
Health Psychology: Introduction
Health Psychology
Health promoting behaviors
Preventive rather than reactive
How do people stay healthy? (emphasis on HOW)
HEALTH:
Complete state of physical, mental, and social well-being; not merely the absence of illness or disease, infirmity (WHO, 1948)
WELL-BEING: optimum state of health
Foci of Health Psychology
Health promotion and maintenance
Prevention and treatment of illness
Treatment: more cognitive behavioral therapy
Etiology and correlates of Health, Illness, and Dysfunction
Causes and factors
Improvement of the Healthcare System and formulation of Healthcare Policy
Development of Health Psychology
Mind-Body Relationship
Human prehistory
superstitious
Evil Spirits = illness
Treatment = exorcism (trephination)
Exorcism: physical corporal punishment; rationalizing torture
Trephination: drilling into skull to remove evil spirit; treatment for head injuries
Ancient Greeks: Humoral Theory of Illness
4 humors
blood (passionate personality)
black bile (sadness/melancholy personality)
yellow bile (angry disposition)
phlegm (laid-back personality)
Phlegmatic personality
Excess of a particular fluid = personality
Middle Ages
Divine punishment = illness
Treatment/Cure = physical/corporal punishment => penance (prayers and good works)
Continued exorcism but illness is divine punishment
Penance: undoing (defense mechanism)
Extended superstition
Renaissance
advancement of the technical basis of medicine
Invention of the microscope in the 1600s
Increased dependence on laboratory/physical findings as basis for health and illness
Clinical Eye: can use labs to confirm diagnosis but should not be too dependent on it
Modern Times
Psychodynamic Contributions
Sigmund Freud: Conversion Hysteria
Unconscious Conflict = physical disturbances that represent repressed psychological conflicts
Anna O. = diagnosed as having hysteria
Physical manifestation of a psychological conflict
Best treated with hypnosis
Psychosomatic Medicine
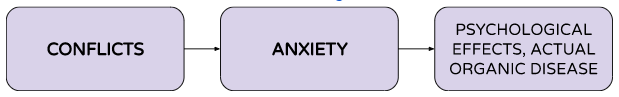
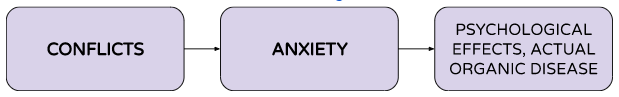
Flanders Dunbar (1930s) and Franz Alexander (1940s)
Conflicts led to anxiety and anxiety show up as physiological symptoms and sometime actual organic disease
Current Perspectives
Traditional East Asian medical philosophies and practices
Acupuncture or acupressure
Advancement of Neuroscience
Development of Psychoneuroimmunology (PNI)
Link between brain, physical symptoms and immunity
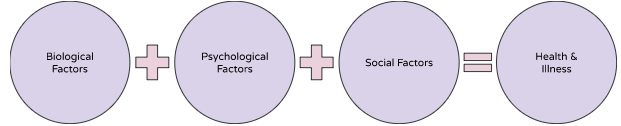
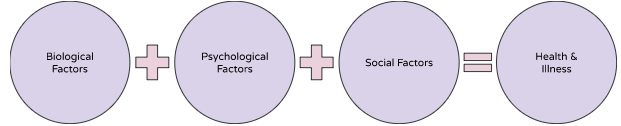
Biopsychosocial Model
Consider biological, psychological, and social factors
Help in planning treatment
Biomedical Model
ALL illness can be explained on the basis of aberrant somatic/physical bodily processes.
Psychological and social processes are IRRELEVANT to the disease process.
Potential Liabilities of the Biomedical Model:
Reductionistic single-factor model: reduces illness to simplistic cause
Implicitly assumes a MIND-BODY DUALISM: mind is separate from body; psyche cannot influence physical body
Emphasizes illness over health
Fails to address certain puzzles related to health (e.g., Given 6 people exposed to measles, why do only 3 develop it?)
Are there psychological and social factors that influence their health?
Advantages of the Biopsychosocial Model
Biological, psychological, and social processes are ALL important determinants of health and illness.
Mind and body cannot be distinguished in matters of health and illness.
Mind influences body, what we feel physically can influence our mind as well
How do biological, psychological, and social processes interact if biological processes are micro-level processes and psychological and social processes are macro-level processes?
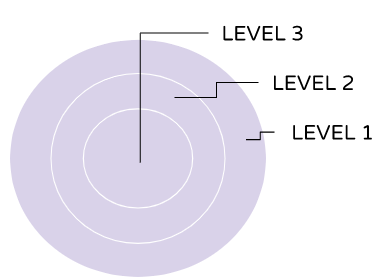
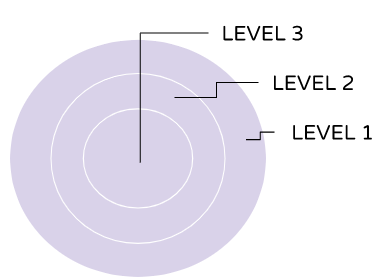
Systems Theory Approach
All levels of organization are linked to EACH OTHER hierarchically. A change in one level results in change in all the other levels.
One would affect another based on their level
Clinical Implications of the Biopsychosocial Model
Diagnoses and recommendations for treatment should consider interactions between and among all 3 factors (Bio, Psych, and Social factors)
Makes explicit the Patient-Practitioner relationship as well as its significance
The achievement and practice of health habits involve the interaction of all 3 factors as well.
Ex social factor: support of family of them getting treatment
Current trends in medicine, psychology, and the health care system
Cases in Health Psychology: The Case of “Nightmare Deaths”
1970s: influx of refugees to the United States from Laos, Cambodia, and Vietnam
Increase in sudden, unexpected, nocturnal deaths among males refugees from these countries.
INITIAL CLUES: Deaths occurred within the first few hours of sleep; victim was noted to gurgle (like drowning) and move restlessly in bed; most victims had a rare, genetically-based malfunction in the heart’s pacemaker (have irregular heartbeat); autopsies showed NO SPECIFIC CAUSE OF DEATH
“Nightmare Deaths”: Bangungot?
Psychosocial Clues:
ONLY MEN from particular ethnic backgrounds were affected
Deaths were clustered in certain families
Survivors and victims’ relatives seemed to recall a dream that foretold the death
Survivors said they experienced a severe night terror
Many victims were noted to have either: watched a violent TV show prior to retiring to bed, or had a family argument, or were exhausted from working 2 jobs or from having full-time work AND learning English.
Bangungot:
acute pancreatitis (pancreas releases hormones and goes to shock and organ failure)
Pancreas release hormones to digest the food
Sudden flood of hormones = inflammation in the pancreas
Cardiac arrest: part of multiple organ failure; heart dilates; cannot handle pumping blood efficiently
“Asian Death Syndrome” : genetics may play in the occurrence
Sleep paralysis: paradoxical sleep (you know you’re awake but you cannot move)
Parasomnia, abnormal sleep features
Death certificates = acute pancreatitis, multiple organ failures, septic shocks
The Need for Health Psychology
Changing patterns of illness: Acute vs. Chronic Illness
Examples of chronic illness: Lifestyle illness (hypertension, diabetes, high blood pressure), dementia
Advances in technology and research: Genetic research & PNI
Role of Epidemiology in Health Psychology: Morbidity and Mortality statistics
What health behaviors can help prevent COVID-19
Expanded Health Services: How can health psychologists help?
Increased medical acceptance of health psychologists
US, health psychologists work in clinics and hospitals; practice in tandem with psychiatrists, cardiologists
Teaching medical doctors how to encourage patients
Career Paths in Health Psychology
Practical Application: Medicine, Applied Medical Field
Therapies (speech, physical)
Research: public health, industrial/occupational health settings
Types of Research: correlational studies, prospective and retrospective studies, longitudinal research, case studies
Issues: promote health behaviors, prevent illness and accidents, control health care costs
Health Psychology: Introduction
Health Psychology
Health promoting behaviors
Preventive rather than reactive
How do people stay healthy? (emphasis on HOW)
HEALTH:
Complete state of physical, mental, and social well-being; not merely the absence of illness or disease, infirmity (WHO, 1948)
WELL-BEING: optimum state of health
Foci of Health Psychology
Health promotion and maintenance
Prevention and treatment of illness
Treatment: more cognitive behavioral therapy
Etiology and correlates of Health, Illness, and Dysfunction
Causes and factors
Improvement of the Healthcare System and formulation of Healthcare Policy
Development of Health Psychology
Mind-Body Relationship
Human prehistory
superstitious
Evil Spirits = illness
Treatment = exorcism (trephination)
Exorcism: physical corporal punishment; rationalizing torture
Trephination: drilling into skull to remove evil spirit; treatment for head injuries
Ancient Greeks: Humoral Theory of Illness
4 humors
blood (passionate personality)
black bile (sadness/melancholy personality)
yellow bile (angry disposition)
phlegm (laid-back personality)
Phlegmatic personality
Excess of a particular fluid = personality
Middle Ages
Divine punishment = illness
Treatment/Cure = physical/corporal punishment => penance (prayers and good works)
Continued exorcism but illness is divine punishment
Penance: undoing (defense mechanism)
Extended superstition
Renaissance
advancement of the technical basis of medicine
Invention of the microscope in the 1600s
Increased dependence on laboratory/physical findings as basis for health and illness
Clinical Eye: can use labs to confirm diagnosis but should not be too dependent on it
Modern Times
Psychodynamic Contributions
Sigmund Freud: Conversion Hysteria
Unconscious Conflict = physical disturbances that represent repressed psychological conflicts
Anna O. = diagnosed as having hysteria
Physical manifestation of a psychological conflict
Best treated with hypnosis
Psychosomatic Medicine
Flanders Dunbar (1930s) and Franz Alexander (1940s)
Conflicts led to anxiety and anxiety show up as physiological symptoms and sometime actual organic disease
Current Perspectives
Traditional East Asian medical philosophies and practices
Acupuncture or acupressure
Advancement of Neuroscience
Development of Psychoneuroimmunology (PNI)
Link between brain, physical symptoms and immunity
Biopsychosocial Model
Consider biological, psychological, and social factors
Help in planning treatment
Biomedical Model
ALL illness can be explained on the basis of aberrant somatic/physical bodily processes.
Psychological and social processes are IRRELEVANT to the disease process.
Potential Liabilities of the Biomedical Model:
Reductionistic single-factor model: reduces illness to simplistic cause
Implicitly assumes a MIND-BODY DUALISM: mind is separate from body; psyche cannot influence physical body
Emphasizes illness over health
Fails to address certain puzzles related to health (e.g., Given 6 people exposed to measles, why do only 3 develop it?)
Are there psychological and social factors that influence their health?
Advantages of the Biopsychosocial Model
Biological, psychological, and social processes are ALL important determinants of health and illness.
Mind and body cannot be distinguished in matters of health and illness.
Mind influences body, what we feel physically can influence our mind as well
How do biological, psychological, and social processes interact if biological processes are micro-level processes and psychological and social processes are macro-level processes?
Systems Theory Approach
All levels of organization are linked to EACH OTHER hierarchically. A change in one level results in change in all the other levels.
One would affect another based on their level
Clinical Implications of the Biopsychosocial Model
Diagnoses and recommendations for treatment should consider interactions between and among all 3 factors (Bio, Psych, and Social factors)
Makes explicit the Patient-Practitioner relationship as well as its significance
The achievement and practice of health habits involve the interaction of all 3 factors as well.
Ex social factor: support of family of them getting treatment
Current trends in medicine, psychology, and the health care system
Cases in Health Psychology: The Case of “Nightmare Deaths”
1970s: influx of refugees to the United States from Laos, Cambodia, and Vietnam
Increase in sudden, unexpected, nocturnal deaths among males refugees from these countries.
INITIAL CLUES: Deaths occurred within the first few hours of sleep; victim was noted to gurgle (like drowning) and move restlessly in bed; most victims had a rare, genetically-based malfunction in the heart’s pacemaker (have irregular heartbeat); autopsies showed NO SPECIFIC CAUSE OF DEATH
“Nightmare Deaths”: Bangungot?
Psychosocial Clues:
ONLY MEN from particular ethnic backgrounds were affected
Deaths were clustered in certain families
Survivors and victims’ relatives seemed to recall a dream that foretold the death
Survivors said they experienced a severe night terror
Many victims were noted to have either: watched a violent TV show prior to retiring to bed, or had a family argument, or were exhausted from working 2 jobs or from having full-time work AND learning English.
Bangungot:
acute pancreatitis (pancreas releases hormones and goes to shock and organ failure)
Pancreas release hormones to digest the food
Sudden flood of hormones = inflammation in the pancreas
Cardiac arrest: part of multiple organ failure; heart dilates; cannot handle pumping blood efficiently
“Asian Death Syndrome” : genetics may play in the occurrence
Sleep paralysis: paradoxical sleep (you know you’re awake but you cannot move)
Parasomnia, abnormal sleep features
Death certificates = acute pancreatitis, multiple organ failures, septic shocks
The Need for Health Psychology
Changing patterns of illness: Acute vs. Chronic Illness
Examples of chronic illness: Lifestyle illness (hypertension, diabetes, high blood pressure), dementia
Advances in technology and research: Genetic research & PNI
Role of Epidemiology in Health Psychology: Morbidity and Mortality statistics
What health behaviors can help prevent COVID-19
Expanded Health Services: How can health psychologists help?
Increased medical acceptance of health psychologists
US, health psychologists work in clinics and hospitals; practice in tandem with psychiatrists, cardiologists
Teaching medical doctors how to encourage patients
Career Paths in Health Psychology
Practical Application: Medicine, Applied Medical Field
Therapies (speech, physical)
Research: public health, industrial/occupational health settings
Types of Research: correlational studies, prospective and retrospective studies, longitudinal research, case studies
Issues: promote health behaviors, prevent illness and accidents, control health care costs
 Knowt
Knowt
