
Chapter 27: The Reproductive System
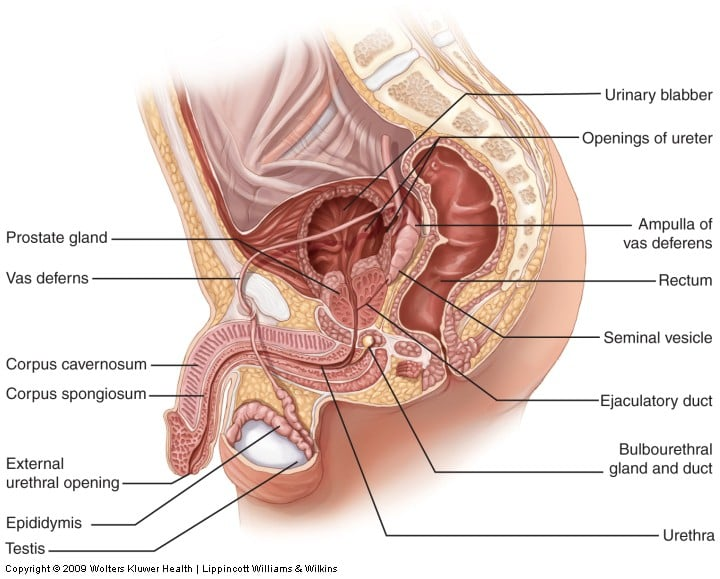
Anatomy and Physiology of the Male Reproductive System
Unique for its role in human reproduction, a gamete is a specialized sex cell carrying 23 chromosomes one half the number in body cells.
At fertilization, the chromosomes in one male gamete, called a sperm (or spermatozoon), combine with the chromosomes in one female gamete, called an oocyte.
Scrotum: The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis.
Testes
The testes (singular = testis) are the male gonads that is, the male reproductive organs. They produce both sperm and androgens, such as testosterone, and are active throughout the reproductive lifespan of the male.
The tightly coiled seminiferous tubules form the bulk of each testis.
Surrounding all stages of the developing sperm cells are elongate, branching Sertoli cells.
The least mature cells, the spermatogonia (singular = spermatogonium), line the basement membrane inside the tubule.
The process that begins with spermatogonia and concludes with the production of sperm is called spermatogenesis.
A process called spermiogenesis transforms these early spermatids, reducing the cytoplasm, and beginning the formation of the parts of a true sperm.
Role of the Epididymis: From the lumen of the seminiferous tubules, the immotile sperm are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed sperm continue to mature.
Duct System
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens).
The ductus deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord.
Sperm make up only 5 percent of the final volume of semen, the thick, milky fluid that the male ejaculates.
Seminal Vesicles: As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle.
Prostate Gland: The centrally located prostate gland sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra (the portion of the urethra that runs within the prostate).
Bulbourethral Glands: The final addition to semen is made by two bulbourethral glands (or Cowper’s glands) that release a thick, salty fluid that lubricates the end of the urethra and the vagina, and helps to clean urine residues from the penile urethra.
The Penis
The penis is the male organ of copulation (sexual intercourse).
Each of the two larger lateral chambers is called a corpus cavernosum (plural = corpora cavernosa).
The corpus spongiosum, which can be felt as a raised ridge on the erect penis, is a smaller chamber that surrounds the spongy, or penile, urethra.
The end of the penis, called the glans penis, has a high concentration of nerve endings, resulting in very sensitive skin that influences the likelihood of ejaculation.
The skin from the shaft extends down over the glans and forms a collar called the prepuce (or foreskin).
Testosterone: Testosterone, an androgen, is a steroid hormone produced by Leydig cells.
Anatomy and Physiology of the Female Reproductive System
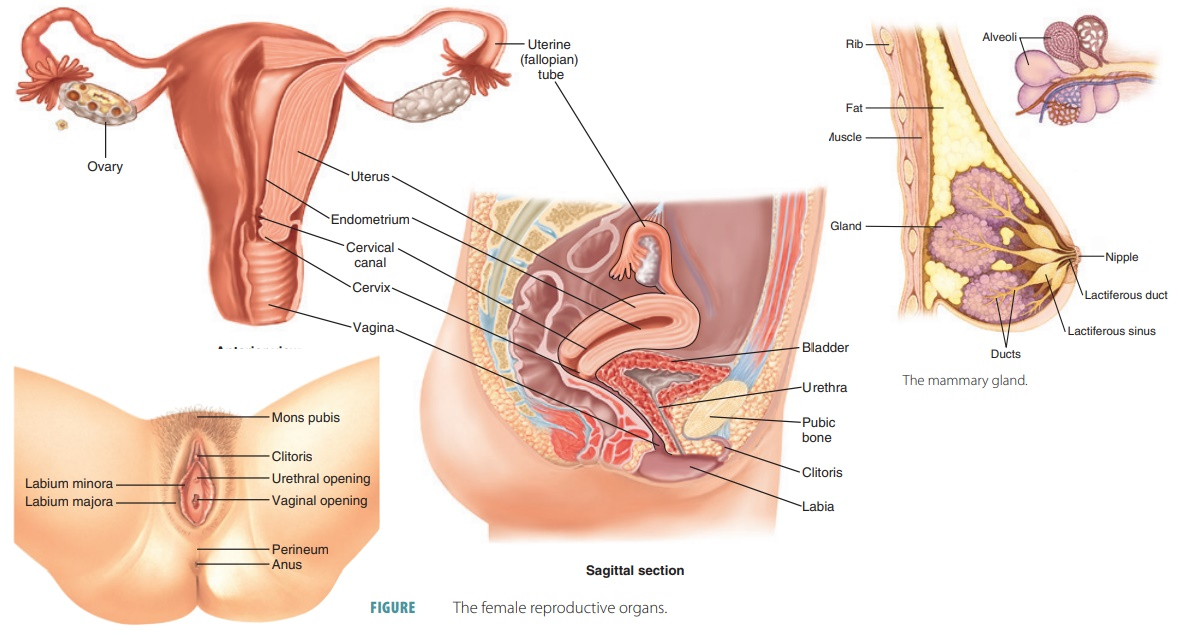
External Female Genitals
The external female reproductive structures are referred to collectively as the vulva.
The mons pubis is a pad of fat that is located at the anterior, over the pubic bone. After puberty, it becomes covered in pubic hair.
The labia majora (labia = “lips”; majora = “larger”) are folds of hair-covered skin that begin just posterior to the mons pubis.
The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) extend medial to the labia majora.
The hymen is a thin membrane that sometimes partially covers the entrance to the vagina.
It is flanked by outlets to the Bartholin’s glands (or greater vestibular glands).
Vagina
is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract.
The walls of the vagina are lined with an outer, fibrous adventitia; a middle layer of smooth muscle; and an inner mucous membrane with transverse folds called rugae.
Ovaries
The ovaries are the female gonads.
The ovaries are located within the pelvic cavity, and are supported by the mesovarium, an extension of the peritoneum that connects the ovaries to the broad ligament.
This grouping of an oocyte and its supporting cells is called a follicle.
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles.
Oogenesis
Gametogenesis in females is called oogenesis.
The process begins with the ovarian stem cells, or oogonia.
The initiation of ovulation, the release of an oocyte from the ovary marks the transition from puberty into reproductive maturity for women.
The smaller cell, called the first polar body, may or may not complete meiosis and produce second polar bodies; in either case, it eventually disintegrates.
Folliculogenesis
Ovarian follicles are oocytes and their supporting cells.
They grow and develop in a process called folliculogenesis, which typically leads to ovulation of one follicle approximately every 28 days, along with death to multiple other follicles.
Folliculogenesis begins with follicles in a resting state.
These small primordial follicles are present in newborn females and are the prevailing follicle type in the adult ovary
Primordial follicles have only a single flat layer of support cells, called granulosa cells, that surround the oocyte, and they can stay in this resting state for years—some until right before menopause.
After puberty, a few primordial follicles will respond to a recruitment signal each day, and will join a pool of immature growing follicles called primary follicles.
As the granulosa cells divide, the follicles now called secondary follicles increase in diameter, adding a new outer layer of connective tissue, blood vessels, and theca cells that work with the granulosa cells to produce estrogens.
A thick fluid, called follicular fluid, that has formed between the granulosa cells also begins to collect into one large pool, or antrum.
Follicles in which the antrum has become large and fully formed are considered tertiary follicles (or antral follicles).
The Uterine Tubes
The uterine tubes (also called fallopian tubes or oviducts) serve as the conduit of the oocyte from the ovary to the uterus.
The isthmus is the narrow medial end of each uterine tube that is connected to the uterus.
The wide distal infundibulum flares out with slender, finger-like projections called fimbriae.
The middle region of the tube, called the ampulla, is where fertilization often occurs.
The Uterus and Cervix
The uterus is the muscular organ that nourishes and supports the growing embryo.
The portion of the uterus superior to the opening of the uterine tubes is called the fundus.
The middle section of the uterus is called the body of uterus (or corpus). The cervix is the narrow inferior portion of the uterus that projects into the vagina.
The innermost layer of the uterus is called the endometrium.
The first menses after puberty, called menarche, can occur either before or after the first ovulation.
The Menstrual Cycle
The menstrual cycle is a natural process in female reproductive health that occurs approximately once a month.
During the menstrual cycle, hormones are released that cause the lining of the uterus to thicken in preparation for a potential pregnancy.
If no pregnancy occurs, the lining of the uterus is shed, resulting in a menstrual period.
The menstrual cycle usually lasts between 21 and 35 days and can vary in length and intensity from woman to woman.
Menses Phase: The menses phase of the menstrual cycle is the phase during which the lining is shed; that is, the days that the woman menstruates.
Proliferative Phase: Once menstrual flow ceases, the endometrium begins to proliferate again, marking the beginning of the proliferative phase of the menstrual cycle.
Secretory Phase: In the uterus, progesterone from the corpus luteum begins the secretory phase of the menstrual cycle, in which the endometrial lining prepares for implantation.
The Breasts
The external features of the breast include a nipple surrounded by a pigmented areola whose coloration may deepen during pregnancy.
Breast milk is produced by the mammary glands, which are modified sweat glands.
The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple.
Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.
Development of the Male and Female Reproductive Systems
In males, secretions from sustentacular cells trigger a degradation of the female duct, called the Müllerian duct.
At the same time, testosterone secretion stimulates growth of the male tract, the Wolffian duct.
Puberty is the stage of development at which individuals become sexually mature.
Development of the Secondary Sexual Characteristics
Male | Female |
|---|---|
Increased larynx size and deepening of the voice | Deposition of fat, predominantly in breasts and hips |
Increased muscular development | Breast development |
Growth of facial, axillary, and pubic hair, and increased growth of body hair | Broadening of the pelvis and growth of axillary and pubic hair |
Chapter 27: The Reproductive System
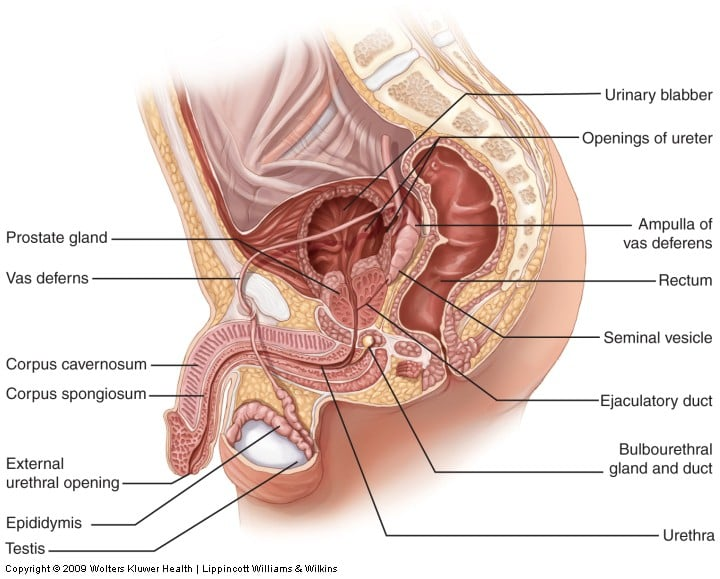
Anatomy and Physiology of the Male Reproductive System
Unique for its role in human reproduction, a gamete is a specialized sex cell carrying 23 chromosomes one half the number in body cells.
At fertilization, the chromosomes in one male gamete, called a sperm (or spermatozoon), combine with the chromosomes in one female gamete, called an oocyte.
Scrotum: The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis.
Testes
The testes (singular = testis) are the male gonads that is, the male reproductive organs. They produce both sperm and androgens, such as testosterone, and are active throughout the reproductive lifespan of the male.
The tightly coiled seminiferous tubules form the bulk of each testis.
Surrounding all stages of the developing sperm cells are elongate, branching Sertoli cells.
The least mature cells, the spermatogonia (singular = spermatogonium), line the basement membrane inside the tubule.
The process that begins with spermatogonia and concludes with the production of sperm is called spermatogenesis.
A process called spermiogenesis transforms these early spermatids, reducing the cytoplasm, and beginning the formation of the parts of a true sperm.
Role of the Epididymis: From the lumen of the seminiferous tubules, the immotile sperm are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed sperm continue to mature.
Duct System
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens).
The ductus deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord.
Sperm make up only 5 percent of the final volume of semen, the thick, milky fluid that the male ejaculates.
Seminal Vesicles: As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle.
Prostate Gland: The centrally located prostate gland sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra (the portion of the urethra that runs within the prostate).
Bulbourethral Glands: The final addition to semen is made by two bulbourethral glands (or Cowper’s glands) that release a thick, salty fluid that lubricates the end of the urethra and the vagina, and helps to clean urine residues from the penile urethra.
The Penis
The penis is the male organ of copulation (sexual intercourse).
Each of the two larger lateral chambers is called a corpus cavernosum (plural = corpora cavernosa).
The corpus spongiosum, which can be felt as a raised ridge on the erect penis, is a smaller chamber that surrounds the spongy, or penile, urethra.
The end of the penis, called the glans penis, has a high concentration of nerve endings, resulting in very sensitive skin that influences the likelihood of ejaculation.
The skin from the shaft extends down over the glans and forms a collar called the prepuce (or foreskin).
Testosterone: Testosterone, an androgen, is a steroid hormone produced by Leydig cells.
Anatomy and Physiology of the Female Reproductive System
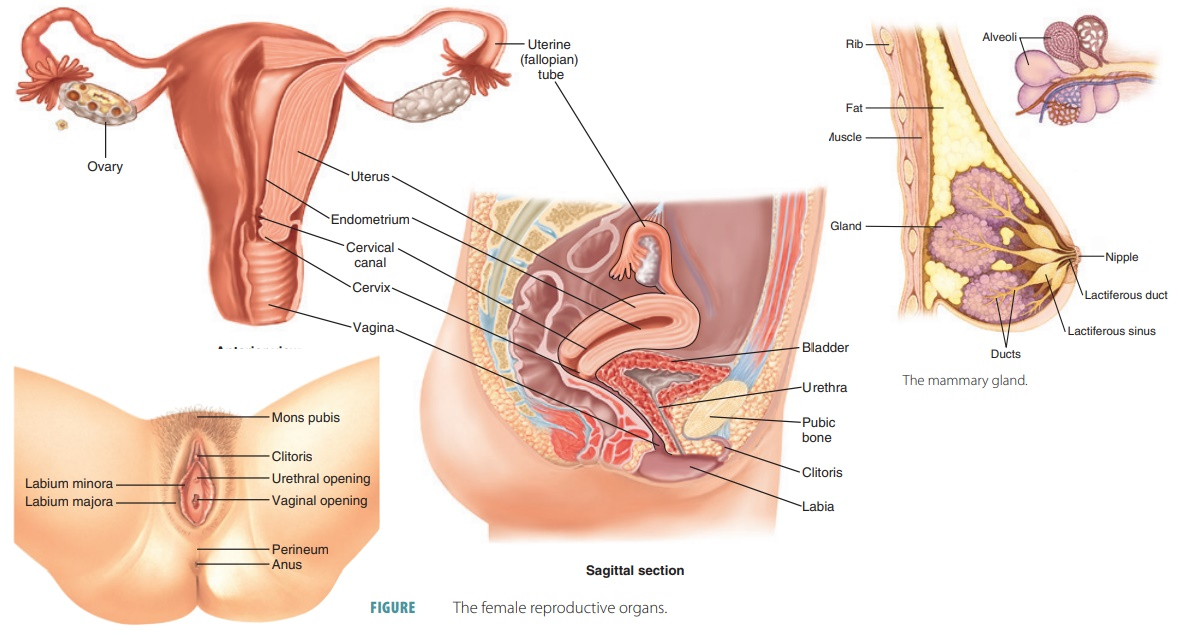
External Female Genitals
The external female reproductive structures are referred to collectively as the vulva.
The mons pubis is a pad of fat that is located at the anterior, over the pubic bone. After puberty, it becomes covered in pubic hair.
The labia majora (labia = “lips”; majora = “larger”) are folds of hair-covered skin that begin just posterior to the mons pubis.
The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) extend medial to the labia majora.
The hymen is a thin membrane that sometimes partially covers the entrance to the vagina.
It is flanked by outlets to the Bartholin’s glands (or greater vestibular glands).
Vagina
is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract.
The walls of the vagina are lined with an outer, fibrous adventitia; a middle layer of smooth muscle; and an inner mucous membrane with transverse folds called rugae.
Ovaries
The ovaries are the female gonads.
The ovaries are located within the pelvic cavity, and are supported by the mesovarium, an extension of the peritoneum that connects the ovaries to the broad ligament.
This grouping of an oocyte and its supporting cells is called a follicle.
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles.
Oogenesis
Gametogenesis in females is called oogenesis.
The process begins with the ovarian stem cells, or oogonia.
The initiation of ovulation, the release of an oocyte from the ovary marks the transition from puberty into reproductive maturity for women.
The smaller cell, called the first polar body, may or may not complete meiosis and produce second polar bodies; in either case, it eventually disintegrates.
Folliculogenesis
Ovarian follicles are oocytes and their supporting cells.
They grow and develop in a process called folliculogenesis, which typically leads to ovulation of one follicle approximately every 28 days, along with death to multiple other follicles.
Folliculogenesis begins with follicles in a resting state.
These small primordial follicles are present in newborn females and are the prevailing follicle type in the adult ovary
Primordial follicles have only a single flat layer of support cells, called granulosa cells, that surround the oocyte, and they can stay in this resting state for years—some until right before menopause.
After puberty, a few primordial follicles will respond to a recruitment signal each day, and will join a pool of immature growing follicles called primary follicles.
As the granulosa cells divide, the follicles now called secondary follicles increase in diameter, adding a new outer layer of connective tissue, blood vessels, and theca cells that work with the granulosa cells to produce estrogens.
A thick fluid, called follicular fluid, that has formed between the granulosa cells also begins to collect into one large pool, or antrum.
Follicles in which the antrum has become large and fully formed are considered tertiary follicles (or antral follicles).
The Uterine Tubes
The uterine tubes (also called fallopian tubes or oviducts) serve as the conduit of the oocyte from the ovary to the uterus.
The isthmus is the narrow medial end of each uterine tube that is connected to the uterus.
The wide distal infundibulum flares out with slender, finger-like projections called fimbriae.
The middle region of the tube, called the ampulla, is where fertilization often occurs.
The Uterus and Cervix
The uterus is the muscular organ that nourishes and supports the growing embryo.
The portion of the uterus superior to the opening of the uterine tubes is called the fundus.
The middle section of the uterus is called the body of uterus (or corpus). The cervix is the narrow inferior portion of the uterus that projects into the vagina.
The innermost layer of the uterus is called the endometrium.
The first menses after puberty, called menarche, can occur either before or after the first ovulation.
The Menstrual Cycle
The menstrual cycle is a natural process in female reproductive health that occurs approximately once a month.
During the menstrual cycle, hormones are released that cause the lining of the uterus to thicken in preparation for a potential pregnancy.
If no pregnancy occurs, the lining of the uterus is shed, resulting in a menstrual period.
The menstrual cycle usually lasts between 21 and 35 days and can vary in length and intensity from woman to woman.
Menses Phase: The menses phase of the menstrual cycle is the phase during which the lining is shed; that is, the days that the woman menstruates.
Proliferative Phase: Once menstrual flow ceases, the endometrium begins to proliferate again, marking the beginning of the proliferative phase of the menstrual cycle.
Secretory Phase: In the uterus, progesterone from the corpus luteum begins the secretory phase of the menstrual cycle, in which the endometrial lining prepares for implantation.
The Breasts
The external features of the breast include a nipple surrounded by a pigmented areola whose coloration may deepen during pregnancy.
Breast milk is produced by the mammary glands, which are modified sweat glands.
The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple.
Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.
Development of the Male and Female Reproductive Systems
In males, secretions from sustentacular cells trigger a degradation of the female duct, called the Müllerian duct.
At the same time, testosterone secretion stimulates growth of the male tract, the Wolffian duct.
Puberty is the stage of development at which individuals become sexually mature.
Development of the Secondary Sexual Characteristics
Male | Female |
|---|---|
Increased larynx size and deepening of the voice | Deposition of fat, predominantly in breasts and hips |
Increased muscular development | Breast development |
Growth of facial, axillary, and pubic hair, and increased growth of body hair | Broadening of the pelvis and growth of axillary and pubic hair |
 Knowt
Knowt
