
2.3a: Adaptations for transport in animals
Transport systems
In animals, these have the following features:
A suitable medium to carry materials, such as blood.
A pump, for example the heart, which keeps this medium flowing.
Valves to maintain the flow in one direction in order to resist gravity.
Some systems have:
Respiratory pigments in vertebrates and some invertebrates, but not insects. These increase the volume of oxygen which can be transported
A system of vessels with branching networks to distribute the transport medium to all parts of the body, such as the capillaries.
Different types in animals
Open circulatory systems
The blood doesn’t use vessels to move, and instead bathes in the tissues directly while held in a cavity called the haemocoel.
Insects use this system:
They have an open, dorsal tube-shaped heart which runs the length of the body. It pumps blood at a low pressure to the haemocoel, where materials are exchanged between the blood and body cells.
The blood returns slowly to the heart and open circulation starts again.
Oxygen is diffused directly to the tissues from tracheoles, therefore the blood needs no respiratory pigment.
Closed circulatory systems
This is when the blood runs in blood vessels, and there are two types:
Single circulation
The blood moves around the heart once in it’s passage around the body.
In fish, the ventricle of the heart pumps deoxygenated blood to the gills, where the capillary network decreases its pressure.
Oxygenated blood is carried to tissues, and returns to the atrium deoxygenated, where it is pumped again by the ventricle.
In earthworms, blood moves forward in the dorsal (top vessel), and back in the ventral (bottom) vessel.
Five pairs of pseudohearts (thickened, muscular blood vessels) pump the blood from the dorsal to the ventral vessel.
Double circulation
The blood moves around the heart twice in it’s passage around the body, used by mammals.
Blood is pumped through the heart at high pressure, which gives a rapid flow rate through blood vessels.
Blood pressure is reduced in lung capillaries, and this pressure would be too low to efficiently circulate to the rest of the body.
The blood is returned to the heart again to raise it’s pressure before being pumped around the body. This quickly delivers materials to body cells.
Organs never make direct contact with blood but are bathed by tissue fluid which seeps out of capillaries.
Haemoglobin is the pigment used to carry oxygen.
This is more efficient than a single circuit, as the blood is pumped around at a higher pressure.
Mammalian transport
There are two systems within the double circulatory system:
Pulmonary circulation - Part between the lungs and the heart.
Blood enters the heart through the right atrium, and exits towards the lungs from the right ventricle.
Once oxygenated, it exits from the other side of the lungs and enters the left atrium.
Systematic circulation - Part between the heart and the rest of the body tissues.
Oxygenated blood exits from the left ventricle, and is pumped by the heart to quickly move around the tissues.
It then returns to the heart through the right atrium, once deoxygenated.
In both circuits the blood enters the heart twice, once on the left and once on the right.
Blood vessels structure and function
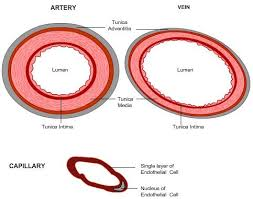
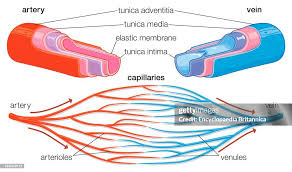
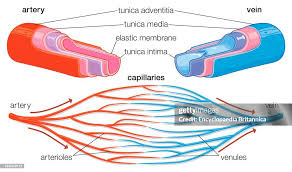
There are three types of vessels; arteries, veins and capillaries.
Function
Arteries:
Carry blood away from the heart, to bodily tissues and to the lungs to be oxygenated.
They have thick muscular walls to withstand the high blood pressure.
They branch into smaller vessels, arterioles, which further branch into capillaries.
Have semi-lunar valves present at the base of the aorta and pulmonary artery.
Capillaries:
A vast network that penetrate all tissues and organs of the body.
Blood from capillaries is collected in venules, which take blood into veins.
Veins:
Return blood to the heart from the venules and from the lungs.
If a vein is above the heart, it returns using gravity.
Otherwise, veins have semi-lunar valves along their length to ensure the flow remains in one direction, against gravity.
These work by timing for the pump of the heart; shutting until the heart pumps to stop blood being pooled to the feet.
When it pumps, these open, allowing the blood to move upwards.
Their faulty functioning leads to heart failure.
Blood pressure changes throughout this process:
Arteries - 160 mmHg - 120 mmHg.
Arterioles - 33 mmHg.
Capillaries - 30 mmHg - 15mmHg.
Venules - 15 mmHg.
Veins - 10 mmHg.
Structure
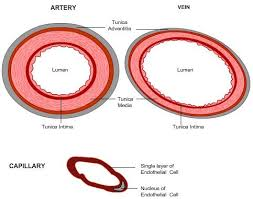
Arteries and veins share the same structural properties, with different proportions.
From the inside to the outside:
Lumen - Where the blood flows.
Wider in the veins, causing a decrease in blood pressure.
Endothelium - Lining of the vessel, one cell thick. Smooth to avoid friction.
Tunica intima - Comprises the endothelium, and also has elastic fibres in it’s collagen, which can stretch and recoil.
Tunica media - Contains elastic fibres and smooth muscle, and is thicker in arteries than veins, to maintain high blood pressure.
The elastic fibres stretch to accommodate for changes in blood flow and pressure caused by the heart pumping too fast or slow.
The stretched elastic fibres recoil at a certain point, which pushes blood on through the artery, which is felt as the pulse.
The smooth muscle also contracts to regulate blood flow and maintain blood pressure as the blood moves further from the heart.
These two structural features combine to maintain blood pressure as it changes throughout activity levels.
Tunica externa - Contains collagen fibres, which resist overstretching of the blood vessel.
This prevents blood vessels bursting, and can withstand extremely high pressure.
Capillaries have some similar structures:
They have thin walls, which are made of one layer of endothelium on a basement membrane.
There are pores between the cells, making the capillary walls permeable to water and solutes, such as glucose, allowing for the exchange of materials between the blood and the tissues.
They have a small diameter and slow blood pressure.
In one capillary bed there are many capillaries, which reduces rate of blood flow to allow time for the exchange of materials with the surrounding tissue fluid.
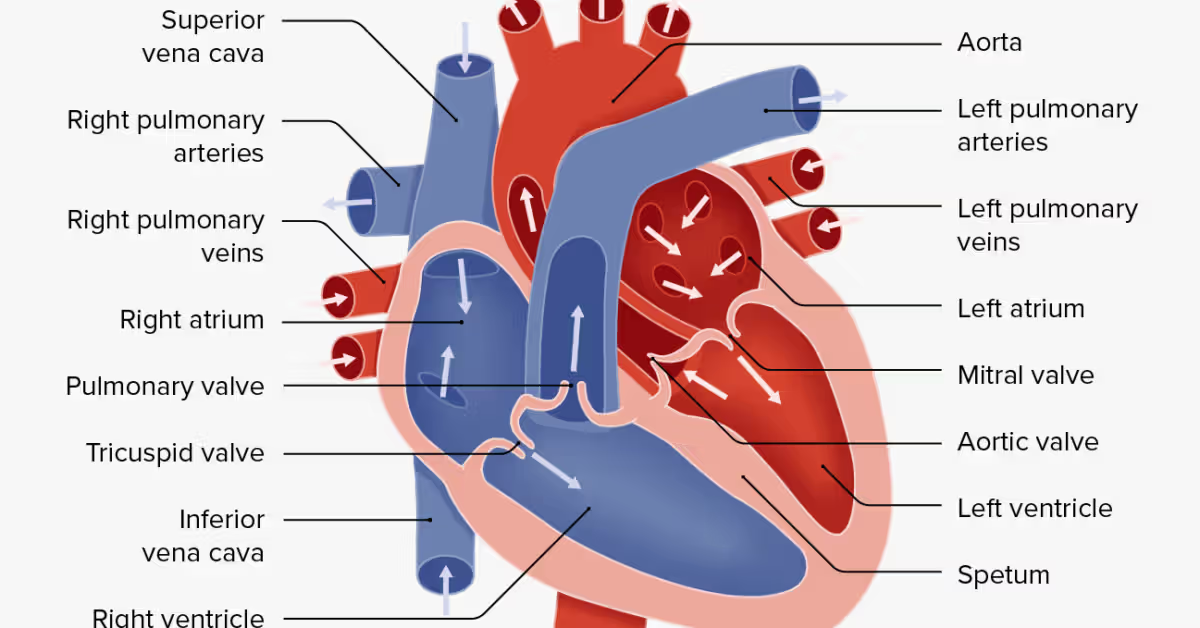
Heart
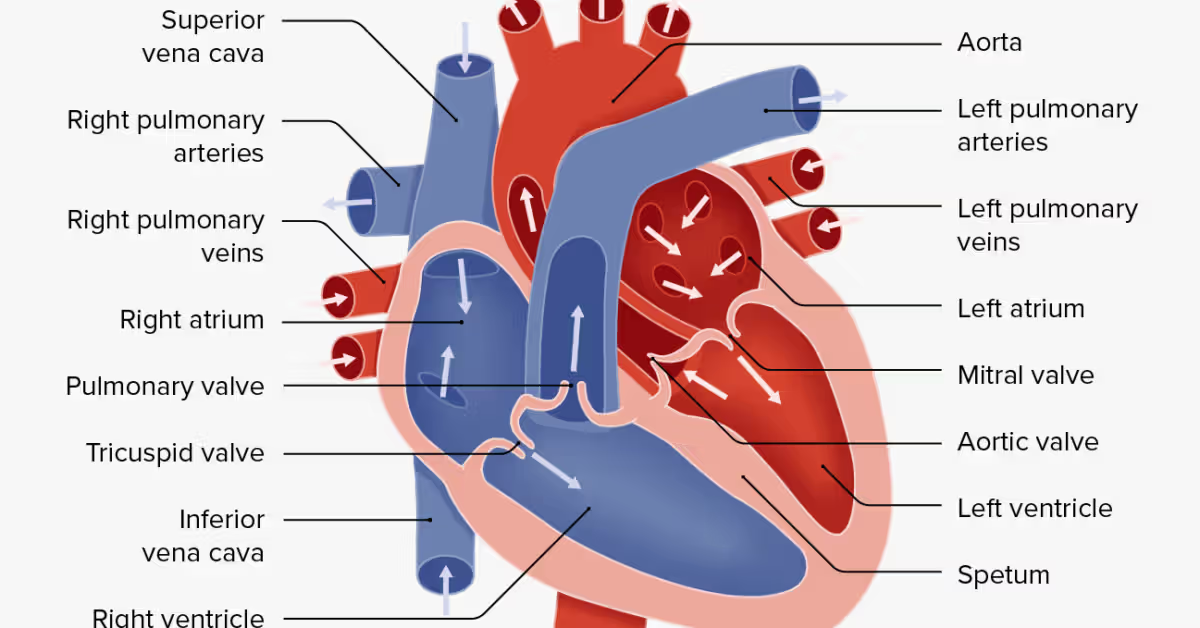
The heart is split into two sections, one that deals with oxygenated blood and one with deoxygenated blood.
These both have an atrium, which is where blood enters and have thin walls. These are above ventricles but below the pulmonary artery/ aorta.
They also both have a ventricle, which is where blood is pumped out from and have thicker walls. These are at the bottom of the heart. The left is thicker than the right.
On the right side, deoxygenated blood enters from the body via the inferior and superior vena cavae, which are named based on their positions, one above and one below the right side of the heart.
This leads to the right atrium, then to the right ventricle, then through the pulmonary artery to the lungs.
On the left side, oxygenated blood enters from the lungs via pulmonary veins which are on either side on the heart.
This then moves through the left atrium, to the left ventricle, and then through the aorta to the rest of the body.
The right side is slower than the left side, as it has thinner walls and is not being pumped out to the rest of the body.
There are also many valves:
Semi-lunar valves close to prevent blood falling back into the ventricle from the aorta and pulmonary artery.
The tricuspid valve prevents blood from the right atrium entering the right ventricle, and the bicuspid valve prevents blood from the left atrium entering the left ventricle.
Collectively, these two valves are known as the atrio-ventricular valves.
The heart is mainly made up of cardiac muscle, which is specialised for myogenic contraction, meaning it contracts and relaxes rhythmically and without need for outside intervention.
However, hormones and the nervous system can alter it’s pumping.
This muscle never tires.
Cardiac cycle
This describes the sequence of events that occur during a singular heartbeat, which on average lasts around 0.8 seconds. There is contractions, known as systole and relaxations, known as diastole. There are four stages:
Atrial systole
Lasts 0.1 seconds, and occurs right at the start of the cycle.
The atrium walls contract, increasing atrium blood pressure. This pushes the blood into the ventricles, through the tricuspid or bicuspid valves.
The blood then enters the ventricle, which is relaxed.
Atrial diastole
Starts at 0.2 seconds, and lasts until 0.8/the end of the cycle.
Once the atrium relaxes, blood begins to enter again through the pulmonary vein and vena cavae, readying for the cycle to start again.
Ventricular systole
Starts at 0.2 seconds, and lasts until 0.4.
The increased pressure in the ventricle causes the bicuspid/tricuspid valves to close to prevent back flow into the atria.
Ventricle walls contract and open the semi-lunar valves once they exceed pressure in the arteries.
This pushes the blood into either the pulmonary artery or aorta.
Ventricular diastole
Starts at 0.4 seconds, and lasts until 0.8 seconds/ the end of the cycle.
Ventricles relax, increasing volume and therefore pressure in them.
The semi-lunar valves shut, to prevent backflow into the ventricles.
The bicuspid and tricuspid valves also open.
Heartbeat control
The beat of the heart is controlled via electrical impulses generated by the sino-atrial node (SAN) - a group of specialised cardiac cells located in the wall of the right atrium. This acts as a pacemaker.
This impulse spreads over both atria, so they contract simultaneously.
However, the ventricles are electrically insulated via a thin layer of connective tissue except at another specialised group of cardiac cells known as the atrio-ventricular node (AVN).
This allows for a delay between atria and ventricles contracting, so ventricles only contract once the atria are finished contracting.
The AVN then passes this electrical impulse down to the nerves in the His bundle, which then moves down the left and right bundle branches and then to the apex of the heart, which is located at the very bottom in between the right and left sides (the point.)
This is then transported to Purkinje fibres in the ventricle walls, which carry it upwards through the ventricular wall muscles.
This causes the ventricles to contract simultaneously, from the apex upwards.
Electrocardiogram
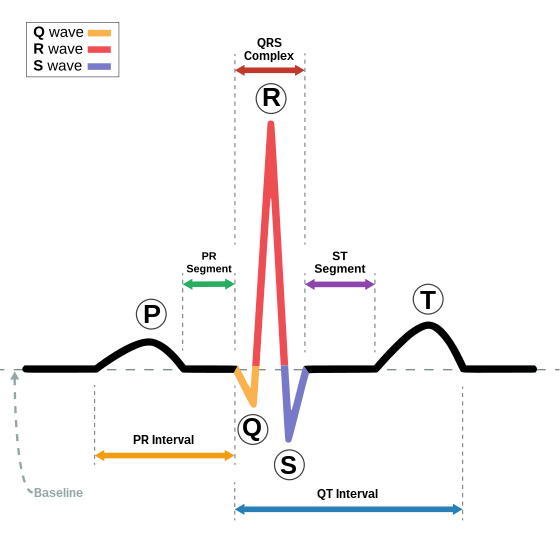
This is a trace of the voltage changes, detected by placing electrodes on the skin. It detects in many stages:
P wave is the voltage generated by the SAN/ atria contraction.
The PR interval is the time for the voltage from the SAN to reach the ventricles via the AVN.
The QRS complex shows the contraction of the ventricles.
The T wave is the repolarisation (reducing the polarisation caused by electrical spread across the membrane) of the ventricle.
The line between the T wave and the P wave of the next sample is the baseline of the trace, known as the isoelectric line.
It is S shaped, also known as sigmoidal. This allows for rapid unloading at small oxygen partial pressure changes.
This can show many different conditions:
Those with atrial fibrillation will have a rapid heartbeat and may lack a P wave.
Those who’ve had heart attacks may have a wide QRS complex.
Those with enlarged ventricle walls may have a QRS complex with a greater voltage charge.
Changes in the ST segment/T wave may be related to insufficient blood being delivered to the heart muscle, such as in atherosclerosis and blocked coronary arteries.
Issues associated
Cardiac ischaemia is a disease that causes decreased blood flow and oxygen to enter the heart. It is caused by decreased lumen area, which is caused by LDL fatty deposits.
Treatment has lead to a decrease in deaths due to this.
There are five steps to treatment:
Identification and treatment of co-morbidities.
Reduction of risk factors.
Modification of lifestyle, such as changing diet or quitting smoking.
Drug treatment of angina (heart pain).
Surgery, such as coronary artery bypass grafting where surgeons cut at the blockage, and reattach the artery to one that is non-damaged, or stent placement.
Blood
Composition
This is made up of 45% cells and 55% solution, which is known as plasma. It contains four main sections:
Red blood cells (erythrocytes) contain the red pigment haemoglobin, which is used to transport oxygen.
They are biconcave discs, which have a larger SA and smaller diffusion pathway than normal discs for increased oxygen diffusion.
They have no nucleus to make room for more haemoglobin.
Plasma is pale yellow and 90% water.
It contains food molecules (such as glucose and amino acids), waste products (such as urea), hormones and the rest of the blood cells.
It also distributes heat.
Platelets which form blood clots to prevent bleeding.
White blood cells fight bacteria and foreign substances.
Haemoglobin
Makes up around 95% of the red blood cell mass, and is the means to transport oxygen around the body.
It is made of four polypeptide chains which bind to one haem group, which contain one iron ion, making it a quaternary structure protein. It has two beta chains, and two alpha chains.
Each haem group can combine with one oxygen molecule, so four can join altogether.
This forms oxyhaemoglobin.
It binds to oxygen by changing it’s affinity for oxygen via changing its shape, a process known as cooperative binding.
This first oxygen bonded changes the shape of the haemoglobin to make it easier for the second to bond.
The second does the same for the third.
The third does not change the shape, meaning a large increase in oxygen concentration (oxygen partial pressure) for the fourth molecule to bind.
Haemoglobin readily associates with oxygen at the alveoli, and readily dissociates at the respiring tissues.
It can also change its affinity based on environmental factors:
It reaches a high affinity in low oxygen conditions, such as high altitudes. This means it attaches to an increased amount of oxygen, but releases a decreased amount.
It reaches a low affinity in high oxygen conditions. This means it attaches to an decreased amount of oxygen, but releases an increased amount.
Myoglobin
This is a protein similar to haemoglobin in that it attaches to oxygen, however it can only bind to a singular molecule and binds tighter, acting as oxygen storage.
It is present in muscles.
It only has one haem group, and is a globular tertiary structure protein.
Dissociation curve
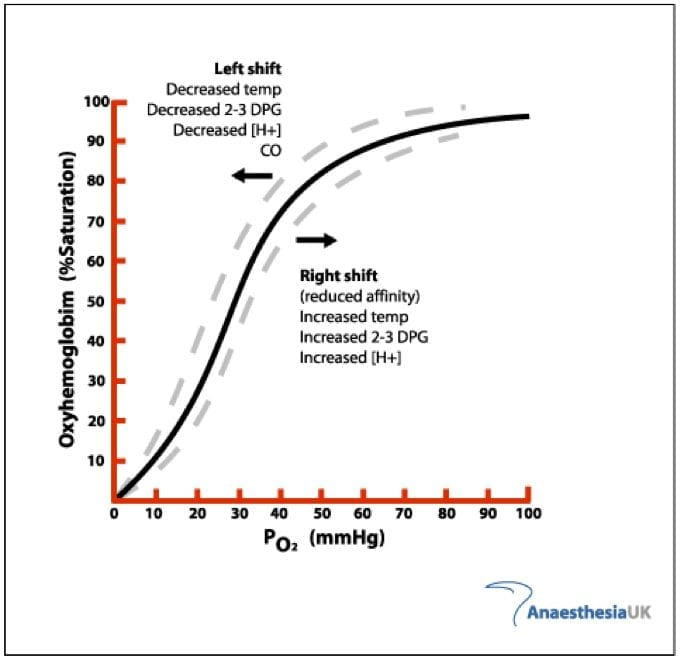
A dissociation curve shows how effective haemoglobin bonds to oxygen in different conditions:
The x axis is the partial pressure of oxygen, which measures the oxygen concentration in the current environment. This is measured in kilopascals (kPa).
The y axis is the percentage saturation, which measures how much oxygen is typically bonded onto haemoglobin. This is measured in percentages.
This tells us that the higher the partial pressure of oxygen, the higher percentage saturation of haemoglobin.
At around 25 kPa and below, the haemoglobin is in exercising tissues, which have a high oxygen requirement and therefore take more from haemoglobin.
At around 25 kPa and above, the haemoglobin is in resting tissues, which still need oxygen but not in as high demand.
At around 60 kPa and above, haemoglobin is in the alveoli, an oxygen rich environment where it bonds with oxygen.
This graph can also represent high and low affinity:
A left shift represents high affinity, with more oxygen intake and less outtake.
A right shift represents low affinity, with more oxygen outtake and less intake.
Many factors additional factors affect this graph:
The Bohr effect means that in areas of high carbon dioxide concentration the curve shifts to the right, meaning it gives away oxygen more easily.
This means it can unload oxygen easier in capillaries and load more easily in alveoli.
Fetal haemoglobin has a higher affinity, so it will curve to the left. It does this by differing in two of the four polypeptide chains.
This is due to the fact it gets its oxygen from the mother’s blood, and therefore requires a fast intake to survive.
Different organisms have different oxygen conditions, therefore their graphs are different, for example:
Lugworms bury themselves in sand during high tides, an extremely low oxygen environment. They also have a low metabolic rate. Therefore, their curve is to the left of humans, and has a high affinity.
Llamas live on mountainous regions, so they need a higher affinity to take in the oxygen necessary for survival. This is to the left of humans but to the right of lugworms.
Carbon dioxide transport
Carbon dioxide travels in many forms:
5% as a solution in the plasma.
10% bound to haemoglobin as carbamino-haemoglobin.
85% as HCO3-, a hydrogen carbonate ion.
It is mostly converted to this ion inside the red blood cell, and then diffused out to plasma. This happens in 6 steps:
Carbon dioxide in the blood diffuses into a red blood cell.
The enzyme carbonic anhydrase catalyses the combination of carbon dioxide and water, which creates carbonic acid/H2CO3.
Carbonic acid then dissociates to a hydrogen ion and a hydrogen carbonate ion (H+ and HCO3-).
The HCO3- ions diffuse out of the red blood cell into the plasma.
In order for the cell to maintain it’s electrochemical neutrality, chloride ions then diffuse into the cell.
This movement is known as a chloride shift.
The H+ ions dissociate oxyhaemoglobin into oxygen and haemoglobin, as the H+ combines with haemoglobin to make haemoglobinic acid (HHb).
The H+ ions are removed, so the pH of the red blood cell doesn’t fall.
Oxygen then leaves the red blood cell via diffusion, where it enters the tissue fluid and then the cells.
This means that more HCO3- ions = more H+ ions, therefore explaining the Bohr effect as more carbon dioxide in red blood cells the more oxygen is released from haemoglobin.
Therefore, carbon dioxide is necessary to deliver oxygen to respiring tissues.
Tissue fluid
Blood cannot directly touch tissues, as blood vessels are closed systems. Therefore, tissue fluid is allows for the exchange of materials.
Capillaries have many features to support this diffusion:
Permeable.
Thin, for short diffusion pathway.
Large SA.
Lower blood pressure to give time for substance exchange.
Tissue fluid is extremely similar to plasma, except is does not contain the colloidal plasma proteins that lower the solute potential of plasma.
The exchanges occur through the use of hydrostatic pressure (the pressure of the blood pressing against the capillary wall) and the osmotic pressure (generated by the low solute potential in the plasma).
The exchange happens in two stages:
Ultra-filtration - Named as it filters out micromolecules, therefore the colloidal plasma proteins cannot leave as they are too big.
This is at the arterioles, therefore there is a high blood pressure, causing a high hydrostatic pressure which pushes tissue fluid out containing molecules cells need such as oxygen, glucose, amino acids, fatty acids, hormones and salts.
There is also an osmotic pressure, but the hydrostatic pressure is higher than this, causing molecules to keep leaving the blood.
Respiring tissues also have a lower concentration of these molecules, aiding the hydrostatic pressure in allowing these molecules out.
Absorption - Named as it absorbs waste products from the cells.
The volume of the blood is lowered via ultra-filtration and the friction of the capillary walls against the blood. This reduces blood pressure, and therefore hydrostatic pressure.
Less fluid means the colloidal plasma proteins are more concentrated, increasing osmotic pressure. This means osmotic pressure is stronger than hydrostatic pressure, pulling water back in.
The tissue fluid surrounding the cells picks up their waste products, such as carbon dioxide and urea, which is diffused into blood down a concentration gradient.
However, not all the tissue fluid returns to the blood. Around 10% drains into the blindly ending (dead end) lymph capillaries of the lymphatic system.
This mostly returns to the venous system via the thoracic duct, which empties into the subclavian vein above the heart.
There are two issues associated with this process:
Hypertension - Too high blood pressure.
The blood does not have enough time for absorption of waste materials.
This causes an accumulation of waste products and carbon dioxide, far beyond what the lymph capillaries can account for.
This causes oedema - a build up of this fluid which causes feet to swell.
Hypotension - Too low blood pressure.
Not enough ultra-filtration occurs, so nutrients are not received by cells.
This causes starvation of the cells, and increases the volume of blood, which can cause bloating.
2.3a: Adaptations for transport in animals
Transport systems
In animals, these have the following features:
A suitable medium to carry materials, such as blood.
A pump, for example the heart, which keeps this medium flowing.
Valves to maintain the flow in one direction in order to resist gravity.
Some systems have:
Respiratory pigments in vertebrates and some invertebrates, but not insects. These increase the volume of oxygen which can be transported
A system of vessels with branching networks to distribute the transport medium to all parts of the body, such as the capillaries.
Different types in animals
Open circulatory systems
The blood doesn’t use vessels to move, and instead bathes in the tissues directly while held in a cavity called the haemocoel.
Insects use this system:
They have an open, dorsal tube-shaped heart which runs the length of the body. It pumps blood at a low pressure to the haemocoel, where materials are exchanged between the blood and body cells.
The blood returns slowly to the heart and open circulation starts again.
Oxygen is diffused directly to the tissues from tracheoles, therefore the blood needs no respiratory pigment.
Closed circulatory systems
This is when the blood runs in blood vessels, and there are two types:
Single circulation
The blood moves around the heart once in it’s passage around the body.
In fish, the ventricle of the heart pumps deoxygenated blood to the gills, where the capillary network decreases its pressure.
Oxygenated blood is carried to tissues, and returns to the atrium deoxygenated, where it is pumped again by the ventricle.
In earthworms, blood moves forward in the dorsal (top vessel), and back in the ventral (bottom) vessel.
Five pairs of pseudohearts (thickened, muscular blood vessels) pump the blood from the dorsal to the ventral vessel.
Double circulation
The blood moves around the heart twice in it’s passage around the body, used by mammals.
Blood is pumped through the heart at high pressure, which gives a rapid flow rate through blood vessels.
Blood pressure is reduced in lung capillaries, and this pressure would be too low to efficiently circulate to the rest of the body.
The blood is returned to the heart again to raise it’s pressure before being pumped around the body. This quickly delivers materials to body cells.
Organs never make direct contact with blood but are bathed by tissue fluid which seeps out of capillaries.
Haemoglobin is the pigment used to carry oxygen.
This is more efficient than a single circuit, as the blood is pumped around at a higher pressure.
Mammalian transport
There are two systems within the double circulatory system:
Pulmonary circulation - Part between the lungs and the heart.
Blood enters the heart through the right atrium, and exits towards the lungs from the right ventricle.
Once oxygenated, it exits from the other side of the lungs and enters the left atrium.
Systematic circulation - Part between the heart and the rest of the body tissues.
Oxygenated blood exits from the left ventricle, and is pumped by the heart to quickly move around the tissues.
It then returns to the heart through the right atrium, once deoxygenated.
In both circuits the blood enters the heart twice, once on the left and once on the right.
Blood vessels structure and function
There are three types of vessels; arteries, veins and capillaries.
Function
Arteries:
Carry blood away from the heart, to bodily tissues and to the lungs to be oxygenated.
They have thick muscular walls to withstand the high blood pressure.
They branch into smaller vessels, arterioles, which further branch into capillaries.
Have semi-lunar valves present at the base of the aorta and pulmonary artery.
Capillaries:
A vast network that penetrate all tissues and organs of the body.
Blood from capillaries is collected in venules, which take blood into veins.
Veins:
Return blood to the heart from the venules and from the lungs.
If a vein is above the heart, it returns using gravity.
Otherwise, veins have semi-lunar valves along their length to ensure the flow remains in one direction, against gravity.
These work by timing for the pump of the heart; shutting until the heart pumps to stop blood being pooled to the feet.
When it pumps, these open, allowing the blood to move upwards.
Their faulty functioning leads to heart failure.
Blood pressure changes throughout this process:
Arteries - 160 mmHg - 120 mmHg.
Arterioles - 33 mmHg.
Capillaries - 30 mmHg - 15mmHg.
Venules - 15 mmHg.
Veins - 10 mmHg.
Structure
Arteries and veins share the same structural properties, with different proportions.
From the inside to the outside:
Lumen - Where the blood flows.
Wider in the veins, causing a decrease in blood pressure.
Endothelium - Lining of the vessel, one cell thick. Smooth to avoid friction.
Tunica intima - Comprises the endothelium, and also has elastic fibres in it’s collagen, which can stretch and recoil.
Tunica media - Contains elastic fibres and smooth muscle, and is thicker in arteries than veins, to maintain high blood pressure.
The elastic fibres stretch to accommodate for changes in blood flow and pressure caused by the heart pumping too fast or slow.
The stretched elastic fibres recoil at a certain point, which pushes blood on through the artery, which is felt as the pulse.
The smooth muscle also contracts to regulate blood flow and maintain blood pressure as the blood moves further from the heart.
These two structural features combine to maintain blood pressure as it changes throughout activity levels.
Tunica externa - Contains collagen fibres, which resist overstretching of the blood vessel.
This prevents blood vessels bursting, and can withstand extremely high pressure.
Capillaries have some similar structures:
They have thin walls, which are made of one layer of endothelium on a basement membrane.
There are pores between the cells, making the capillary walls permeable to water and solutes, such as glucose, allowing for the exchange of materials between the blood and the tissues.
They have a small diameter and slow blood pressure.
In one capillary bed there are many capillaries, which reduces rate of blood flow to allow time for the exchange of materials with the surrounding tissue fluid.
Heart
The heart is split into two sections, one that deals with oxygenated blood and one with deoxygenated blood.
These both have an atrium, which is where blood enters and have thin walls. These are above ventricles but below the pulmonary artery/ aorta.
They also both have a ventricle, which is where blood is pumped out from and have thicker walls. These are at the bottom of the heart. The left is thicker than the right.
On the right side, deoxygenated blood enters from the body via the inferior and superior vena cavae, which are named based on their positions, one above and one below the right side of the heart.
This leads to the right atrium, then to the right ventricle, then through the pulmonary artery to the lungs.
On the left side, oxygenated blood enters from the lungs via pulmonary veins which are on either side on the heart.
This then moves through the left atrium, to the left ventricle, and then through the aorta to the rest of the body.
The right side is slower than the left side, as it has thinner walls and is not being pumped out to the rest of the body.
There are also many valves:
Semi-lunar valves close to prevent blood falling back into the ventricle from the aorta and pulmonary artery.
The tricuspid valve prevents blood from the right atrium entering the right ventricle, and the bicuspid valve prevents blood from the left atrium entering the left ventricle.
Collectively, these two valves are known as the atrio-ventricular valves.
The heart is mainly made up of cardiac muscle, which is specialised for myogenic contraction, meaning it contracts and relaxes rhythmically and without need for outside intervention.
However, hormones and the nervous system can alter it’s pumping.
This muscle never tires.
Cardiac cycle
This describes the sequence of events that occur during a singular heartbeat, which on average lasts around 0.8 seconds. There is contractions, known as systole and relaxations, known as diastole. There are four stages:
Atrial systole
Lasts 0.1 seconds, and occurs right at the start of the cycle.
The atrium walls contract, increasing atrium blood pressure. This pushes the blood into the ventricles, through the tricuspid or bicuspid valves.
The blood then enters the ventricle, which is relaxed.
Atrial diastole
Starts at 0.2 seconds, and lasts until 0.8/the end of the cycle.
Once the atrium relaxes, blood begins to enter again through the pulmonary vein and vena cavae, readying for the cycle to start again.
Ventricular systole
Starts at 0.2 seconds, and lasts until 0.4.
The increased pressure in the ventricle causes the bicuspid/tricuspid valves to close to prevent back flow into the atria.
Ventricle walls contract and open the semi-lunar valves once they exceed pressure in the arteries.
This pushes the blood into either the pulmonary artery or aorta.
Ventricular diastole
Starts at 0.4 seconds, and lasts until 0.8 seconds/ the end of the cycle.
Ventricles relax, increasing volume and therefore pressure in them.
The semi-lunar valves shut, to prevent backflow into the ventricles.
The bicuspid and tricuspid valves also open.
Heartbeat control
The beat of the heart is controlled via electrical impulses generated by the sino-atrial node (SAN) - a group of specialised cardiac cells located in the wall of the right atrium. This acts as a pacemaker.
This impulse spreads over both atria, so they contract simultaneously.
However, the ventricles are electrically insulated via a thin layer of connective tissue except at another specialised group of cardiac cells known as the atrio-ventricular node (AVN).
This allows for a delay between atria and ventricles contracting, so ventricles only contract once the atria are finished contracting.
The AVN then passes this electrical impulse down to the nerves in the His bundle, which then moves down the left and right bundle branches and then to the apex of the heart, which is located at the very bottom in between the right and left sides (the point.)
This is then transported to Purkinje fibres in the ventricle walls, which carry it upwards through the ventricular wall muscles.
This causes the ventricles to contract simultaneously, from the apex upwards.
Electrocardiogram
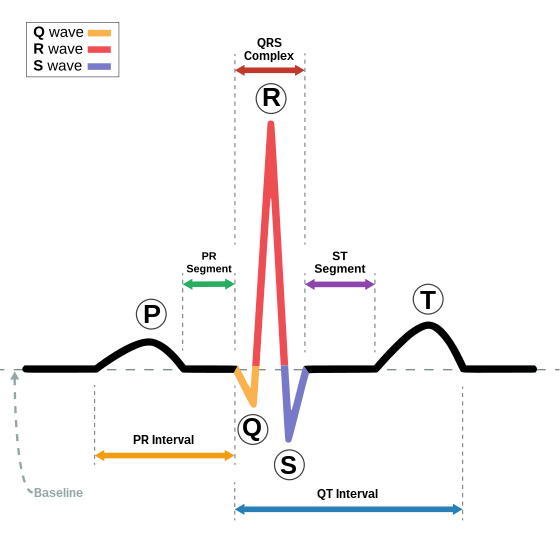
This is a trace of the voltage changes, detected by placing electrodes on the skin. It detects in many stages:
P wave is the voltage generated by the SAN/ atria contraction.
The PR interval is the time for the voltage from the SAN to reach the ventricles via the AVN.
The QRS complex shows the contraction of the ventricles.
The T wave is the repolarisation (reducing the polarisation caused by electrical spread across the membrane) of the ventricle.
The line between the T wave and the P wave of the next sample is the baseline of the trace, known as the isoelectric line.
It is S shaped, also known as sigmoidal. This allows for rapid unloading at small oxygen partial pressure changes.
This can show many different conditions:
Those with atrial fibrillation will have a rapid heartbeat and may lack a P wave.
Those who’ve had heart attacks may have a wide QRS complex.
Those with enlarged ventricle walls may have a QRS complex with a greater voltage charge.
Changes in the ST segment/T wave may be related to insufficient blood being delivered to the heart muscle, such as in atherosclerosis and blocked coronary arteries.
Issues associated
Cardiac ischaemia is a disease that causes decreased blood flow and oxygen to enter the heart. It is caused by decreased lumen area, which is caused by LDL fatty deposits.
Treatment has lead to a decrease in deaths due to this.
There are five steps to treatment:
Identification and treatment of co-morbidities.
Reduction of risk factors.
Modification of lifestyle, such as changing diet or quitting smoking.
Drug treatment of angina (heart pain).
Surgery, such as coronary artery bypass grafting where surgeons cut at the blockage, and reattach the artery to one that is non-damaged, or stent placement.
Blood
Composition
This is made up of 45% cells and 55% solution, which is known as plasma. It contains four main sections:
Red blood cells (erythrocytes) contain the red pigment haemoglobin, which is used to transport oxygen.
They are biconcave discs, which have a larger SA and smaller diffusion pathway than normal discs for increased oxygen diffusion.
They have no nucleus to make room for more haemoglobin.
Plasma is pale yellow and 90% water.
It contains food molecules (such as glucose and amino acids), waste products (such as urea), hormones and the rest of the blood cells.
It also distributes heat.
Platelets which form blood clots to prevent bleeding.
White blood cells fight bacteria and foreign substances.
Haemoglobin
Makes up around 95% of the red blood cell mass, and is the means to transport oxygen around the body.
It is made of four polypeptide chains which bind to one haem group, which contain one iron ion, making it a quaternary structure protein. It has two beta chains, and two alpha chains.
Each haem group can combine with one oxygen molecule, so four can join altogether.
This forms oxyhaemoglobin.
It binds to oxygen by changing it’s affinity for oxygen via changing its shape, a process known as cooperative binding.
This first oxygen bonded changes the shape of the haemoglobin to make it easier for the second to bond.
The second does the same for the third.
The third does not change the shape, meaning a large increase in oxygen concentration (oxygen partial pressure) for the fourth molecule to bind.
Haemoglobin readily associates with oxygen at the alveoli, and readily dissociates at the respiring tissues.
It can also change its affinity based on environmental factors:
It reaches a high affinity in low oxygen conditions, such as high altitudes. This means it attaches to an increased amount of oxygen, but releases a decreased amount.
It reaches a low affinity in high oxygen conditions. This means it attaches to an decreased amount of oxygen, but releases an increased amount.
Myoglobin
This is a protein similar to haemoglobin in that it attaches to oxygen, however it can only bind to a singular molecule and binds tighter, acting as oxygen storage.
It is present in muscles.
It only has one haem group, and is a globular tertiary structure protein.
Dissociation curve
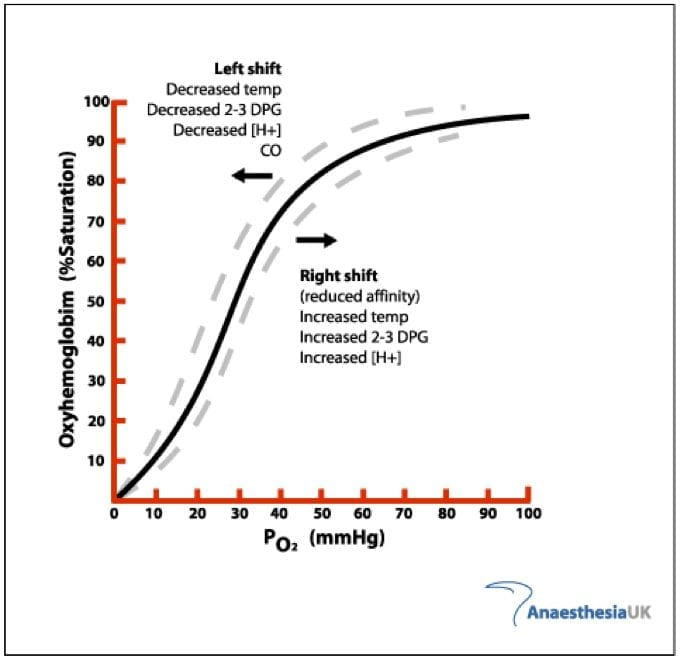
A dissociation curve shows how effective haemoglobin bonds to oxygen in different conditions:
The x axis is the partial pressure of oxygen, which measures the oxygen concentration in the current environment. This is measured in kilopascals (kPa).
The y axis is the percentage saturation, which measures how much oxygen is typically bonded onto haemoglobin. This is measured in percentages.
This tells us that the higher the partial pressure of oxygen, the higher percentage saturation of haemoglobin.
At around 25 kPa and below, the haemoglobin is in exercising tissues, which have a high oxygen requirement and therefore take more from haemoglobin.
At around 25 kPa and above, the haemoglobin is in resting tissues, which still need oxygen but not in as high demand.
At around 60 kPa and above, haemoglobin is in the alveoli, an oxygen rich environment where it bonds with oxygen.
This graph can also represent high and low affinity:
A left shift represents high affinity, with more oxygen intake and less outtake.
A right shift represents low affinity, with more oxygen outtake and less intake.
Many factors additional factors affect this graph:
The Bohr effect means that in areas of high carbon dioxide concentration the curve shifts to the right, meaning it gives away oxygen more easily.
This means it can unload oxygen easier in capillaries and load more easily in alveoli.
Fetal haemoglobin has a higher affinity, so it will curve to the left. It does this by differing in two of the four polypeptide chains.
This is due to the fact it gets its oxygen from the mother’s blood, and therefore requires a fast intake to survive.
Different organisms have different oxygen conditions, therefore their graphs are different, for example:
Lugworms bury themselves in sand during high tides, an extremely low oxygen environment. They also have a low metabolic rate. Therefore, their curve is to the left of humans, and has a high affinity.
Llamas live on mountainous regions, so they need a higher affinity to take in the oxygen necessary for survival. This is to the left of humans but to the right of lugworms.
Carbon dioxide transport
Carbon dioxide travels in many forms:
5% as a solution in the plasma.
10% bound to haemoglobin as carbamino-haemoglobin.
85% as HCO3-, a hydrogen carbonate ion.
It is mostly converted to this ion inside the red blood cell, and then diffused out to plasma. This happens in 6 steps:
Carbon dioxide in the blood diffuses into a red blood cell.
The enzyme carbonic anhydrase catalyses the combination of carbon dioxide and water, which creates carbonic acid/H2CO3.
Carbonic acid then dissociates to a hydrogen ion and a hydrogen carbonate ion (H+ and HCO3-).
The HCO3- ions diffuse out of the red blood cell into the plasma.
In order for the cell to maintain it’s electrochemical neutrality, chloride ions then diffuse into the cell.
This movement is known as a chloride shift.
The H+ ions dissociate oxyhaemoglobin into oxygen and haemoglobin, as the H+ combines with haemoglobin to make haemoglobinic acid (HHb).
The H+ ions are removed, so the pH of the red blood cell doesn’t fall.
Oxygen then leaves the red blood cell via diffusion, where it enters the tissue fluid and then the cells.
This means that more HCO3- ions = more H+ ions, therefore explaining the Bohr effect as more carbon dioxide in red blood cells the more oxygen is released from haemoglobin.
Therefore, carbon dioxide is necessary to deliver oxygen to respiring tissues.
Tissue fluid
Blood cannot directly touch tissues, as blood vessels are closed systems. Therefore, tissue fluid is allows for the exchange of materials.
Capillaries have many features to support this diffusion:
Permeable.
Thin, for short diffusion pathway.
Large SA.
Lower blood pressure to give time for substance exchange.
Tissue fluid is extremely similar to plasma, except is does not contain the colloidal plasma proteins that lower the solute potential of plasma.
The exchanges occur through the use of hydrostatic pressure (the pressure of the blood pressing against the capillary wall) and the osmotic pressure (generated by the low solute potential in the plasma).
The exchange happens in two stages:
Ultra-filtration - Named as it filters out micromolecules, therefore the colloidal plasma proteins cannot leave as they are too big.
This is at the arterioles, therefore there is a high blood pressure, causing a high hydrostatic pressure which pushes tissue fluid out containing molecules cells need such as oxygen, glucose, amino acids, fatty acids, hormones and salts.
There is also an osmotic pressure, but the hydrostatic pressure is higher than this, causing molecules to keep leaving the blood.
Respiring tissues also have a lower concentration of these molecules, aiding the hydrostatic pressure in allowing these molecules out.
Absorption - Named as it absorbs waste products from the cells.
The volume of the blood is lowered via ultra-filtration and the friction of the capillary walls against the blood. This reduces blood pressure, and therefore hydrostatic pressure.
Less fluid means the colloidal plasma proteins are more concentrated, increasing osmotic pressure. This means osmotic pressure is stronger than hydrostatic pressure, pulling water back in.
The tissue fluid surrounding the cells picks up their waste products, such as carbon dioxide and urea, which is diffused into blood down a concentration gradient.
However, not all the tissue fluid returns to the blood. Around 10% drains into the blindly ending (dead end) lymph capillaries of the lymphatic system.
This mostly returns to the venous system via the thoracic duct, which empties into the subclavian vein above the heart.
There are two issues associated with this process:
Hypertension - Too high blood pressure.
The blood does not have enough time for absorption of waste materials.
This causes an accumulation of waste products and carbon dioxide, far beyond what the lymph capillaries can account for.
This causes oedema - a build up of this fluid which causes feet to swell.
Hypotension - Too low blood pressure.
Not enough ultra-filtration occurs, so nutrients are not received by cells.
This causes starvation of the cells, and increases the volume of blood, which can cause bloating.
 Knowt
Knowt