
Abnormal Psychology
I. Anxiety Disorders
GAD: Generalized anxiety disorder
- Emotional-cognitive symptoms: Worrying, having anxious feelings about many subjects, and sometimes “free-floating” anxiety with no attachment to any subject. Anxious anticipation interferes with concentration.
- Physical symptoms: Autonomic arousal, trembling, sweating, fidgeting, agitation, and sleep disruption.
Diagnostic Criteria:
Excessive anxiety and worry, occurring more days than not for at least 6 months, about a number of events or activities.
The individual finds it difficult to control the worry.
The anxiety and worry are associated with three of the following six symptoms (present for more days than not for the past 6 months).
Restlessness, feeling keyed up or on edge.
Being easily fatigued
Difficulty concentrating or mind going blank.
Irritability.
Muscle tension.
Sleep disturbanc.
The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The disturbance is not attributable to the physiological effects of a substance or another medical condition.
The disturbance is not better explained by another medical disorder.
Panic disorder “I’m Dying”
- A panic attack may include many minutes of intense dread or terror, chest pains, choking, numbness, or other frightening physical sensations, and a feeling of a need to escape.
- Panic disorder refers to repeated and unexpected panic attacks, as well as a fear of the next attack, and a change in behavior to avoid panic attacks.
Phobias
- A specific phobia is more than just a strong fear or dislike. A specific phobia is diagnosed when there is an uncontrollable, irrational, intense desire to avoid some object or situation. Even an image of the object can trigger a reaction.
- Symptoms may include sweating, chest pains, and pins and needles.
- Behavioral therapy and medication for treatment.
- 19 million people in the US.
- It is believed that phobias are mostly learned either from watching parents exhibit the fear or through a traumatic experience
- Exposure Therapy can help people with a phobia alter their response to the source of fear. They are gradually exposed to the cause of their phobia over a series of escalating steps.
OCD: Obsessive-compulsive disorder
- Obsessions are intense, unwanted worries, ideas, and images that repeatedly pop up in the mind.
- A compulsion is a repeatedly strong feeling of “needing” to carry out an action, even though it doesn’t feel like it makes sense.
PTSD: Post-traumatic stress disorder
- 10 to 35 percent of people who experience trauma.
- Repeated intrusive recall of those memories, nightmares and other re-experiencing, social withdrawal; phobic avoidance, jumpy anxiety or hypervigilance, and insomnia or sleep problems.
- People with less control in the situation, traumatized more frequently, have brain differences, and less resiliency, and the ones who get re-traumatized get PTSD.
II. Mood Disorders
Major Depressive Disorders
- Symptoms must be present for more than 2 weeks.
Depressed mood most of the day
Markedly diminished interest or pleasure in activities
Significant increase or decrease in appetite or weight
Insomnia, sleeping too much, or disrupted sleep
Lethargy, or physical agitation
Fatigue or loss of energy nearly every day
Worthlessness, or excessive/inappropiate guilt
Daily problems in thinking, concentrating, and/or making decisions
Recurring thoughts of death and suicide
- Depressive episodes happen to 6 percent of men and 9 percent of women yearly.
Seasonal Affective Disorder
- SAD involves a recurring seasonal pattern of depression, usually during winter’s short, dark, cold days.
- More common in women.
Bipolar Disorder
- Once called “manic-depressive disorder.”
- Two polar opposite moods are depression and mania.
- Mania refers to a period of hyper-elevated mood that is euphoric, giddy, easily irritated, hyperactive, impulsive, overly optimistic, and grandiose.
- Bipolar I and Bipolar II (Mania and hypomania)
Suicide and Self-Injury
- Every year, 1 million people commit suicide.
- Can happen when people feel frustrated, trapped, isolated, and ineffective, and see no end to these feelings.
- Non-suicidal self-injury has other functions such as sending a message, or self-punishment.
- Brain activity is diminished in depression and increased in mania.
- Brain structure: smaller frontal lobes in depression and fewer axons in bipolar disorder.
- More arousal in mania, less in depression.
- Reduced serotonin in depression.
- Treat depression with exercise to increase serotonin levels.
- Reduce brain inflammation with a healthy diet. (olive and fish oils)
- Depression is associated with low self-esteem, learned helplessness, depressive explanatory style, and rumination (stuck focusing on what’s bad).
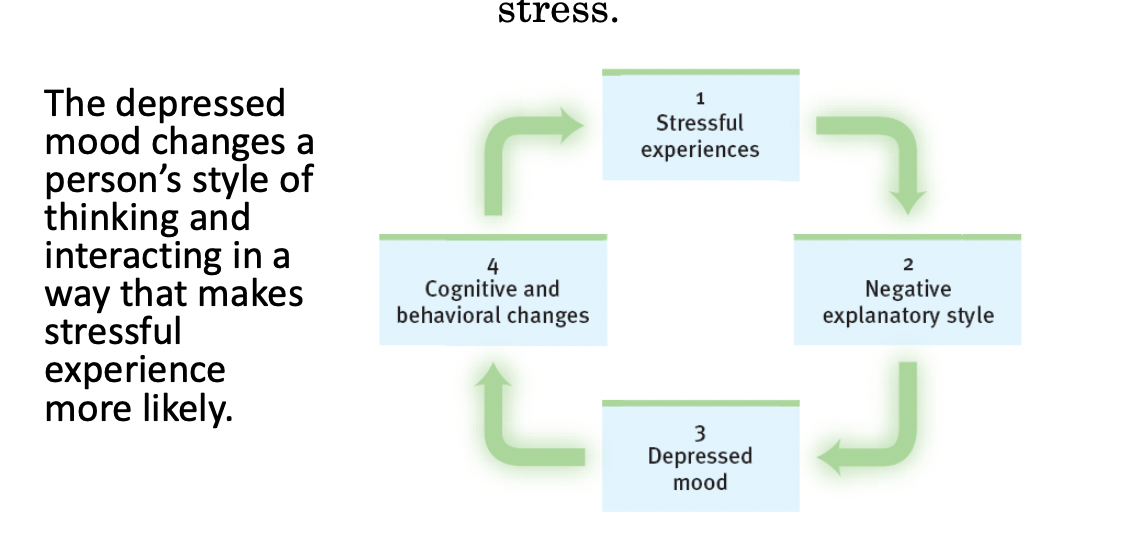
- Depression’s Vicious Cycle:
III. Schizophrenia
- Schizophrenia: The mind is split from reality, a split from one’s own thoughts so that they appear as hallucinations.
- Psychosis refers to a mental split between reality and rationality.
- Schizophrenia symptoms include:
Disorganized and/or delusional thinking.
Disturbed perceptions.
Inappropiate emotions and actions.
Positive symptoms:
Hallucinations
Delusions
Disorganized thought and nonsencical speech
Bizarre behaviors
Negative symptoms:
Flat effect (no emotion showing in the face)
Reduced social interaction
Anhedonia (no feeling of enjoyment)
Avolition (less motivation, initiative, focus on tasks)
Alogia (speaking less)
Catatonia (moving less)
- Schizophrenic symptoms appear at the end of adolescence and in early adulthood, later for women than for men.
- 1 in a 100
- Likely to develop when:
Low birth weight
Maternal diabetes
Older paternal age
Famine
Oxygen deprivation during delivery
Maternal virus during mid-pregnancy impairing brain development.
- Dopamine/D4 receptors explain paranoia and hallucinations.
IV: Dissociative Identity Disorder
- Previously: Multiple personality disorder.
- A key element to diagnosis is the presence of at least two distinct and separate personalities within an individual.
- The personalities are called alters, and only one is manifested at a time, each with its own memories, behaviors, and life preferences.
- Common symptoms:
Inability to recall large memories of childhood.
Lack of awareness of recent event.
Flashbacks or sudden return of memories.
Feelings of disconection or detachment from body or thoughts.
Hallucinations or voices
Self-harm or suicidal thoughts
Changes in handwriting.
Functional changes: from nearly disabled to highly functioning.
- Develops to cope with severe and prolonged trauma.
- 1.9% of the population.
- Women are 3x likely to be diagnosed (women in their 30s)
- Treatment is integrated functioning (trying to integrate all the personalities into 1 whole being, a state where all identities can harmoniously coexist.)
Establish safety
Confronting
Integration and rehabilitation
V: Personality disorders
Paranoid Personality Disorder
- Unjustified suspicions that others are trying to harm them.
- Hesitancy to confide in others.
- Tendency to hold grudges.
Antisocial Personality Disorder
- No regard for right or wrong.
- Impulsive behavior.
- Lack of remorse.
- Irresponsible.
Borderline Personality Disorder
- Fear of abandonment
- Difficulty with social relationships
- Loss of contact with reality.
Narcissistic Personality Disorder
- Need and seek too much attention
- Center of attention
Obsessive Compulsive Personality Disorder
- Preoccupation with control
- Perfectionism
- Extreme attention to detail
Avoidant Personality Disorder
- Social inhibition
- Avoid social situations
- Fear of being criticized.
Abnormal Psychology
I. Anxiety Disorders
GAD: Generalized anxiety disorder
- Emotional-cognitive symptoms: Worrying, having anxious feelings about many subjects, and sometimes “free-floating” anxiety with no attachment to any subject. Anxious anticipation interferes with concentration.
- Physical symptoms: Autonomic arousal, trembling, sweating, fidgeting, agitation, and sleep disruption.
Diagnostic Criteria:
Excessive anxiety and worry, occurring more days than not for at least 6 months, about a number of events or activities.
The individual finds it difficult to control the worry.
The anxiety and worry are associated with three of the following six symptoms (present for more days than not for the past 6 months).
Restlessness, feeling keyed up or on edge.
Being easily fatigued
Difficulty concentrating or mind going blank.
Irritability.
Muscle tension.
Sleep disturbanc.
The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The disturbance is not attributable to the physiological effects of a substance or another medical condition.
The disturbance is not better explained by another medical disorder.
Panic disorder “I’m Dying”
- A panic attack may include many minutes of intense dread or terror, chest pains, choking, numbness, or other frightening physical sensations, and a feeling of a need to escape.
- Panic disorder refers to repeated and unexpected panic attacks, as well as a fear of the next attack, and a change in behavior to avoid panic attacks.
Phobias
- A specific phobia is more than just a strong fear or dislike. A specific phobia is diagnosed when there is an uncontrollable, irrational, intense desire to avoid some object or situation. Even an image of the object can trigger a reaction.
- Symptoms may include sweating, chest pains, and pins and needles.
- Behavioral therapy and medication for treatment.
- 19 million people in the US.
- It is believed that phobias are mostly learned either from watching parents exhibit the fear or through a traumatic experience
- Exposure Therapy can help people with a phobia alter their response to the source of fear. They are gradually exposed to the cause of their phobia over a series of escalating steps.
OCD: Obsessive-compulsive disorder
- Obsessions are intense, unwanted worries, ideas, and images that repeatedly pop up in the mind.
- A compulsion is a repeatedly strong feeling of “needing” to carry out an action, even though it doesn’t feel like it makes sense.
PTSD: Post-traumatic stress disorder
- 10 to 35 percent of people who experience trauma.
- Repeated intrusive recall of those memories, nightmares and other re-experiencing, social withdrawal; phobic avoidance, jumpy anxiety or hypervigilance, and insomnia or sleep problems.
- People with less control in the situation, traumatized more frequently, have brain differences, and less resiliency, and the ones who get re-traumatized get PTSD.
II. Mood Disorders
Major Depressive Disorders
- Symptoms must be present for more than 2 weeks.
Depressed mood most of the day
Markedly diminished interest or pleasure in activities
Significant increase or decrease in appetite or weight
Insomnia, sleeping too much, or disrupted sleep
Lethargy, or physical agitation
Fatigue or loss of energy nearly every day
Worthlessness, or excessive/inappropiate guilt
Daily problems in thinking, concentrating, and/or making decisions
Recurring thoughts of death and suicide
- Depressive episodes happen to 6 percent of men and 9 percent of women yearly.
Seasonal Affective Disorder
- SAD involves a recurring seasonal pattern of depression, usually during winter’s short, dark, cold days.
- More common in women.
Bipolar Disorder
- Once called “manic-depressive disorder.”
- Two polar opposite moods are depression and mania.
- Mania refers to a period of hyper-elevated mood that is euphoric, giddy, easily irritated, hyperactive, impulsive, overly optimistic, and grandiose.
- Bipolar I and Bipolar II (Mania and hypomania)
Suicide and Self-Injury
- Every year, 1 million people commit suicide.
- Can happen when people feel frustrated, trapped, isolated, and ineffective, and see no end to these feelings.
- Non-suicidal self-injury has other functions such as sending a message, or self-punishment.
- Brain activity is diminished in depression and increased in mania.
- Brain structure: smaller frontal lobes in depression and fewer axons in bipolar disorder.
- More arousal in mania, less in depression.
- Reduced serotonin in depression.
- Treat depression with exercise to increase serotonin levels.
- Reduce brain inflammation with a healthy diet. (olive and fish oils)
- Depression is associated with low self-esteem, learned helplessness, depressive explanatory style, and rumination (stuck focusing on what’s bad).
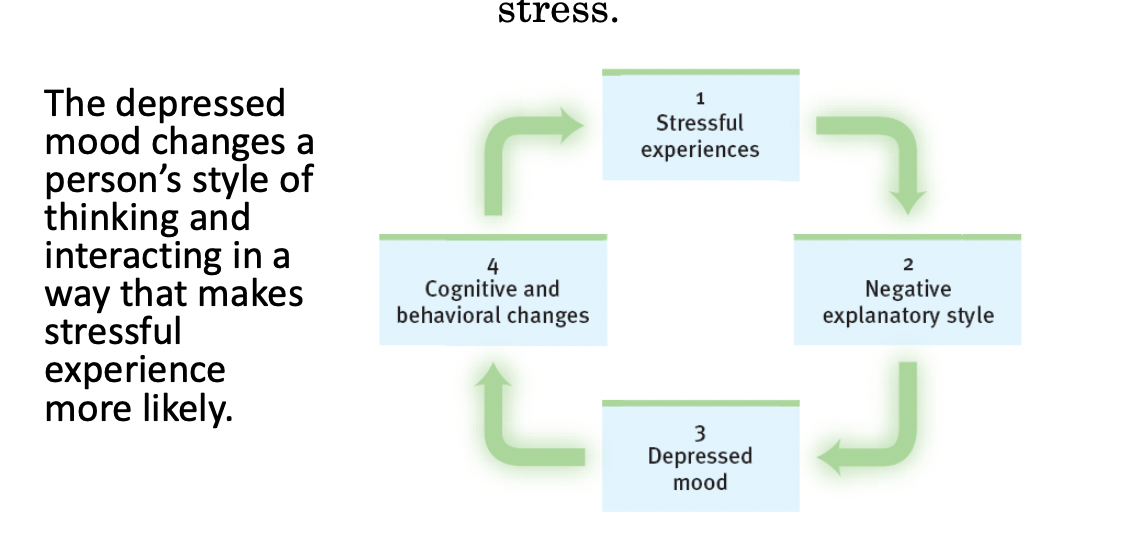
- Depression’s Vicious Cycle:
III. Schizophrenia
- Schizophrenia: The mind is split from reality, a split from one’s own thoughts so that they appear as hallucinations.
- Psychosis refers to a mental split between reality and rationality.
- Schizophrenia symptoms include:
Disorganized and/or delusional thinking.
Disturbed perceptions.
Inappropiate emotions and actions.
Positive symptoms:
Hallucinations
Delusions
Disorganized thought and nonsencical speech
Bizarre behaviors
Negative symptoms:
Flat effect (no emotion showing in the face)
Reduced social interaction
Anhedonia (no feeling of enjoyment)
Avolition (less motivation, initiative, focus on tasks)
Alogia (speaking less)
Catatonia (moving less)
- Schizophrenic symptoms appear at the end of adolescence and in early adulthood, later for women than for men.
- 1 in a 100
- Likely to develop when:
Low birth weight
Maternal diabetes
Older paternal age
Famine
Oxygen deprivation during delivery
Maternal virus during mid-pregnancy impairing brain development.
- Dopamine/D4 receptors explain paranoia and hallucinations.
IV: Dissociative Identity Disorder
- Previously: Multiple personality disorder.
- A key element to diagnosis is the presence of at least two distinct and separate personalities within an individual.
- The personalities are called alters, and only one is manifested at a time, each with its own memories, behaviors, and life preferences.
- Common symptoms:
Inability to recall large memories of childhood.
Lack of awareness of recent event.
Flashbacks or sudden return of memories.
Feelings of disconection or detachment from body or thoughts.
Hallucinations or voices
Self-harm or suicidal thoughts
Changes in handwriting.
Functional changes: from nearly disabled to highly functioning.
- Develops to cope with severe and prolonged trauma.
- 1.9% of the population.
- Women are 3x likely to be diagnosed (women in their 30s)
- Treatment is integrated functioning (trying to integrate all the personalities into 1 whole being, a state where all identities can harmoniously coexist.)
Establish safety
Confronting
Integration and rehabilitation
V: Personality disorders
Paranoid Personality Disorder
- Unjustified suspicions that others are trying to harm them.
- Hesitancy to confide in others.
- Tendency to hold grudges.
Antisocial Personality Disorder
- No regard for right or wrong.
- Impulsive behavior.
- Lack of remorse.
- Irresponsible.
Borderline Personality Disorder
- Fear of abandonment
- Difficulty with social relationships
- Loss of contact with reality.
Narcissistic Personality Disorder
- Need and seek too much attention
- Center of attention
Obsessive Compulsive Personality Disorder
- Preoccupation with control
- Perfectionism
- Extreme attention to detail
Avoidant Personality Disorder
- Social inhibition
- Avoid social situations
- Fear of being criticized.
 Knowt
Knowt