrect information when making a decision about an individual or when disclosing information to third parties.
Safeguards
Protect personal information in a way that is appropriate to how sensitive it is.
Protect all personal information (regardless of how it is stored) against loss, theft, or any unauthorized access, disclosure, copying, use or modification
Openness: Inform your customers and employees that you have policies and practices for managing personal information.
Make these policies and practices easily understandable and easily available.
Individual Access:When asked, advise people about the personal information about them your organization holds.
Explain where the information was obtained.
Explain how that information is or has been used and to whom it has been disclosed.
Give people access to their information at minimal or no cost, or explain your reasons for not providing access. Providing access can take different forms. For example, you may provide a
written or electronic copy of the information, or allow the individual to view the information or listen to a recording of the information.
Correct or amend personal information in cases where accuracy and completeness is deficient.
Note any disputes on the file and advise third parties where appropriate.
Challenging Compliance
Provide recourse by developing simple complaint handling and investigation procedures.
Tell complainants about their avenues of recourse. These include your organization’s own complaint procedures, along with those related to industry associations, regulatory bodies and the OPC.
Investigate all complaints you receive. Improve any information-handling practices and policies that are found to be problematic
Non-Disclosure of Confidential information and documents
140(1) A person who, in the course of carrying out duties under this Act or the regulations, becomes aware of information Or a document that is confidential has the same obligation
respecting disclosure of that information or document as the member from whom the information or document was obtained.140(2) A member who, in accordance with this Act or the regulations, provides the College with information or a document that is confidential shall be deemed not to have breached any duty or obligation that the member would otherwise have had to the College or the client not to disclose the information or document.
140(3) A person who, during the course of any court proceeding with respect to a matter under this Act or the regulations, becomes aware of information or a document that is confidential shall not utilize, produce or disclose the document or information for a purpose other than that for which it was obtained
140(4) In any court proceeding with respect to a matter under this Act or the regulations, the Court may exclude members of the public from the hearing where the Court considers the exclusion is necessary to prevent the disclosure of information or the production of a document that is confidential.
140(5) In giving reasons for judgement in any court proceeding, the Court shall take all reasonable precautions to avoid including in its reasons any information before the Court that is confidential.
140(6) In addition to the requirements in this Act and in the regulations, members shall comply with the requirements of the New Brunswick Personal Health Information Privacy and Access Act, or any successor legislation
Code of Ethics (02/28)
Self-regulation is a privilege granted by government on the condition that the self-regulating profession agrees to put the interests of the public above its own interests collectively, and above registrants’ interests individually. The alternative to self-regulation is unilaterally- imposed government regulation. The Act requires that all decisions and activities of the College be made in the public interest
Acting in the public interest broadly encompasses:
Duties to the public: To promote and protect the health, well-being, safety and
interest of the public (i.e., individuals who utilize pharmacy services or “patients”)Duties of Conduct: To hold forth the independence, integrity and honour of the profession.
Purpose:
Competency and ethics are tightly intertwined and the CoE (code of ethics) is applicable to all pharmacy practice whether direct patient care or otherwise. All registrants are responsible to the College and therefore the public for application of the CoE in the context of their professional environment. This document provided by NBCP is a foundation for practice that interlinks with standards of practice; provincial and federal legislation; and College regulation
The Code of Ethics is used by the Public, Registrants and the College in order to:
Articulate the ethical principles for pharmacy professionals
Serve as an educational resource
Self-evaluate knowledge, skills and attitudes pertaining to ethics in the course of Continued Professional Development
Establish a basis for the evaluation of registratints’ conduct in the course of complaints and discipline proceedings
This CoE purposefully provides a conceptual rather than a granular approach to codifying pharmacy professionals’ ethical practice.
Registrants may not justify unethical behaviour by rationalizing that a given behaviour is not expressly prohibited by this CoE. (Code of Ethics)-pertains where direct or not
Authoring an exhaustive list of ethical rules is unrealistic given the infinite number of situations and scenarios potentially presenting in practice
Value Based Decision Making (00:11:48)
STEP 1 Establish the facts Identify conflicting or competing values
Prioritize core value of promoting and protecting public interest Promoting and protecting the public interest is the core value of pharmacy practice in New Brunswick. Registrants have a duty to embody this value and incorporate it in every aspect of their daily practice, not just when faced with a difficult ethical dilemma.
Registrants should habitually ask themselves: skills can be developed and improved with practice
Will what I am about to do result in promoting and protecting the health, wellbeing, safety and interests of the public and/or patient?
Will what I am about to do hold forth the independence, integrity and honour of the profession?
In determining the correct action, it emphasizes performing that action;
In the correct manner,
At the correct time,
With the correct people
And for the correct reasons
It is a methodology that results in the application of good judgement.
Judgement that is consistently motivated by a duty to promote and protect the public
interest, as well as judgement that holds forth the independence, integrity and honour of the profession.
Process of Values-Based Decision Making (00:20:54)
STEP 1: Establish the Facts
Understand the facts as completely and objectively as possible. The focus is to assemble the relevant factual information without judgement. This is known as identifying the context within which a decision is made.
Although the contextual facts are essential to VBDM, it is crucial to understand that the facts alone will not determine what should be done. Values ultimately determine the result of a given decision
STEP 2: Ensure Everyone Agrees on the Facts
Determine whether the relevant stakeholders agree on the facts or if there are any factual disagreements. This is important because the VBDM methodology cannot function unless there is agreement on the facts. At this point it is possible to have total agreement on the facts but to disagree about the appropriate course of action. This is a values conflict.
STEP 3: Identify the Conflicting or Competing Values of the Parties Involved
Identify and understand the values that are at play in the particular fact situation. The decisive factor in every decision, whether realized or not, is a ”judgement” based on a “value” (i.e., a value judgement). Sometimes these ‘value judgements’ are made instinctively, intuitively, or are the result of our beliefs and/or assumptions. Nevertheless, values are present in every decision and they ultimately determine what course of action will be pursued. Therefore, this step in the process is to understand and identify the values that
are “in play” within the context of the decision to be made.
STEP 4: Prioritize the Core Value of Promoting and Protecting the Public Interest (i.e., duties to the public and/or duties of conduct)
Analyze the values that are in conflict and then determine how to implement the value of promoting and protecting the public interest, in other words, prioritize the duties to the public and/or duties of conduct. All values conflicts should be resolved in favour of promoting and protecting the public interest and hold forth the independence, integrity and honour of the profession. After determining the decision that will promote and protect the public interest, the action must be performed in a contextually appropriate manner; that is, in the correct manner, at the correct time, with the correct people, and for the correct reasons. The exercise of good judgement is paramount
Bioethical Principles (00:26:27)
Beneficence:
Protect the interest of the patient to their benefit
The first foundational principle that forms and guides our commitment to serve and protect the best interests of our patients establishes the fact that our primary role and function as healthcare professionals is to benefit our patients. We need to remember that our patients seek our care and services because they believe and trust that we will apply our knowledge, skills and abilities to help make them better.
Non Maleficence (do no harm, and prevent harm from occurring)
The second foundational principle that guides our commitment to serve and protect the best interests of our patients addresses the reality that as we strive to benefit our patients we must be diligent in our efforts to do no harm and, whenever possible, prevent harm from occurring.
Components of practice that may be ethically fraught include stakeholder’’ financial interests influencing patient care, scope of practice boundaries, disclosing and documenting medication errors and near-misses, transitioning of care between providers or environments,
conscientious objection and allocating sufficient resources to provide comprehensive patient centered pharmaceutical care/medication management.
Respect for Persons (1:25:00)
Respect for persons is generally understood as the requirement that all patients be treated with dignity. There is an inherent vulnerability associated with being a patient and therefore
patients must be able to trust that the health care professional is motivated primarily by the core value of what is best for the patient. The registrant should consider the impact on the dignity of the patient. Would the potential action respect the inherent dignity of the patient or would it be an example of using the patient as a means to achieve an alternative goal? The focus should be on patient-centered care.Particularly challenging aspects of practice that this principle applies to include managing professional patient relationships, informed consent/refusal, substitute decision makers, advanced health directives, freedom of patient choice of pharmacy, and fiduciary duties of the professional.
Justice
The social aspect of the principle of justice is paramount. Justice includes the broader social obligations to protect the public interest and includes facilitating equitable access to services and conducting business ethically. Particularly challenging aspects of practice that justice impacts upon include allocation of rationed medication, patient incentives strategies, gifts, documentation, assumption and abrogation of responsibility, conflict of interest, dual relationships, advertising and referrals.
The four bioethical principles can be brought together with the VBDM methodology. As the professional answers yes or no to the two VBDM questions regarding duty to the patient and duty to the profession, the principles provide the ‘how’ to the answer. If the answer is ‘no’ then a statement can be made, “The individual value held by party X does not adhere to Y bioethical principle”. This is analogous to the statement of a drug-related problem within the Pharmaceutical Care Process.
Conflict of Interest (1:38:00)
A conflict of interest can be defined as any situation, interaction, or decision in which the professional’s personal and/or financial values (or the personal and/or financial values of another person) have the potential to influence or compromise the professional’s judgement. For the purposes of this Code of Ethics, there is no meaningful difference between an actual conflict of
interest and a perceived conflict of interest. The ethical management of the two is identical and typically starts with a “disclosure” to the relevant body, e.g., management or the New Brunswick College of Pharmacists (the College).Perceive conflict and actual conflict are treated the same
Conscientious Objection (00:54:40)
A conscientious objection is an opinion held by a professional that precludes participation in the delivery of an aspect of patient care. Pharmacy professionals may hold sincere beliefs of a conscientious nature that prevent the registrant from performing certain actions. If the service is permitted legally and prescribed by an authorized prescriber, then a claim to conscientious objection means that, “but for”, the conscientious objection the registrant would normally have a duty to provide the service.
that service has to be given to that patient
Fiduciary Relationship, Best Interest of the Patient, and Professional Boundaries (00:58:11)
The health professional and the patient are engaged in a therapeutic relationship. This relationship is characterized by a power imbalance. The professional is in a power position as a result of possessing specialized knowledge that the patient requires and the patient is vulnerable by virtue of being in need of that knowledge. A consequence of this power imbalance is that the professional owes the patient a fiduciary duty, in other words the professional has a duty to act in the patient’s best interest. This will require, amongst other considerations, the establishment of professional boundaries.
Informed Consent (01:00:15)
Informed consent requires the health professional to disclose the amount of information that a reasonable person in the patient’s position would want to know. Informed patient consent can be garnered only if the patient understands treatment benefits and risks. Consent can be implied or expressed
Mental Competency, Proxy and Substitute Decision Makers, and Advanced Health
Care Directives (1:02:07)
TLDR if a person is no longer to make sound decisions they can appoint a proxy to make decisions for them
On December 16th 2016, the New Brunswick Advanced Health Care Directives Act received Royal Assent. This Act allows anyone, who has the capacity, to make an advanced health care directive that would come into effect should that person lose his or her capacity to make health care decisions In addition to permitting advanced health care directives, this Act allows the patient to appoint a proxy to make decisions on behalf of the patient. The term proxy is used in this legislation; however, the term “substitute decision maker” is used in a parallel way in other Acts.
Patient-Centered Care (1:47:00)
Patient-centered care is an approach where health professionals and patients work together to meet the individual healthcare needs of the patient. Patient-centered care is a continual effort to ensure the needs and choices of the patient are being met. The concept of patient centered care is often expanded to include families as well; hence the term “patient and family-centered
care.” Regardless of the label, the insight of this approach is the meaningful inclusion of patients (and often families) in the health care decision making process.
Model for Ethical Decision Making
Ethical Issue Vs. Ethical Dilemma
What is an ethical issue?
A situation that raises an ethical question about what is right or wrong.
What is an ethical dilemma?
An ethical dilemma involves a situation which raises an ethical question about what is right or wrong which also involves a conflict of values.
conflict of value which is person on what you see
When faced with a ethical decision ask yourself the following:
What is the situation? What’s going on here really? What are the facts? What am I assuming?
Is this an ethical issue or an ethical dilemma?
Identify the people involved?
Identify any values or principles involved and any potential conflicts.
look beyond who or what is actually the problem
What are my motives in all of this?
Personal values/principles
Self-aware and honest about your motives and intentions
Are you motivated by your patient’s best interest?
Does a clear answer already exist?
What does the “rules” say regarding this situation?
Code of Ethics
Regulations/legislation
NBCP Policies or guidelines
keep pure motives
can you put feelings aside is it black and white?
Consult with a colleague and ask yourself the following:
How would I feel if I were the patient in this situation?
How would I feel if my action were made public?
What would happen if all healthcare professionals did this?
Ask around
talk to someone you trust and give them the raw situation
What is the best option and why?
Come up with 3 viable options
Doing nothing can be an option
Identify the pro’s and con’s of each option
Pick the option you consider to be the best and document why you consider it to be the best option
What have I learned from this?
Review your decision after some time has passed.
Was the outcome favorable? If it was, why? If it was not, why?
What could I do differently if faced with a similar situation?
sometimes people just leave even if everything was done right
 Knowt
Knowt