
Option: Immunology and disease
Important terminology
Word | Definition | Example |
|---|---|---|
Pathogenic | An organism that causes disease. | Tuberculosis is highly pathogenic. |
Infectious | A disease that is transmittable, either by inhalation, consumption or physical contact. | Influenza is highly infectious. |
Carrier | An infected person showing no symptoms but able to infect others. | Those infected with cholera become carriers. |
Disease reservoir | A long term host of a pathogen, with little to no symptoms, but able to infect others. | Those infected with cholera can act as disease reservoirs. |
Endemic | A disease occurring constantly, at a predictable rate, at a specific location. | Malaria is endemic in certain areas. |
Epidemic | Rapid spread of infectious disease to a large number of people in a small amount of time. | New influenza virus types can cause epidemics. |
Pandemic | Widespread occurrence of an infectious disease over a country or the world. | Spanish ‘flu was a devastating pandemic. |
Vaccine | A weakened or killed pathogen, or a toxic or antigen derived from it, which stimulates the immune system to cause a response without causing infection. | The smallpox vaccine led to it’s elimination. |
Antibiotic | A substance produced by a fungus which diminishes bacterial growth. | TB is treated by antibiotics. |
Antigen | A molecule which causes the body to produce an immune response. | Influenza antigens change rapidly. |
Antibody | A blood protein produced in response to and counteracting a specific antigen. | Human antibodies are produced in response to a vaccine, preventing further infection. |
Resistance | When pathogens become immune to the drugs used to kill and treat them. | Resistance in present in TB bacteria. |
Vector | A person, animal or microbe that carries and transmits an infectious pathogen into another person. | Those infected with smallpox become vectors. |
Toxin | A small molecule, such as a peptide, produced in cells or organisms that causes disease following contact or absorption. These often affect macromolecules. | Malaria produces toxins which affect red blood cells. |
Disease
Body as a host
Humans can be seen as colonies, not individuals.
This is because a similar amount of pathogenic species are in our body to individual cells.
We carry microbes, such as fungi, protista, and 1000 bacterial species in our gut flora.
We can also carry other parasites, such as insects, fleas, or worms.
Parasites have the potential to cause disease if they secrete toxins, have too high population or are transferred to an inappropriate part of the body, but many are necessary:
E.coli for vitamin K synthesis in the large intestine.
It can cause gastrointestinal disease in the stomach or small intestine.
Mites in hair follicles of eyelashes eat dead cells.
They stick to eye makeup, which means not removing mascara can cause their population to build up and cause inflammation.
Entamoeba is a protocistan which grazes on dead skin cells on gums.
If teeth are not brushed enough, they build up and cause gingivitis.
Therefore, in a healthy body there is an ecological balance.
Important diseases
Cholera
This is caused by the gram negative, comma shaped bacteria Vibrio cholerae.
It can only reproduce inside human hosts.
It in endemic in parts of the world.
Transmission
It is transmitted through contaminated food and water.
Those infected become carriers, and reservoirs of disease, which can contaminate other water supplies and spread the disease.
Infection
A toxin is produced in the small intestine, which affects the chlorine channel proteins, or CFTR.
This prevents water, and many ions; chloride, sodium, potassium and bicarbonate, from entering the blood.
This causes severe, watery diarrhea.
This leads to dehydration, causing blood pressure to fall dramatically and the patient to potentially die within hours.
Prevention
It can be prevented by good hygiene and sanitation, such as improved sewage treatment, water purification, safe food handling and regular hand washing.
There is a temporary vaccine, but it is only given to those at high risk.
Treatment
There is two strands:
Water and ions are replaced by giving patients electrolytes, orally or intravenously in severe cases.
Bacteria are treated with antibiotics.
Tuberculosis (TB)
Tuberculosis is caused by the bacillus bacterium Mycobacterium tuberculosis.
It is named for the tubercles, or nodules of dead and damaged cells in the lungs of those infected.
These can contain gas filled cavities, which are easily seen in X-rays.
Transmission
It spreads rapidly by aerosol transmission - the inhalation of bacteria-laden droplets from the coughs and sneezes of those infected.
It is again a public health concern due to it’s rapid spread in cities, especially as those with HIV/AIDs have weakened immune systems.
Infection
This mainly affects the lungs, causing chest pain and phlegm (sputum) to be coughed up, which often contains blood.
This can also infect neck lymph nodes, causing swelling.
Those infected lose their appetite and develop a fever.
Prevention
The BCG vaccine is given to babies, and if a skin test proves negative, to people up to the age of 16.
It is made from an attenuated (weakened) strand of a related bacterium, M.bovis, and named after the scientists who discovered it - bacillus of Calmette and Guerin.
It provides around 75% protection, but only for 15 years.
It is less effective than adults, and only given to those at risk.
Treatment
It is treated with a long course of antibiotics, although it does show some resistance.
Smallpox
It is caused by a DNA containing virus, Variola major.
It is completely extinct following vaccination campaigns, and only remains in high security labs.
Ethical debates are ongoing about the total extinction of the virus.
Transmission
It is inhaled, or transmitted via saliva from close contact with an infected person.
Infection
It enters small blood vessels in the skin, mouth and throat, and is dispersed around the body.
It causes a rash and fluid-filled blisters, which leave scars on survivors.
Some survivors also suffer blindness and limb deformities.
Prevention
The smallpox vaccine is made with live Vaccinia virus (cowpox) and is highly effective.
Prior to this, infected people were isolated.
Influenza
There are three subgroups of the virus, known as flu A, B and C.
The most well known is flu A.
It contains RNA as it’s genetic material, but has 8 single strands instead of 1.
The virion is surrounded by a phospholipid envelope, derived from the host cell’s surface membrane.
It contains two important proteins, which are antigens:
Haemagglutinin (H) has a role in the virus entering a host cell.
Neuraminidase (N) has a role in the virus leaving the host cell.
When a new strain appears, with new proteins on it’s surface, the human immune system cannot provide adequate protection.
This can cause pandemics, such as Spanish flu, one of the deadliest natural disasters in human history, killing 4% of the population.
Transmission
It can infect many species, such as avian and swine flus which can infect humans.
Chickens and pigs are known as animal reservoirs for virus infection - a source of a new infection produced when an animal virus mutates and becomes infectious to humans.
It is inhaled in droplets from coughs and sneezes, via aerosol transmission.
The virus has a mucus protecting it, and it survives better in dry and low UV light conditions, therefore it survives better in winter than summer.
Infection
It attacks mucous membranes, especially in the upper respiratory tract, causing a sore throat, cough and fever.
Prevention
This can be done via regular hand washing, using and discarding tissues for coughs and sneezes, quarantines and vaccines.
However, vaccine success is variable due to the surface antigens changing, meaning new vaccines are needed annually.
Antigenic types
This is different individuals of the same pathogenic species with differing surface proteins, and therefore antibodies.
There are two main ways these differences originate:
Antigenic drift:
Due to there being no RNA proofreading enzymes, on average a virion has a new mutation after every round of replication.
This causes a gradual change in surface proteins, known as antigenic drift.
Antigenic shift:
‘Flu has 16 types of haemagglutinin, with 1, 2 and 3 most common in humans.
It has 9 types of neuraminidase, with 1 and 2 most common in humans.
If a single cell is infected by viruses with different combinations of H and N, the separate strands of RNA can recombine, causing different virus types.
This can cause epidemics.
Malaria
It is caused by a protocistan - Plasmodium. This has five malaria causing species, with P. falciparum causing the most deaths and P. vivax being another major killer.
It is transmitted by over 100 species of Anopheles mosquitoes, when they pierce the skin to make a blood meal.
Only females are vectors, however, as males feed on plant nectar instead.
It occurs in habitats that support the Anopheles mosquito, making it endemic in sub-tropical regions.
It can be considered an epidemic during wet seasons.
It can be seen as a pandemic, as millions are affected worldwide and more are killed than any other infection, despite years of research and drug development.
Transmission
When an infected mosquito takes a blood meal, Plasmodium sporozoites in the saliva are injected into the human.
These travel to the liver and reproduce asexually in the liver cells, producing merozoites.
Merozoites are released into the blood and infect red blood cells, where more asexual reproduction occurs.
Red blood cells burst and release more merozoites, which infect more red blood cells.
This repeats every few days, causing fever symptoms when the fever occurs.
Some of these become gametocytes, which are taken into a mosquito when it takes blood from an infected person.
These produce zygotes, which develop into the infective stage known as sporozoites.
These migrate from the mosquito’s gut to the salivary glands.
Treatment
Drugs can only effect Plasmodium when it is outside of red blood cells and liver cells and in the blood, limiting their effectiveness.
Quinine was developed in the 17th century, but has lost effectiveness.
Artemisinin is a newer drug, but has documented resistance.
Normally, malaria is treated with artemisinin and a combination of other drugs, because it is unlikely that Plasmodium will have resistance to all the drugs.
Prevention
Mosquito behaviour is countered by:
Sleeping under mosquito nets, as they feed most often during dusk and dawn.
These nets are often treated with pyrethroid insecticide to kill any mosquitos.
Walls are treated with insecticide, as mosquitos often rest on walls after feeding.
Drain or cover stagnant water, to prevent mosquitoes from laying eggs.
Alternatively, a film of fish oil is applied to lower surface tension, preventing the larvae from piercing the surface to obtain oxygen.
Biological control:
Fish are introduced to the water, causing the larvae to be consumed.
Mosquitoes are infected with Wolbachia bacterium, which blocks Plasmodium development.
Male mosquitos are sterilised via X-rays, therefore no offspring are produced.
Virus pathogenicity and reproduction
Virus are sometimes described as the ‘ultimate parasite‘ as they are inert outside of living cells.
They show no life characteristics, except for when they are replicated within a host cell.
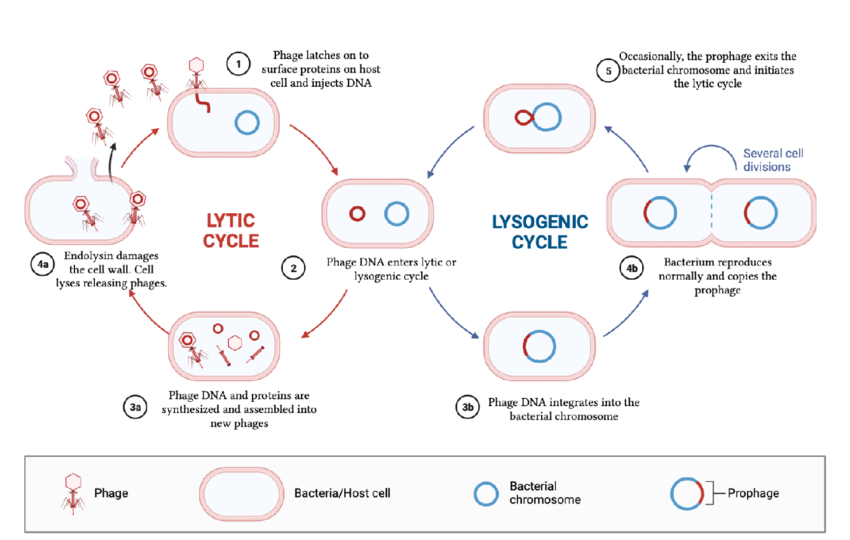
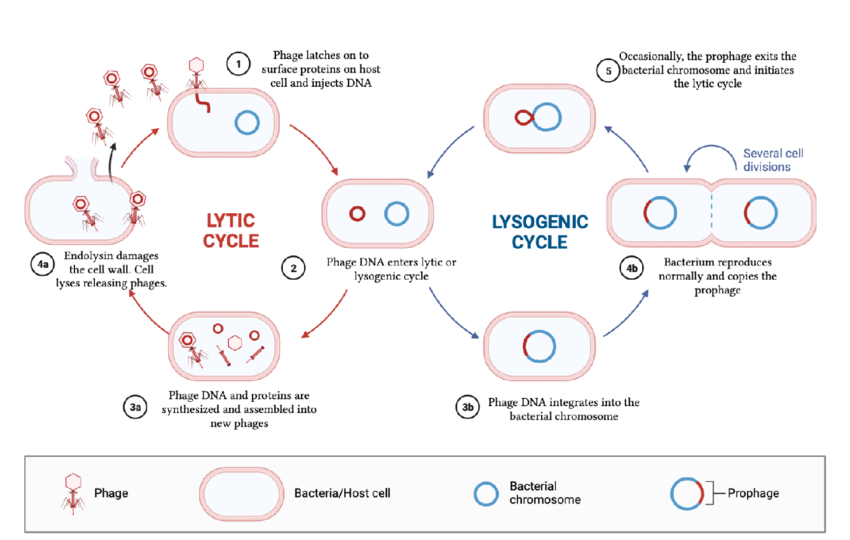
There are two cycles a pathogen can follow:
The lytic cycle, where a virus immediately reproduces using the host’s metabolism to copy their own nucleic acids (DNA or RNA) and synthesise a new protein coat.
This cycle occurs in 4 steps:
The virion attaches to a cell.
Viral nucleic acid is injected into the cell, leaving the protein coat outside.
The nucleic acid and capsid protein are synthesised using the host cell metabolism and they assemble to make mature virus particles.
Cell lysis then releases the viruses.
Some viruses are lysogenic, meaning they integrate their nucleic acid into the host cell genome, and can remain there for many cell generations with no clinical effect.
They will then enter the lytic cycle later when triggered, producing symptoms.
Viruses can be pathogenic in many ways:
Cell lysis - In bacteria, the pressure of new bacteriophage particles inside the cell causes it to burst.
In animal cells, inflammation cause by T-lymphocytes or antibodies causes lysis.
An example is rhinovirus, a type of common cold, which lyses cells in the upper respiratory tract.
Toxins - Viral components and their by-products can be toxic. The mechanisms for this are not fully understood, but examples include:
Measles virus causing chromosome fusion.
Herpes virus causing cell fusion.
Viral proteins inhibiting
RNA, DNA and protein synthesis.
Cell transformation - Viral DNA can integrate into the host chromosome.
If the DNA inserts into a pro-oncogene or tumour suppressor gene it can cause rapid controlled mitosis, making it cancerous.
An example is HPV, where cervical cancer is caused by entering into the TP53 tumour suppressor gene.
Immune suppression - This can include:
Suppression of reactions that cause B and T lymphocytes to mature.
Reduction of antibody formation.
An example is HIV, which destroys a group of T helper cells, preventing B lymphocytes from making antibodies.
This makes those with HIV immuno-compromised and highly susceptible to infection.
Antibiotics
Types
Compounds that inhibit the growth of bacteria are known as antimicrobials. This includes:
Antiseptics used on living tissue, such as Dettol.
Disinfectants used on non-living surfaces, such as bleach.
Antibiotics.
Antibiotics are produced by fungi, and only act on bacteria, not viruses and eukaryotic cells.
They therefore treat without causing any harm to the patient.
There are two types of spectrums for bacteria:
Broad-spectrum - Affect many different Gram-positive and Gram-negative species, such as ampicillin and tetracycline.
Narrow-spectrum - More selective, such as only killing Gram-positive bacteria, like penicillin.
Antibiotics also affect different aspects of bacterial metabolism:
Bactericidal antibiotics kill bacteria, such as penicillin.
Bacteriostatic antibiotics prevent bacterial multiplication, but do not kill bacteria. Bacteria would return to normal when the antibiotic is not present.
Examples include sulphonamides, which are competitive enzyme inhibitors and tetracycline.
Bacterial cell walls
All bacteria have a peptidoglycan, or murein, cell wall, but this varies on size based on whether they are gram positive or negative.
It contains polysaccharide and short chains of amino acids.
Transpeptidase enzymes cross-link polysaccharide molecules by attaching them to side chains of amino acids.
This makes the cell wall strong, gives the cell it’s shape and allows it resist bursting via osmosis.
Gram-positive bacteria have a thick layer of murein, making up over 90% of their cell wall.
Pores in this layer close during the depolarization stage of the gram stain test, so the CV is retained within the cell.
Safranin then turns the violet colour to a purple.
Murein is accessible to molecules outside the cell, making it susceptible to lysozymes and penicillin.
Gram-negative bacteria have a thin layer or murein, no more than 10% of the cell wall. This is surrounded by lipoprotein and lipopolysaccharide.
These lipid molecules are disrupted by the decolorization stage of the Gram staining, causing CV to leak out the cell and leaving them unstained.
Safarin then turns these cells red.
This layer protects the murein from antimicrobial agents, such as lysozymes and penicillin.
Antibiotic mechanisms
Penicillin
This is released by the penicillium fungus when its growth is inhibited and it is under high stress.
This is bactericidal, as it bursts cells by breaking their cell walls.
Originally, it was mass produced from P. notatum, but now high yielding strains of P. chrysogenum are used.
It is grown aerobically in industrial fermenters and penicillin is then purified for use.
Penicillin is unique from other antibiotics as it is small enough to penetrate right through mureine, so the whole thickness of the cell wall is affected.
The first penicillin was penicillin G, which had to be injected as stomach acid broke it down.
Penicillin V and other derivatives, such as ampicillin, can be taken orally.
Penicillin works in 5 steps:
It readily diffuses through the cell wall of Gram-positive bacteria and it enters some Gram-negative bacteria through surface molecules called porins.
This makes it a narrow spectrum antibiotic.
Bacteria continues to break down and remake it’s cell wall.
Penicillin prevents this via acting as an enzyme inhibitor the the DD-transpeptidase enzyme, which makes cross-links between amino acid side chains joining peptidoglycan molecules.
This enzyme is also known as the penicillin binding protein.
The cell wall continues to break down via hydrolysis, meaning more is lost than gained.
Precursors for the cell wall creation also build up and are hydrolysed, as they are not being used in cell wall production.
The cell wall then becomes so weakened, that water entering the cell via osmosis causes too much pressure for the cell wall, which lyses.
Tetracycline
Produced by the Streptomyces fungus, and is a broad spectrum antibiotic.
It is also bacteriostatic as it inhibits protein synthesis.
It has a wide medical use, and is used for acne, common infections (such as Chlamydia), anthrax and plague.
It has even been shown to have activity against eukaryotic parasites, such as Plasmodium.
However, many bacteria are beginning to shown resistance against Tetracycline.
It works in 3 steps:
It diffuses and is pumped into bacteria cells.
It then binds to small (30S) ribosome subunit and blocks tRNA attachment in the second position, the A site, so no new amino acids can be added to a polypeptide chain.
This is reversible, meaning it has a bacteriostatic effect.
Antibiotic overuse
Antibiotics have been used throughout history, especially during wars.
Now, however, antibiotics are being used as a preventive measure for infection, meaning they are used continuously and not in response to infection.
This is because productivity is increased when an animal has more energy for growth over fighting infection.
However, some bacteria will develop a resistance to antibiotics, giving them a selective advantage over un-immune bacteria.
They will then reproduce and pass on the immunity allele, building a resistant population.
There are two sources of these antibiotic resistant alleles:
Every time bacterial DNA replicates, mutations conferring resistance may arise.
Bacteria replicate rapidly in suitable conditions, increasing their rate of mutation.
Bacteria can acquire plasmids with antibiotic resistant alleles from their environment.
These then replicate inside a bacterium, and are passed onto daughter cells when the bacteria replicates.
Examples of resistance against penicillin include:
Secreting B-lactamase, which is an enzyme which degrades penicillin.
Altered DD-transpeptidase enzyme, which prevents penicillin from binding.
Penicillin entry is reduced via fewer or smaller porins.
Examples of resistance against tetracycline include:
Tetracycline is pumped out of cells.
Tetracycline is dislodged from it’s binding.
Tetracycline is prevented from ever attaching to a ribosome.
Without antibiotics, antibiotic resistant bacteria have a selective disadvantage due to energy required to synthesise these proteins. This would make it more likely to die.
Therefore, the continuous use of antibiotics gives these bacteria this advantage, increasing their population.
Several bacteria have begun to show resistance, such as leprosy, TB and gonorrhea.
Some have even shown resistance to multiple bacteria, such as:
MRSA - Methicillin-resistant Staphylococcus aureus.
This is resistant to penicillin and all it’s derivatives, and it treated with vancomycin.
Clostridium difficile - Severe cases are also treated with vancomycin.
New antibiotics need to be developed in order to combat infection post-surgery, otherwise bacteria will become life threatening again.
Immune response
The immune system exists to resist disease.
There are physical barriers to protect against the entry of pathogens.
if these fail, there are cellular and chemical responses.
Every day, huge numbers of microorganisms invade the body, most of the time individuals remain healthy.
It does this by detecting foreign ‘non-self’ antigens and distinguishing them from ‘self‘ antigens.
Innate immune system
These are natural barriers that resist infection:
The skin covers the external surface of the body, except as openings such as the mouth and eyes.
Keratin in epidermal cells makes skin waterproof.
Collagen in the connective tissue of the dermis, maintained by vitamin C, makes the skin tough.
The skin flora, or microbiota, comprises bacteria and fungi which outcompete pathogenic strains.
Unlike pathogens, these are hard to wash off and so regular washing is a good technique to remove pathogens.
Inhaled air is a source of microorganisms and their spores.
The mucus traps them and cilia of epithelial cells lining the respiratory passages brings them up to the opening of the oesophagus, where they are swallowed.
When the skin barrier is breached:
If capillaries are broken, blood clots prevent the entry of microbes.
Inflammation sets in, where increased blood flow towards the site of infection brings in large numbers of phagocytic cells .
The broken capillaries heal and the raised temperature is unfavourable to microbes.
Adaptive immune system
‘Adaptive‘ means the body produces a specific response to each antigen, so the body is adapting.
Lymphocytes provide this response, and are derived from stem cells in the bone marrow, and their precise role depends on their subsequent location.
Adaptive response
This has two components.
Humoral response
This results in the production of antibodies.
B lymphocytes mature in the spleen and lymph nodes.
Receptors on their cell membranes respond to a foreign protein in the bloodstream, and they divide making:
Plasma cells, which release antibodies.
Memory cells, which remain dormant in the circulation, and when the same antigen is encountered divide to form more B lymphocytes.

Antibodies are Y shaped glycoprotein molecules, known as immunoglobulins.
They have a quaternary structure, as each molecule is made up of four polypeptides held together by disulphide bonds.
The variable portions are specific to each antigen, and are at the end of the molecule.
The inner Y is heavy, while the outer parts are light
An antigen molecule binds to an antibody and each antibody molecule can bind to two antigen molecules.
Molecules with antigens on their surfaces are clumped together - they agglutinate (firmly stick together to form a mass).
Cell mediated response
This is the activation of phagocytic cells, B lymphocytes and T lymphocytes.
T lymphocytes activate in the thymus gland.
Receptors on their cell membranes respond to antigens and they divide, making:
T memory cells, which remain dormant in the circulation, and when the same antigen is encountered divide to form more T lymphocytes.
T killer or cytotoxic T cells, which kill pathogens with the antigen by lysing them.
T helper cells, which release chemicals including cytokines.
These cytokines stimulate:
Phagocytic cells, including macrophages, monocytes and neutrophils, which engulf pathogens and digest them.
B and T lymphocytes to undergo clonal expansion, which is when they divide repeatedly into genetically identical cells, forming a large population of cells specific to one antigen.
These cells differentiate into the various classes of lymphocyte.
B lymphocytes to make antibodies.
Fighting infection
Primary immune response
After first exposure to an antigen, there is a short latency period in which macrophages engulf the foreign antigen, or the cell, or virus to which it is attached.
They incorporate the antigenic molecules into their own cell membrane, a process known as antigen presentation, making macrophages a type of antigen-presenting cell.
T helper cells then detect these antigens and respond by secreting cytokines.
The B plasma cells secrete antibodies for around 3 weeks, subsiding symptoms of infection.
Secondary immune response
This relies on memory cells, and may protect against an identical antigen, even many decades after first exposure.
Upon re-exposure to even a small amount of an antigen, after a short latency period, memory cells undergo clonal expansion.
This is faster than the primary response.
Antibodies are made quicker, and are up to a 100x more concentrated than in the primary response.
They remain at high concentrations in the circulation for longer, and therefore no symptoms develop.
Active and passive immunity
Active immunity
This is when the body makes its own antibodies, stimulated by either infection or vaccination.
This is long lasting as the response produces memory cells.
Vaccination
Vaccination triggers humoral and cell-mediated responses, even though no harmful pathogen is present.
Types of vaccines include:
Antigens isolated from the pathogen, such as the HPV vaccine.
Weakened or attenuated (reduced in force, effect or value) strains of the pathogen, such as the MMR combined vaccine.
Inactive or killed pathogen, such as the whooping cough vaccine.
Inactivated toxin, such as the tetanus vaccine.
The vaccine is recognised as ‘non-self‘ by the body, and the immune system behaves as if it is a normal pathogen, meaning it produces it’s own antigens.
Over time, however, memory cells decrease if the body is not exposed to the antigen again.
In some cases, one or more boosters are given, such as the tetanus booster every 10 years.
This is further exposure to the vaccine and the response is faster, bigger and longer lasting than the first.
More memory cells are then made, meaning the body is protected for longer.
Passive immunity
This is when the body receives antibodies from another individual.
This can occur naturally, such as:
From the mother to the foetus across the placenta.
To the baby in breast milk.
Antibody injections, also known as Ig (immunoglobulin) replacement therapy are given in various situations, such as:
When rapid resistance is needed, and there is no time for active immune response to develop.
Example is when someone is bitten by a rabies infected animal, a wound which has a high risk of tetanus, or an urgent visit to a part of the world where an infection is endemic.
Cases of PIDD (primary immune deficiency disease) and cases of acquired immunity conditions, such as HIV, where patients do not make enough antibodies and cannot protect themselves against pathogens.
The protection given by injected antibodies is short lived because the body mounts an immune response against them as they are recognised as foreign.
Vaccine effectiveness
Vaccines can vary in effectiveness, and will have different schedules to provide long lasting immunity.
The HPV vaccine can come in only one dose, while the meningitis B is required 3 times and influenza vaccines are given annually to older people.
For a vaccination to be successful, it must:
Have a highly immunogenic (able to produce an immune response) antigen, meaning a single dose of the vaccine would cause a strong response from the immune system.
This would mean a large number of specific antibodies would be rapidly made, such as the smallpox vaccine using cowpox.
There should only be one antigenic type (serotype) of the pathogen, such as Rubella, where all Rubella viruses have the same surface antigens, meaning only one vaccine is required and antibodies formed can attack all of them.
The flu virus has many serotypes due to genetic recombination and frequent mutation, meaning memory cells produced from first exposure may not be stimulated.
Different vaccines are therefore needed for each antigenic type, and small changes in the antigens generated by mutation may mean that a vaccine may not be totally effective.
Ethical considerations
Vaccines are highly successful, and no other method is as effective.
For some diseases, it can be the only reliable means of protection.
Additionally, the more vaccinated, the less live pathogens in the population, meaning that fewer people will become infected in the future.
This controls the spread of disease, so even those non-vaccinated have some protection.
This is known as community or herd immunity and requires a particular proportion of people to be vaccinated.
If the proportion drops below this significant value, infection can spread.
This can be seen as a moral argument to get vaccinated.
But not everyone is vaccinated, for many reasons:
Vaccinations may not be medically advised for those:
Immunocompromised, for example they have a faulty spleen.
Taking chemotherapy.
Living with HIV-AIDS.
Very old.
Very ill in hospital.
Alternatively, some people choose not to vaccinate themselves or their children for other reasons, such as:
Religious objections.
A preference for natural and alternative medicine.
Mistrust of pharmaceutical companies who manufacture the vaccines.
Safety fears.
Cost effectiveness
Health authorities must consider whether the cost of vaccinations schemes outweighs the benefit.
For dangerous conditions, such as measles, vaccination is advised for all, but for influenza it is only recommended for target groups.
Overall, however, vaccination is considered cost effective due to the costs of treatment.
Compulsory vs voluntary vaccinations
The policy in the UK is that the government cannot infringe on the right of the individual to choose their own medication, therefore vaccination is not compulsory.
This becomes complicated in terms of health workers and children:
Health workers have a duty to not harm, which may be contravened if they are not vaccinated.
Children have decisions made by their parents, meaning they could be harmed by their parent’s poor decisions.
Places where vaccines are compulsory argue it is for the right of a society to protect itself, and prevent harm to others caused by anti vax individuals.
Side effects
This is sometimes used as a reason to not vaccinate children.
Common ones for vaccines include; soreness at injection site, fever, fatigue and muscle or joint pain.
Serious side effects have been documented but are extremely rare, but attention from mass media (availability heuristic) makes them seem more common.
Option: Immunology and disease
Important terminology
Word | Definition | Example |
|---|---|---|
Pathogenic | An organism that causes disease. | Tuberculosis is highly pathogenic. |
Infectious | A disease that is transmittable, either by inhalation, consumption or physical contact. | Influenza is highly infectious. |
Carrier | An infected person showing no symptoms but able to infect others. | Those infected with cholera become carriers. |
Disease reservoir | A long term host of a pathogen, with little to no symptoms, but able to infect others. | Those infected with cholera can act as disease reservoirs. |
Endemic | A disease occurring constantly, at a predictable rate, at a specific location. | Malaria is endemic in certain areas. |
Epidemic | Rapid spread of infectious disease to a large number of people in a small amount of time. | New influenza virus types can cause epidemics. |
Pandemic | Widespread occurrence of an infectious disease over a country or the world. | Spanish ‘flu was a devastating pandemic. |
Vaccine | A weakened or killed pathogen, or a toxic or antigen derived from it, which stimulates the immune system to cause a response without causing infection. | The smallpox vaccine led to it’s elimination. |
Antibiotic | A substance produced by a fungus which diminishes bacterial growth. | TB is treated by antibiotics. |
Antigen | A molecule which causes the body to produce an immune response. | Influenza antigens change rapidly. |
Antibody | A blood protein produced in response to and counteracting a specific antigen. | Human antibodies are produced in response to a vaccine, preventing further infection. |
Resistance | When pathogens become immune to the drugs used to kill and treat them. | Resistance in present in TB bacteria. |
Vector | A person, animal or microbe that carries and transmits an infectious pathogen into another person. | Those infected with smallpox become vectors. |
Toxin | A small molecule, such as a peptide, produced in cells or organisms that causes disease following contact or absorption. These often affect macromolecules. | Malaria produces toxins which affect red blood cells. |
Disease
Body as a host
Humans can be seen as colonies, not individuals.
This is because a similar amount of pathogenic species are in our body to individual cells.
We carry microbes, such as fungi, protista, and 1000 bacterial species in our gut flora.
We can also carry other parasites, such as insects, fleas, or worms.
Parasites have the potential to cause disease if they secrete toxins, have too high population or are transferred to an inappropriate part of the body, but many are necessary:
E.coli for vitamin K synthesis in the large intestine.
It can cause gastrointestinal disease in the stomach or small intestine.
Mites in hair follicles of eyelashes eat dead cells.
They stick to eye makeup, which means not removing mascara can cause their population to build up and cause inflammation.
Entamoeba is a protocistan which grazes on dead skin cells on gums.
If teeth are not brushed enough, they build up and cause gingivitis.
Therefore, in a healthy body there is an ecological balance.
Important diseases
Cholera
This is caused by the gram negative, comma shaped bacteria Vibrio cholerae.
It can only reproduce inside human hosts.
It in endemic in parts of the world.
Transmission
It is transmitted through contaminated food and water.
Those infected become carriers, and reservoirs of disease, which can contaminate other water supplies and spread the disease.
Infection
A toxin is produced in the small intestine, which affects the chlorine channel proteins, or CFTR.
This prevents water, and many ions; chloride, sodium, potassium and bicarbonate, from entering the blood.
This causes severe, watery diarrhea.
This leads to dehydration, causing blood pressure to fall dramatically and the patient to potentially die within hours.
Prevention
It can be prevented by good hygiene and sanitation, such as improved sewage treatment, water purification, safe food handling and regular hand washing.
There is a temporary vaccine, but it is only given to those at high risk.
Treatment
There is two strands:
Water and ions are replaced by giving patients electrolytes, orally or intravenously in severe cases.
Bacteria are treated with antibiotics.
Tuberculosis (TB)
Tuberculosis is caused by the bacillus bacterium Mycobacterium tuberculosis.
It is named for the tubercles, or nodules of dead and damaged cells in the lungs of those infected.
These can contain gas filled cavities, which are easily seen in X-rays.
Transmission
It spreads rapidly by aerosol transmission - the inhalation of bacteria-laden droplets from the coughs and sneezes of those infected.
It is again a public health concern due to it’s rapid spread in cities, especially as those with HIV/AIDs have weakened immune systems.
Infection
This mainly affects the lungs, causing chest pain and phlegm (sputum) to be coughed up, which often contains blood.
This can also infect neck lymph nodes, causing swelling.
Those infected lose their appetite and develop a fever.
Prevention
The BCG vaccine is given to babies, and if a skin test proves negative, to people up to the age of 16.
It is made from an attenuated (weakened) strand of a related bacterium, M.bovis, and named after the scientists who discovered it - bacillus of Calmette and Guerin.
It provides around 75% protection, but only for 15 years.
It is less effective than adults, and only given to those at risk.
Treatment
It is treated with a long course of antibiotics, although it does show some resistance.
Smallpox
It is caused by a DNA containing virus, Variola major.
It is completely extinct following vaccination campaigns, and only remains in high security labs.
Ethical debates are ongoing about the total extinction of the virus.
Transmission
It is inhaled, or transmitted via saliva from close contact with an infected person.
Infection
It enters small blood vessels in the skin, mouth and throat, and is dispersed around the body.
It causes a rash and fluid-filled blisters, which leave scars on survivors.
Some survivors also suffer blindness and limb deformities.
Prevention
The smallpox vaccine is made with live Vaccinia virus (cowpox) and is highly effective.
Prior to this, infected people were isolated.
Influenza
There are three subgroups of the virus, known as flu A, B and C.
The most well known is flu A.
It contains RNA as it’s genetic material, but has 8 single strands instead of 1.
The virion is surrounded by a phospholipid envelope, derived from the host cell’s surface membrane.
It contains two important proteins, which are antigens:
Haemagglutinin (H) has a role in the virus entering a host cell.
Neuraminidase (N) has a role in the virus leaving the host cell.
When a new strain appears, with new proteins on it’s surface, the human immune system cannot provide adequate protection.
This can cause pandemics, such as Spanish flu, one of the deadliest natural disasters in human history, killing 4% of the population.
Transmission
It can infect many species, such as avian and swine flus which can infect humans.
Chickens and pigs are known as animal reservoirs for virus infection - a source of a new infection produced when an animal virus mutates and becomes infectious to humans.
It is inhaled in droplets from coughs and sneezes, via aerosol transmission.
The virus has a mucus protecting it, and it survives better in dry and low UV light conditions, therefore it survives better in winter than summer.
Infection
It attacks mucous membranes, especially in the upper respiratory tract, causing a sore throat, cough and fever.
Prevention
This can be done via regular hand washing, using and discarding tissues for coughs and sneezes, quarantines and vaccines.
However, vaccine success is variable due to the surface antigens changing, meaning new vaccines are needed annually.
Antigenic types
This is different individuals of the same pathogenic species with differing surface proteins, and therefore antibodies.
There are two main ways these differences originate:
Antigenic drift:
Due to there being no RNA proofreading enzymes, on average a virion has a new mutation after every round of replication.
This causes a gradual change in surface proteins, known as antigenic drift.
Antigenic shift:
‘Flu has 16 types of haemagglutinin, with 1, 2 and 3 most common in humans.
It has 9 types of neuraminidase, with 1 and 2 most common in humans.
If a single cell is infected by viruses with different combinations of H and N, the separate strands of RNA can recombine, causing different virus types.
This can cause epidemics.
Malaria
It is caused by a protocistan - Plasmodium. This has five malaria causing species, with P. falciparum causing the most deaths and P. vivax being another major killer.
It is transmitted by over 100 species of Anopheles mosquitoes, when they pierce the skin to make a blood meal.
Only females are vectors, however, as males feed on plant nectar instead.
It occurs in habitats that support the Anopheles mosquito, making it endemic in sub-tropical regions.
It can be considered an epidemic during wet seasons.
It can be seen as a pandemic, as millions are affected worldwide and more are killed than any other infection, despite years of research and drug development.
Transmission
When an infected mosquito takes a blood meal, Plasmodium sporozoites in the saliva are injected into the human.
These travel to the liver and reproduce asexually in the liver cells, producing merozoites.
Merozoites are released into the blood and infect red blood cells, where more asexual reproduction occurs.
Red blood cells burst and release more merozoites, which infect more red blood cells.
This repeats every few days, causing fever symptoms when the fever occurs.
Some of these become gametocytes, which are taken into a mosquito when it takes blood from an infected person.
These produce zygotes, which develop into the infective stage known as sporozoites.
These migrate from the mosquito’s gut to the salivary glands.
Treatment
Drugs can only effect Plasmodium when it is outside of red blood cells and liver cells and in the blood, limiting their effectiveness.
Quinine was developed in the 17th century, but has lost effectiveness.
Artemisinin is a newer drug, but has documented resistance.
Normally, malaria is treated with artemisinin and a combination of other drugs, because it is unlikely that Plasmodium will have resistance to all the drugs.
Prevention
Mosquito behaviour is countered by:
Sleeping under mosquito nets, as they feed most often during dusk and dawn.
These nets are often treated with pyrethroid insecticide to kill any mosquitos.
Walls are treated with insecticide, as mosquitos often rest on walls after feeding.
Drain or cover stagnant water, to prevent mosquitoes from laying eggs.
Alternatively, a film of fish oil is applied to lower surface tension, preventing the larvae from piercing the surface to obtain oxygen.
Biological control:
Fish are introduced to the water, causing the larvae to be consumed.
Mosquitoes are infected with Wolbachia bacterium, which blocks Plasmodium development.
Male mosquitos are sterilised via X-rays, therefore no offspring are produced.
Virus pathogenicity and reproduction
Virus are sometimes described as the ‘ultimate parasite‘ as they are inert outside of living cells.
They show no life characteristics, except for when they are replicated within a host cell.
There are two cycles a pathogen can follow:
The lytic cycle, where a virus immediately reproduces using the host’s metabolism to copy their own nucleic acids (DNA or RNA) and synthesise a new protein coat.
This cycle occurs in 4 steps:
The virion attaches to a cell.
Viral nucleic acid is injected into the cell, leaving the protein coat outside.
The nucleic acid and capsid protein are synthesised using the host cell metabolism and they assemble to make mature virus particles.
Cell lysis then releases the viruses.
Some viruses are lysogenic, meaning they integrate their nucleic acid into the host cell genome, and can remain there for many cell generations with no clinical effect.
They will then enter the lytic cycle later when triggered, producing symptoms.
Viruses can be pathogenic in many ways:
Cell lysis - In bacteria, the pressure of new bacteriophage particles inside the cell causes it to burst.
In animal cells, inflammation cause by T-lymphocytes or antibodies causes lysis.
An example is rhinovirus, a type of common cold, which lyses cells in the upper respiratory tract.
Toxins - Viral components and their by-products can be toxic. The mechanisms for this are not fully understood, but examples include:
Measles virus causing chromosome fusion.
Herpes virus causing cell fusion.
Viral proteins inhibiting
RNA, DNA and protein synthesis.
Cell transformation - Viral DNA can integrate into the host chromosome.
If the DNA inserts into a pro-oncogene or tumour suppressor gene it can cause rapid controlled mitosis, making it cancerous.
An example is HPV, where cervical cancer is caused by entering into the TP53 tumour suppressor gene.
Immune suppression - This can include:
Suppression of reactions that cause B and T lymphocytes to mature.
Reduction of antibody formation.
An example is HIV, which destroys a group of T helper cells, preventing B lymphocytes from making antibodies.
This makes those with HIV immuno-compromised and highly susceptible to infection.
Antibiotics
Types
Compounds that inhibit the growth of bacteria are known as antimicrobials. This includes:
Antiseptics used on living tissue, such as Dettol.
Disinfectants used on non-living surfaces, such as bleach.
Antibiotics.
Antibiotics are produced by fungi, and only act on bacteria, not viruses and eukaryotic cells.
They therefore treat without causing any harm to the patient.
There are two types of spectrums for bacteria:
Broad-spectrum - Affect many different Gram-positive and Gram-negative species, such as ampicillin and tetracycline.
Narrow-spectrum - More selective, such as only killing Gram-positive bacteria, like penicillin.
Antibiotics also affect different aspects of bacterial metabolism:
Bactericidal antibiotics kill bacteria, such as penicillin.
Bacteriostatic antibiotics prevent bacterial multiplication, but do not kill bacteria. Bacteria would return to normal when the antibiotic is not present.
Examples include sulphonamides, which are competitive enzyme inhibitors and tetracycline.
Bacterial cell walls
All bacteria have a peptidoglycan, or murein, cell wall, but this varies on size based on whether they are gram positive or negative.
It contains polysaccharide and short chains of amino acids.
Transpeptidase enzymes cross-link polysaccharide molecules by attaching them to side chains of amino acids.
This makes the cell wall strong, gives the cell it’s shape and allows it resist bursting via osmosis.
Gram-positive bacteria have a thick layer of murein, making up over 90% of their cell wall.
Pores in this layer close during the depolarization stage of the gram stain test, so the CV is retained within the cell.
Safranin then turns the violet colour to a purple.
Murein is accessible to molecules outside the cell, making it susceptible to lysozymes and penicillin.
Gram-negative bacteria have a thin layer or murein, no more than 10% of the cell wall. This is surrounded by lipoprotein and lipopolysaccharide.
These lipid molecules are disrupted by the decolorization stage of the Gram staining, causing CV to leak out the cell and leaving them unstained.
Safarin then turns these cells red.
This layer protects the murein from antimicrobial agents, such as lysozymes and penicillin.
Antibiotic mechanisms
Penicillin
This is released by the penicillium fungus when its growth is inhibited and it is under high stress.
This is bactericidal, as it bursts cells by breaking their cell walls.
Originally, it was mass produced from P. notatum, but now high yielding strains of P. chrysogenum are used.
It is grown aerobically in industrial fermenters and penicillin is then purified for use.
Penicillin is unique from other antibiotics as it is small enough to penetrate right through mureine, so the whole thickness of the cell wall is affected.
The first penicillin was penicillin G, which had to be injected as stomach acid broke it down.
Penicillin V and other derivatives, such as ampicillin, can be taken orally.
Penicillin works in 5 steps:
It readily diffuses through the cell wall of Gram-positive bacteria and it enters some Gram-negative bacteria through surface molecules called porins.
This makes it a narrow spectrum antibiotic.
Bacteria continues to break down and remake it’s cell wall.
Penicillin prevents this via acting as an enzyme inhibitor the the DD-transpeptidase enzyme, which makes cross-links between amino acid side chains joining peptidoglycan molecules.
This enzyme is also known as the penicillin binding protein.
The cell wall continues to break down via hydrolysis, meaning more is lost than gained.
Precursors for the cell wall creation also build up and are hydrolysed, as they are not being used in cell wall production.
The cell wall then becomes so weakened, that water entering the cell via osmosis causes too much pressure for the cell wall, which lyses.
Tetracycline
Produced by the Streptomyces fungus, and is a broad spectrum antibiotic.
It is also bacteriostatic as it inhibits protein synthesis.
It has a wide medical use, and is used for acne, common infections (such as Chlamydia), anthrax and plague.
It has even been shown to have activity against eukaryotic parasites, such as Plasmodium.
However, many bacteria are beginning to shown resistance against Tetracycline.
It works in 3 steps:
It diffuses and is pumped into bacteria cells.
It then binds to small (30S) ribosome subunit and blocks tRNA attachment in the second position, the A site, so no new amino acids can be added to a polypeptide chain.
This is reversible, meaning it has a bacteriostatic effect.
Antibiotic overuse
Antibiotics have been used throughout history, especially during wars.
Now, however, antibiotics are being used as a preventive measure for infection, meaning they are used continuously and not in response to infection.
This is because productivity is increased when an animal has more energy for growth over fighting infection.
However, some bacteria will develop a resistance to antibiotics, giving them a selective advantage over un-immune bacteria.
They will then reproduce and pass on the immunity allele, building a resistant population.
There are two sources of these antibiotic resistant alleles:
Every time bacterial DNA replicates, mutations conferring resistance may arise.
Bacteria replicate rapidly in suitable conditions, increasing their rate of mutation.
Bacteria can acquire plasmids with antibiotic resistant alleles from their environment.
These then replicate inside a bacterium, and are passed onto daughter cells when the bacteria replicates.
Examples of resistance against penicillin include:
Secreting B-lactamase, which is an enzyme which degrades penicillin.
Altered DD-transpeptidase enzyme, which prevents penicillin from binding.
Penicillin entry is reduced via fewer or smaller porins.
Examples of resistance against tetracycline include:
Tetracycline is pumped out of cells.
Tetracycline is dislodged from it’s binding.
Tetracycline is prevented from ever attaching to a ribosome.
Without antibiotics, antibiotic resistant bacteria have a selective disadvantage due to energy required to synthesise these proteins. This would make it more likely to die.
Therefore, the continuous use of antibiotics gives these bacteria this advantage, increasing their population.
Several bacteria have begun to show resistance, such as leprosy, TB and gonorrhea.
Some have even shown resistance to multiple bacteria, such as:
MRSA - Methicillin-resistant Staphylococcus aureus.
This is resistant to penicillin and all it’s derivatives, and it treated with vancomycin.
Clostridium difficile - Severe cases are also treated with vancomycin.
New antibiotics need to be developed in order to combat infection post-surgery, otherwise bacteria will become life threatening again.
Immune response
The immune system exists to resist disease.
There are physical barriers to protect against the entry of pathogens.
if these fail, there are cellular and chemical responses.
Every day, huge numbers of microorganisms invade the body, most of the time individuals remain healthy.
It does this by detecting foreign ‘non-self’ antigens and distinguishing them from ‘self‘ antigens.
Innate immune system
These are natural barriers that resist infection:
The skin covers the external surface of the body, except as openings such as the mouth and eyes.
Keratin in epidermal cells makes skin waterproof.
Collagen in the connective tissue of the dermis, maintained by vitamin C, makes the skin tough.
The skin flora, or microbiota, comprises bacteria and fungi which outcompete pathogenic strains.
Unlike pathogens, these are hard to wash off and so regular washing is a good technique to remove pathogens.
Inhaled air is a source of microorganisms and their spores.
The mucus traps them and cilia of epithelial cells lining the respiratory passages brings them up to the opening of the oesophagus, where they are swallowed.
When the skin barrier is breached:
If capillaries are broken, blood clots prevent the entry of microbes.
Inflammation sets in, where increased blood flow towards the site of infection brings in large numbers of phagocytic cells .
The broken capillaries heal and the raised temperature is unfavourable to microbes.
Adaptive immune system
‘Adaptive‘ means the body produces a specific response to each antigen, so the body is adapting.
Lymphocytes provide this response, and are derived from stem cells in the bone marrow, and their precise role depends on their subsequent location.
Adaptive response
This has two components.
Humoral response
This results in the production of antibodies.
B lymphocytes mature in the spleen and lymph nodes.
Receptors on their cell membranes respond to a foreign protein in the bloodstream, and they divide making:
Plasma cells, which release antibodies.
Memory cells, which remain dormant in the circulation, and when the same antigen is encountered divide to form more B lymphocytes.

Antibodies are Y shaped glycoprotein molecules, known as immunoglobulins.
They have a quaternary structure, as each molecule is made up of four polypeptides held together by disulphide bonds.
The variable portions are specific to each antigen, and are at the end of the molecule.
The inner Y is heavy, while the outer parts are light
An antigen molecule binds to an antibody and each antibody molecule can bind to two antigen molecules.
Molecules with antigens on their surfaces are clumped together - they agglutinate (firmly stick together to form a mass).
Cell mediated response
This is the activation of phagocytic cells, B lymphocytes and T lymphocytes.
T lymphocytes activate in the thymus gland.
Receptors on their cell membranes respond to antigens and they divide, making:
T memory cells, which remain dormant in the circulation, and when the same antigen is encountered divide to form more T lymphocytes.
T killer or cytotoxic T cells, which kill pathogens with the antigen by lysing them.
T helper cells, which release chemicals including cytokines.
These cytokines stimulate:
Phagocytic cells, including macrophages, monocytes and neutrophils, which engulf pathogens and digest them.
B and T lymphocytes to undergo clonal expansion, which is when they divide repeatedly into genetically identical cells, forming a large population of cells specific to one antigen.
These cells differentiate into the various classes of lymphocyte.
B lymphocytes to make antibodies.
Fighting infection
Primary immune response
After first exposure to an antigen, there is a short latency period in which macrophages engulf the foreign antigen, or the cell, or virus to which it is attached.
They incorporate the antigenic molecules into their own cell membrane, a process known as antigen presentation, making macrophages a type of antigen-presenting cell.
T helper cells then detect these antigens and respond by secreting cytokines.
The B plasma cells secrete antibodies for around 3 weeks, subsiding symptoms of infection.
Secondary immune response
This relies on memory cells, and may protect against an identical antigen, even many decades after first exposure.
Upon re-exposure to even a small amount of an antigen, after a short latency period, memory cells undergo clonal expansion.
This is faster than the primary response.
Antibodies are made quicker, and are up to a 100x more concentrated than in the primary response.
They remain at high concentrations in the circulation for longer, and therefore no symptoms develop.
Active and passive immunity
Active immunity
This is when the body makes its own antibodies, stimulated by either infection or vaccination.
This is long lasting as the response produces memory cells.
Vaccination
Vaccination triggers humoral and cell-mediated responses, even though no harmful pathogen is present.
Types of vaccines include:
Antigens isolated from the pathogen, such as the HPV vaccine.
Weakened or attenuated (reduced in force, effect or value) strains of the pathogen, such as the MMR combined vaccine.
Inactive or killed pathogen, such as the whooping cough vaccine.
Inactivated toxin, such as the tetanus vaccine.
The vaccine is recognised as ‘non-self‘ by the body, and the immune system behaves as if it is a normal pathogen, meaning it produces it’s own antigens.
Over time, however, memory cells decrease if the body is not exposed to the antigen again.
In some cases, one or more boosters are given, such as the tetanus booster every 10 years.
This is further exposure to the vaccine and the response is faster, bigger and longer lasting than the first.
More memory cells are then made, meaning the body is protected for longer.
Passive immunity
This is when the body receives antibodies from another individual.
This can occur naturally, such as:
From the mother to the foetus across the placenta.
To the baby in breast milk.
Antibody injections, also known as Ig (immunoglobulin) replacement therapy are given in various situations, such as:
When rapid resistance is needed, and there is no time for active immune response to develop.
Example is when someone is bitten by a rabies infected animal, a wound which has a high risk of tetanus, or an urgent visit to a part of the world where an infection is endemic.
Cases of PIDD (primary immune deficiency disease) and cases of acquired immunity conditions, such as HIV, where patients do not make enough antibodies and cannot protect themselves against pathogens.
The protection given by injected antibodies is short lived because the body mounts an immune response against them as they are recognised as foreign.
Vaccine effectiveness
Vaccines can vary in effectiveness, and will have different schedules to provide long lasting immunity.
The HPV vaccine can come in only one dose, while the meningitis B is required 3 times and influenza vaccines are given annually to older people.
For a vaccination to be successful, it must:
Have a highly immunogenic (able to produce an immune response) antigen, meaning a single dose of the vaccine would cause a strong response from the immune system.
This would mean a large number of specific antibodies would be rapidly made, such as the smallpox vaccine using cowpox.
There should only be one antigenic type (serotype) of the pathogen, such as Rubella, where all Rubella viruses have the same surface antigens, meaning only one vaccine is required and antibodies formed can attack all of them.
The flu virus has many serotypes due to genetic recombination and frequent mutation, meaning memory cells produced from first exposure may not be stimulated.
Different vaccines are therefore needed for each antigenic type, and small changes in the antigens generated by mutation may mean that a vaccine may not be totally effective.
Ethical considerations
Vaccines are highly successful, and no other method is as effective.
For some diseases, it can be the only reliable means of protection.
Additionally, the more vaccinated, the less live pathogens in the population, meaning that fewer people will become infected in the future.
This controls the spread of disease, so even those non-vaccinated have some protection.
This is known as community or herd immunity and requires a particular proportion of people to be vaccinated.
If the proportion drops below this significant value, infection can spread.
This can be seen as a moral argument to get vaccinated.
But not everyone is vaccinated, for many reasons:
Vaccinations may not be medically advised for those:
Immunocompromised, for example they have a faulty spleen.
Taking chemotherapy.
Living with HIV-AIDS.
Very old.
Very ill in hospital.
Alternatively, some people choose not to vaccinate themselves or their children for other reasons, such as:
Religious objections.
A preference for natural and alternative medicine.
Mistrust of pharmaceutical companies who manufacture the vaccines.
Safety fears.
Cost effectiveness
Health authorities must consider whether the cost of vaccinations schemes outweighs the benefit.
For dangerous conditions, such as measles, vaccination is advised for all, but for influenza it is only recommended for target groups.
Overall, however, vaccination is considered cost effective due to the costs of treatment.
Compulsory vs voluntary vaccinations
The policy in the UK is that the government cannot infringe on the right of the individual to choose their own medication, therefore vaccination is not compulsory.
This becomes complicated in terms of health workers and children:
Health workers have a duty to not harm, which may be contravened if they are not vaccinated.
Children have decisions made by their parents, meaning they could be harmed by their parent’s poor decisions.
Places where vaccines are compulsory argue it is for the right of a society to protect itself, and prevent harm to others caused by anti vax individuals.
Side effects
This is sometimes used as a reason to not vaccinate children.
Common ones for vaccines include; soreness at injection site, fever, fatigue and muscle or joint pain.
Serious side effects have been documented but are extremely rare, but attention from mass media (availability heuristic) makes them seem more common.
 Knowt
Knowt
